Superficial Back and Scapular Area
The back forms the posterior aspect of the trunk over the thorax, abdomen, and pelvis. The posterior part of the neck is included for descriptive purposes. The back is an important musculoskeletal region functionally related to both the upper and lower limbs. The vertebral column is located in the midline of the back, where it is covered superficially by muscles, fat and other fascia, and skin. The vertebral column is the anchor of the axial skeleton—formed by the vertebral column, skull, hyoid bone, ribs and sternum—and also encloses and protects the spinal cord. The appendicular skeletons of the upper and lower limbs form joints (articulations) with the axial skeleton, and some proximal limb muscles attach to it. The back is traditionally studied with the upper limb because of their close functional relationship.
The back will be dissected during three lab periods, the first two of which are scheduled this semester. This period is devoted to studying the superficial back and scapular area. The deep back dissection will be performed during the next lab period. Next semester the vertebral canal will be opened to expose the spinal cord during the third back lab.
SKELETAL LANDMARKS
The cadaver must be placed in the prone (face down) position for this dissection.
1. Identification of bony landmarks on a skeleton and their palpation on the cadaver will facilitate the dissection. On the skull identify the external occipital protuberance [R201.12] and superior nuchal lines of the occipital bone and the mastoid process of the temporal bone (G11 7.2, 7.3; G12 7.3A-B, 7.4A,B,C,D; N6, 10) [R29.20]. Now find the second sacral vertebra (Sv2), which is located at the level of the posterior superior iliac spines (G11 3.3D-F, 4.22, 4.27; G12 3.7A, 3.1A, 3.2A, 3.7B, 3.1B, 3.2B, 4.25A-B, 4.30; N149, 155A-B). Study the parts of a typical vertebra [R191]: an anterior cylindrical body and a posterior vertebral arch consisting of two pedicles, two laminae, two transverse processes, two superior and two inferior articular processes, and a spinous process (G11 4.4; G12 4.4A-B; N151A,B,C,D, 152A,B,C,D). Examine the spinous processes of the vertebrae between the external occipital protuberance and Sv2, paying particular attention to the long spinous process of Cv7, the vertebra prominens (G11 1.9B, 4.1, 4.3, 4.9B & D, 8.2F; G12 1.9B, 4.1, 4.3A,B,C, 4.10B, 4.11B, 8.4B; N22, 149, 150). Find the inferior angle, glenoid cavity, acromion and spine of the scapula (G11 6.1, 6. 31; [note that the labels for “Acromion” and “Spine of scapula” have been transposed in 6.1B] G12 6.1A-B, 6.31A,B,C,D,E; N179A-B [Posterior view], 408A-B). Palpate these landmarks on the prone cadaver.
In the superficial back dissection we study muscles that “migrated” into the back during embryonic development. These muscles are essential for movements of the upper limb and assist in movements of the neck. Thus, injury or paralysis of the superficial back muscles results in significant deficits in upper extremity movements. During this dissection, focus attention on where these muscles are attached and the orientations of their muscle fibers. This will aid in understanding how each muscle functions and the potential deficits that may result from the loss of its function.
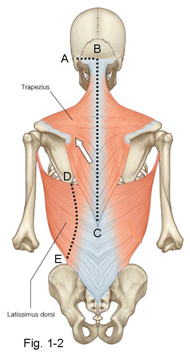
The superficial muscles of the back are extrinsic back muscles that connect the upper limb to the vertebral column and help control upper limb movements. They migrated into the back during development, carrying their innervation from the anterior rami of spinal nerves (G11 1.18, 4.46B-C; G12 1.18, 4.49A; N162A-B, 163A-B, 174, 185, 252). These extrinsic back muscles are arranged in layers. The first layer comprises the trapezius and latissimus dorsi, and the second layer is formed by the levator scapulae, rhomboid major, and rhomboid minor (Fig. 1-2; G11 4.27, 4.28, 4.29; G12 4.30, 4.31, 4.32; N149, 168, 411A-B [Posterior view]).
The trapezius takes origin from the external occipital protuberance and superior nuchal line, nuchal ligament, and spinous processes of vertebraeTv1-Tv12. Distally it attaches to the lateral 1/3 of the clavicle, acromion, and spine of the scapula. Given these extensive attachments, it isn’t surprising that the upper, middle, and lower thirds of the trapezius (G11 4.27, 4.28; Table 6.4 [p. 496]; G12 4.30, 4.31; N168, 411A-B) may act with some degree of independence to produce elevation, retraction (adduction), and depression of the scapula, respectively. The descending fibers of the upper part hold up the point of the shoulder in its normal postural position. The upper and lower parts act together to upwardly rotate the glenoid cavity of the scapula, which is necessary to raise the arm above a horizontal plane.
The trapezius is unique among the back muscles in that it receives its motor innervation from a cranial nerve, the accessory nerve (CNXI) (G11 4.28, 6.27A, 8.3A-C, Table 9.13 [p. 820]; G12 4.31, 6.39A, 8.5A,D,E,F, Table 9.13 [p. 838]; N31, 126, 171). The trapezius also receives proprioceptive and pain fibers from the anterior rami of spinal nerves C3 and C4. A lesion of the accessory nerve results in inability to shrug the shoulder and difficulty raising the arm above the horizontal level. Paralysis of the trapezius muscle allows the shoulder to droop (e.g., in many stroke patients), predisposing to subluxation (partial dislocation) of the shoulder joint. Iatrogenic injury of the accessory nerve is common during surgery of the posterior triangle of the neck.
The latissimus dorsi muscle attaches proximally to the lower 6 thoracic vertebrae, lumbar vertebrae, and sacral vertebrae via thoracolumbar fascia and to the iliac crest (Fig. 1-2; G11 4.27, 4.28; Table 6.4 [p. 496]; G12 4.30, 4.31; N168, 173, 248A-B). It is a broad triangular muscle that tapers to a band-like tendon, which inserts into the intertubercular (bicipital) groove of the humerus. The latissimus dorsi extends, adducts, and medially rotates the arm. If the humerus is fixed in position by other muscles, the latissimus draws the trunk upward toward it (e.g., doing chin-ups). The latissimus dorsi is important clinically because it can act through the humerus to depress the shoulder, lifting the body when walking with axillary crutches or when moving oneself into or from a wheelchair (wheelchair transfer). The latissimus dorsi is innervated by the thoracodorsal (middle subscapular) nerve, a branch of the brachial plexus which will be seen during dissection of the axilla (G11 6.23, 6.24, 6.25; G12 6.24, 6.25A-B, 6.27; N412, 417).
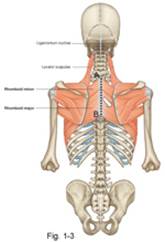
The second layer of extrinsic back muscles lies deep to the trapezius. It is formed by the levator scapulae, rhomboid major, and rhomboid minor (Fig. 1-3; G11 4.28, 4.29; Table 6.4 [p. 496]; G12 4.31, 4.32; N168, 411A-B). The levator scapulae is a strap-like muscle that attaches proximally to the transverse processes of the upper four cervical vertebrae. It descends slightly laterally to attach to the vertebral (medial) border of the scapula superior to its spine. The levator scapulae elevates the scapula and helps to rotate the glenoid cavity downward (e.g., when depressing the shoulder to reach down and pick up a suitcase). It is innervated by the dorsal scapular nerve (C5) and cervical spinal nerves 3 and 4 (C3,4).
The rhomboid major and rhomboid minor muscles frequently are fused and are identified by location and attachments (Fig. 1-3; G11 4.28, 4.29; G12 4.31, 4.32; N168, 171, 411A-B). The rhomboid minor is the upper muscle of the two, taking origin from the lower part of the nuchal ligament (ligamentum nuchae) and the spinous processes of Cv7 and Tv1. It passes inferolaterally to insert into the vertebral border of the scapula at the level of its spine (G11 6.31D; G12 6.31E; N408A-B). The larger rhomboid major passes from the spinous processes of Tv2-Tv5 to insert into the vertebral border of the scapula inferior to its spine. The rhomboid muscles act together to retract (adduct) the scapula. They act with the levator scapulae to downwardly rotate the glenoid cavity. The rhomboid muscles are innervated by the dorsal scapular nerve (N465).
The skin of the back is a tough, leathery layer easily distinguished from the underlying loose subcutaneous connective tissue (superficial fascia), which contains a variable amount of fat. The fat may appear brownish-tan, bright yellow, or almost white in color.
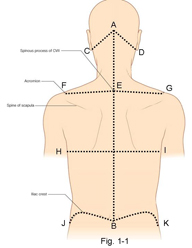
2. Make an incision through only the skin of the back (≈ 6mm thick in places) down the midline, along the tips of the spinous processes of vertebrae, from the external occipital protuberance above to the level of Sv2 below (Fig. 1-1, A-B).
3. From the initial midsagittal incision, make four transverse incisions through the skin on each side:
►Between the external occiSpital protuberance and the mastoid process (Fig. 1-1, A-C and A-D).
►From the spinous process of Cv7 (vertebra prominens, E) along the top of the shoulder to the bony point of the shoulder (acromion of the scapula) (Fig. 1-1 E-F and E-G).
►Transversely at the level of the inferior angle of the scapula to the posterior axillary fold (G11 1.1, 6.14; G12 1.1, 6.14) (Fig. 1-1, H-I).
►From the median sacral crest at Sv2 along the iliac crest to the level of the posterior axillary fold (Fig. 1-1 B-J and B-K).
4. Reflect a small square of skin (≈10 cm by 10 cm) laterally on one side, starting at the edge of a flap, and leaving the superficial fascia in place. When done correctly, the deep surface of the reflected skin has a pitted appearance somewhat resembling an orange peel. This practice will become important in dissecting areas, such as the dorsum of the hand, where the skin is thin and subcutaneous structures are easily damaged.
5. Now deepen the original cuts from the skin down through superficial fascia but DO NOT CUT INTO THE UNDERLYING MUSCLES! Reflect the remaining skin and the superficial fascia en bloc and clean the exposed back muscles. The best result in reflecting the skin and fascia is produced by maintaining steady traction as they are being reflected. Traction can be obtained by making a small incision in the skin flap and placing a finger through this “button hole.” At the end of the lab period, we will spray the cadaver with wetting solution and replace the skin flaps in position to cover the dissection. This helps to maintain the dissected tissues in good condition.
6. Attempt to find the cut ends of a few of the cutaneous nerves (G11 4.28, 4.33, 4.34; G12 4.31, 4.36, 4.37; N163A-B, 171, 252), which arise from the posterior rami of spinal nerves and pierce the back muscles (G11 1.18, 4.46B-C; G12 1.18, 4.49A; N171, 252) [R226.4; 226.8]. The cutaneous nerves in the lower thoracic and lumbar regions of the back are located farther from the midline than the more superior nerves. That’s because the more inferior cutaneous nerves arise from the lateral branches of posterior rami [R226.4] instead of from the medial branches [R226.4]. Don’t spend a lot of time looking for cutaneous nerves now since we will see better examples in the upper extremity. Carefully remove the thin layer of deep fascia (epimysium) from the surface of the exposed back muscles.
All dissections will be performed on both sides of the body unless otherwise indicated.
7. Identify the trapezius [R226.3] and latissimus dorsi [R226.7] muscles (G11 4.28, 6.29, Table 6.4; G12 4.31, 6.29; N168, 411A-B). Study the triangle of auscultation [R226] bounded superiorly by the trapezius, inferiorly by the latissimus dorsi, and laterally by the rhomboid major muscle and scapula. It is a good place to position a stethoscope to listen to posterior segments of the lungs (auscultation) through the sixth intercostal space.
8. Clean the proximal attachment of the trapezius to the skull, nuchal ligament, and spinous processes of vertebrae Tv1-Tv12. Trace the muscle to its distal attachment on the clavicle, acromion, and spine of the scapula (G11 8.3A; G12 8.5A; N407A-B, 408A-B, 411A-B). Carefully clean the length of the upper free border of the muscle so as not to damage structures in the posterior triangle of the neck (lateral cervical region), for which the trapezius forms the posterior boundary (G11 8.3A, Tables 8.2, 8.3 [pp. 724-725]; G12 8.5A, Table 8.3A,B,C [p. 753]; N26, 182).
9. Cut the attachment of the trapezius from the superior nuchal line and external occipital protuberance (Fig. 1-2, A-B).
10. Make a vertical incision 2.5 cm (about 1 inch) lateral to the spinous processes of vertebrae along the entire length of the trapezius (Fig. 1-2, B-C). The muscle varies substantially in thickness among cadavers, so be careful not to cut too deeply if the muscle is thin in your cadaver. Carefully reflect the trapezius laterally toward the scapula, starting inferiorly at Tv12 and continuing upward (Fig. 1-2, direction of white arrow). After the upper third of the trapezius is reflected, identify the accessory nerve (CNXI) [R235.11] and superficial branch of the transverse cervical artery [R235.13] on its deep surface (G11 4.28, 6.27A, 8.3B; G12 4.31, 6.39A, 8.5A,B,C,D,E,F; N171). These are the major nerve and artery supplying the trapezius.
11. Clean the attachment of the latissimus dorsi along the lower 6 thoracic vertebrae, lumbar vertebrae, and iliac crest (Fig. 1-2, D-E). Note its fusion with the thoracolumbar (lumbodorsal) fascia (G11 4. 28, 4.29, 4.31; G12 4.31, 4.32, 4.34; N168, 173) [R226.9]. Starting from its superior border, carefully cut the latissimus dorsi in a curving line beginning about 5 cm from the spinous processes and passing laterally above the iliac crest (Fig. 1-2, D-E). Reflect the latissimus dorsi laterally. Its nerve and blood supply, the thoracodorsal nerve and artery, will be seen during the axilla dissection.
12. Identify the levator scapulae [R382.2], rhomboid minor [R382.4], and rhomboid major [R382.6] muscles. They attach, from superior to inferior, along the medial border of the scapula (G11 4.28, 4.29, Table 6.4 [p. 496]; G12 4.31, 4.32; N408A-B, 411A-B) [R383.1/2/3]. Sever the origin of the rhomboid major and minor from the vertebral column (Fig. 1-3 A-B) and reflect them laterally (Fig. 1-3, arrow), leaving the levator scapulae intact. Look for the dorsal scapular nerve and artery [R235.23] descending deep to the rhomboids near their scapular attachments. The levator scapulae also receives innervation from the anterior rami of C3-4 but don’t attempt to dissect these nerves. The artery descending along the medial border of the scapula is called the "dorsal scapular artery," even though it may be given a different name (deep branch of the transverse cervical artery) before arriving at the superior border of the scapula. XXX
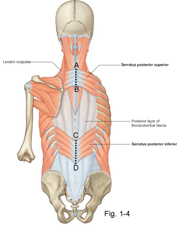
Two thin sheets of muscle, the serratus posterior superior and serratus posterior inferior (Fig. 1-4; G11 4.29; Table 1.1 [p. 21] (Posterior view); G12 4.32, Table 1.1A,B,C[p. 21]; N168, 169), form an intermediate layer of extrinsic muscles in the back deep to the rhomboids and the latissimus dorsi, respectively. The serratus posterior superior passes inferolaterally from the spines of Cv7-Tv3 to attach to ribs 2-5. The serratus posterior inferior angles superolaterally from the spinous processes of Tv11-Lv2 to attach into ribs 9-12. The serratus posterior muscles have traditionally been described as functioning during respiration. They are segmentally innervated by anterior rami of spinal nerves.
13. Clean the serratus posterior superior [R235.24] and inferior [R226.24] muscles and cut their medial attachments. Reflect them laterally (Fig. 1-4 A-B, C-D). Their innervation is difficult to demonstrate, but remember that they are segmentally innervated by the anterior rami of spinal nerves.
STOP HERE - END OF LAB 1
(The 2nd half 'Scapular Region' will be dissected in LAB 2)
SCAPULAR REGION
14. On a skeleton or free scapula identify the coracoid process and acromion, the superior and inferior angles, spine, supraspinous and infraspinous fossae, and the suprascapular and spinoglenoid notches (G11 6.1A-B, 6.31A & C; G12 6.1A-B, 6.31A & D; N407A-B, 408A-B) [R371] [R406]. The spinoglenoid notch is the concave free lateral edge of the spine where it attaches to the body of the scapula. The spinoglenoid notch is traversed by a nerve and vessels passing from the supraspinous fossa into the infraspinous fossa.
15. Find the greater and lesser tubercles of the humerus separated by the intertubercular sulcus. A v-shaped roughening on the anterolateral shaft of the humerus, a little above its middle, is the deltoid tuberosity (G11 6.1A, 6.31A; G12 6.1A, 6.31A; N407A-B,408A-B,409). On the skeleton also note the glenohumeral (shoulder) joint formed between the large head of the humerus and the shallow glenoid cavity of the scapula.
16. If the skin of the shoulder is still intact, make an incision down the lateral side of the shoulder and the upper arm for 12-15 cm. From the lower end of this incision make an incision that encircles the arm. Reflect the skin and superficial fascia carefully from the posterior and lateral aspects of the shoulder and upper arm.
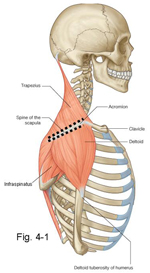
17. Palpate the distal attachment of the trapezius to the spine and acromion of the scapula (Fig. 4-1, G11 6.29, Table 6.4 [p. 496]; G12 6.29; N411A-B). Cut these attachments while protecting the spinal accessory nerve and superficial branch of the transverse cervical artery running on the deep surface of the muscle (G11 6.27, 6.29; G12 6.39A,B,C, 6.29; N31, 171). Leave the trapezius attached to the lateral third of the clavicle. Reflect the rest of the trapezius laterally toward its clavicular attachment to expose the underlying supraspinatus muscle.
The deltoid muscle has the shape of an inverted triangle (Greek letter Δ) and is responsible for the rounded contour of the shoulder (G11 6.38; G12 6.34A-B; N400, 411A-B). Its proximal attachments mirror the distal attachments of the trapezius: inferior margin of the spine and acromion of the scapula and the lateral third of the clavicle (G11 6.27, 6.29, 6.31; G12 6.39A, B, C, 6.29, 6.31A, B, C, D, E; N168, 411A-B). The deltoid descends to insert at the deltoid tuberosity of the humerus. The deltoid muscle contracts to abduct the arm after the first 15°. Abduction is mainly performed by its acromial portion, which has a powerful multipennate internal structure. The clavicular portion of the deltoid helps to flex and medially rotate the arm, and its spinous portion helps to extend and laterally rotate. The clavicular and spinous parts consist of long parallel fibers and are weaker than the acromial portion. The deltoid is supplied on its deep surface by the axillary nerve.
18. Cut the spinous and acromial attachments of the deltoid [R382.9] from the scapula bilaterally (Fig. 4-1) and reflect the posterior portion of each muscle forward toward its clavicular attachment. Leave the clavicular attachment of the deltoid intact. Deep to the superior part of the deltoid muscle and the acromion look for the subacromial (subdeltoid) bursa (G11 6.43B, 6.44A, 6.45A; G12 6.41A, 6.43A; N410A,B,C,D). It may be difficult to demonstrate. Bursae are thin connective tissue sacs with smooth internal surfaces that glide over each other. They contain a small amount of synovial fluid and reduce friction where musculoskeletal structures move across each other. XXX
The supraspinatus is one of four rotator cuff (musculotendinous cuff) muscles—along with the infraspinatus, teres minor, and subscapularis—that help to hold the large head of the humerus in the shallow glenoid cavity of the scapula. The supraspinatus also initiates abduction of the arm (first 15°). It takes origin from the deep fascia overlying it and from the underlying bone of the supraspinous fossa of the scapula. Its tendon passes laterally below the acromion and fuses with the capsule of the shoulder joint to attach to the greater tubercle of the humerus (G11 6.27A-B, 6.28, 6.37, Table 6.5 [p. 497]; G12 6.39 A-B, 6.30E, 6.38, 6.30A & C; N410A,B,C,D, 413A,B,C). The tendon of the supraspinatus is prone to degenerative changes with age, making it the most frequently torn rotator cuff muscle. The tendon may develop calcium deposits (calcific tendinitis) that irritate the subacromial bursa, causing subacromial bursitis, and that result in pain during 50°-130° of abduction (painful arc syndrome). The pain results from contact of the inflamed tissues with the undersurface of the acromion. The supraspinatus is innervated by the suprascapular nerve (C5,6).
On the superior border of the scapula medial to the coracoid process and deep to the supraspinatus, the superior transverse scapular ligament converts the suprascapular notch into a foramen. The suprascapular artery, a branch of the thyrocervical trunk, passes above the superior transverse scapular ligament (G11 6.27; G12 6.39A,B,C; N414A-B [Posterior view], 415A-B), and the suprascapular nerve passes below the ligament, through the suprascapular foramen, to enter the deep surface of the supraspinatus muscle.
The infraspinatus muscle attaches proximally to overlying fascia and to bone of the infraspinous fossa (G11 6.36, 6.37; Table 6.5 [p. 497]; G12 6.37, 6.38, 6.3A & C; N408A-B, 411A-B, 413A,B,C). The infraspinatus’ fibers ascend laterally to fuse with the posterior part of the capsule of the shoulder joint and attach to the greater tubercle of the humerus below the supraspinatus attachment (G11 6.28, 6.31, 6.48C; Table 6.5 [p. 497]; G12 6.30E, 6.31A,B,C,D,E, 6.44F, 6.3A & C; N408A-B, 411A-B, 414A-B [Posterior view], 420A-B). It laterally rotates the arm in addition to helping to stabilize the head of the humerus. The infraspinatus is innervated by the suprascapular nerve, which traverses the spinoglenoid notch from the supraspinous fossa to reach it. The suprascapular nerve may be entrapped at the suprascapular foramen, resulting in paresis (weakness/partial paralysis) and atrophy of the supraspinatus and infraspinatus muscles. Alternatively, the nerve may be compressed at the spinoglenoid notch (e.g., by a hypertrophied inferior transverse scapular ligament), involving only the infraspinatus muscle.
The teres minor muscle is the last and smallest member of the three rotator cuff muscles that are visible from behind (G11 6,36, 6,37; Table 6.5 [p. 497]; G12 6.37, 6.38, 6.3A & C; N411A-B, 413A,B,C, 414A-B [Posterior view]). Its tendon fuses with the posterior aspect of the capsule of the shoulder joint. The teres minor works with the other rotator cuff muscles to hold the head of the humerus against the shallow glenoid cavity and also laterally rotates the arm. The axillary nerve supplies teres minor. Due to its much smaller physiologic cross-sectional area, paralysis of the teres minor results in relatively little weakness in lateral rotation of the arm compared to paralysis of the infraspinatus.
The subscapularis is the fourth rotator cuff muscle. It crosses the shoulder joint anteriorly and will be seen during the axilla dissection.
The teres major takes origin from the back of the inferior angle and lower lateral border of the scapula and passes medial to the humerus to attach into the crest of the lesser tubercle (medial lip of intertubercular sulcus) (G11 6.31, 6.32, 6.36, 6.37; G12 6.31A,B,C,D,E, 6.33A, 6.37, 6.38; N408A-B, 411A-B [Posterior view], 414A-B [Posterior view], 420A-B). The attachment of teres major’s tendon to the humerus is closely related to that of the latissimus dorsi (G11 6.33, 6.34A; G12 6.33B, 6.35B; N407A-B, 412). The teres major is not a rotator cuff muscle! It medially rotates and adducts the arm under control of the lower subscapular nerve but normally contracts only if the motion is resisted (i.e., it is a reserve muscle).19. Remove the deep (supraspinatus) fascia covering the right and left supraspinatus muscles, realizing that each muscle takes part of its origin from the fascia. Make a vertical incision through the supraspinatus muscle [R406], down to bone, 3-4 cm lateral to the vertebral (medial) border of the scapula. Carefully reflect the lateral part of the muscle toward the humerus. Starting at the superior angle of the scapula, palpate laterally along the sharp superior border until you encounter a duller (thicker) edge that angles upward. This is the superior transverse scapular ligament [R406.5]. Identify the suprascapular nerve [R406.4] traversing the suprascapular notch, which is converted into a foramen by the ligament, to enter the deep surface of the supraspinatus muscle. Clean the suprascapular artery [R406.3] passing above the superior transverse scapular ligament to enter the muscle.
20. Remove the deep fascia covering the infraspinatus muscle [R405.18]. Make a vertical incision through the infraspinatus 5 cm lateral to the vertebral border of the scapula and reflect the lateral part of the divided muscle toward its humeral attachment. Clean the suprascapular nerve and artery as they pass through the spinoglenoid notch of the scapula to enter the deep surface of the infraspinatus (G11 6.27B-C, 6.37; G12 6.39B-C, 6.38; N408A-B, 414A-B [Posterior view], 415A-B [Posterior view]). The spinoglenoid notch [R406.5] connects the supraspinous and infraspinous fossae lateral to the attachment of the spine of the scapula to its body.
21. Identify the teres minor muscle [R405.19] as it passes from the middle of the lateral border of the scapula to the lowest articular facet on the greater tubercle of the humerus. Notice how much smaller it is than the infraspinatus muscle; therefore, although both the infraspinatus and teres minor laterally rotate the humerus, the teres minor is much weaker in its action due to its smaller physiologic cross-sectional area.
22. Locate the teres major muscle [R405.21], which arises from the back of the inferior angle and the lower third of the lateral border of the scapula. It passes medial to the humerus, and its insertion on the crest of the lesser tubercle can’t be seen at this time. The teres major is not a rotator cuff muscle. XXX
The long head of the triceps brachii, a muscle of the posterior compartment of the arm, attaches proximally to the infraglenoid tubercle of the scapula. The long head descends between the teres minor and teres major muscles to join the medial and lateral heads of the triceps (G11 6.37; G12 6.38; N414A-B [Posterior view], 420A-B). The long head of the triceps brachii separates two spaces in the scapular region, the triangular space medial to the long head from the quadrangular space lateral to it. The triangular space is bounded by the teres minor, teres major, and long head of triceps, and is traversed by the scapular circumflex artery (G11 6.37; G12 6.38; N415A-B). The scapular circumflex artery, which is a branch of the subscapular artery from the axillary artery, is usually easy to identify at this location.
The quadrangular space is bounded by the teres minor, teres major, long head of triceps, and surgical neck of the humerus (G11 6.36, 6.37; G12 6.37, 6.38; N414A-B [Posterior View], 420A-B). The axillary nerve and posterior humeral circumflex artery traverse the quadrangular space from the axilla to reach the deep surface of the deltoid. Fractures of the surgical neck are common fractures of the humerus and may injure the axillary nerve, paralyzing the deltoid and teres minor muscles. The nerve also may be injured in a shoulder (glenohumeral) joint dislocation. Deltoid weakness is noticed mainly in loss of abduction of the arm after the first 15°. There is also a small area of sensory loss over the deltoid. The rounded contour of the shoulder disappears as the deltoid atrophies.23. Clean the upper part of the long head of the triceps brachii [R404.10] and identify the boundaries of the triangular space [R404.5] and quadrangular space [R404.9]. Within the triangular space, locate the scapular circumflex artery. Demonstrate the axillary nerve and posterior humeral circumflex artery as they emerge through the quadrangular space, noting their close relationship to the surgical neck of the humerus. Clean and attempt to preserve branches entering the deltoid muscle. XXX
Do not attempt to demonstrate, but be aware of, the arterial anastomoses around the scapula that allow safe ligation of the axillary artery proximal to its subscapular branch (G11 6.11B, 6.27B; G12 6.7B, 6.39B; N415A-B). The scapular circumflex artery anastomoses with the dorsal scapular artery (or deep branch of the transverse cervical) and suprascapular artery. Ligation or injury of the axillary artery distal to the subscapular artery, between it and the profunda brachii (deep artery of the arm), cuts off the blood supply to the upper limb, resulting in ischemic tissue necrosis and loss of the limb!
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.