Pectoral Region and Axilla
For this dissection the cadaver must be in a supine (face up) position.
The pectoral region is the area at the junction of the trunk and the upper limb that contains the pectoralis major and pectoralis minor muscles (G11 1.1, 1.2, 1.3, 1.6, 6.15, 6.16, 6.17; G12 1.1, 1.2, 1.3, 1.6A-B, 6.15, 6.16; N175,176A-B, 177, 182, 183). In females, the breast is a clinically important structure insuperficial fascia overlying the pectoralis major. The pectoralis major and minor muscles form the anterior wall of the axilla, which is a pyramidal space providing passage to neurovascular structures that enter and leave the upper limb (G11 6.18, 6.20, 6.21; G12 6.18, 6.20A-B, 6.21A-B-C; N411A-B [Anterior view], 412, 415A-B, 416A-B, 417). The axilla contains a number of important structures, including the brachial plexus of nerves, the axillary artery and its branches, the axillary vein and its tributaries, and the axillary lymph nodes.
The study of the pectoral region is made easier by learning associated skeletal structures. The most important of these are the sternum, the ribs and costal cartilages, the clavicle, and the acromion and coracoid process of the scapula (G11 1.9A, 1.10A & C, 6.1; G12 1.9A, 1.10A & C, 6.1A-B; N179A-B, 180A-B-C, 407A-B, 409). The sternum is a long, flat bone located in the middle of the anterior part of the thoracic wall. The sternum articulates laterally with costal cartilages that continue toward it from the anterior ends of the ribs. The space between two adjacent ribs and their costal cartilages is an intercostal space. The ribs, costal cartilages, and intercostal spaces will be studied in more detail in a later dissection, but note that only the costal cartilages of the upper 7 ribs (true ribs) articulate directly with the sternum.
From above downward, the sternum consists of the manubrium, body, and xiphoid process. The shallow concavity at the superior border of the manubrium is the suprasternal (jugular) notch (G11 1.9A, 1.10; G12 1.9A, 1.10A-B-C-D; N179A-B, 180A-B-C [lower]). The manubrium and body of the sternum meet at the sternal angle (manubriosternal joint). The sternal angle is the level at which the second costal cartilages articulate with the sternum, and that relationship makes the sternal angle useful in counting ribs, which may be difficult in heavily muscled or obese individuals. The xiphoid process usually angles posteriorly at the xiphisternal junction, which is the level of articulation of the seventh costal cartilages with the sternum. The sternal angle and xiphisternal junction are useful landmarks indicating the positions of some thoracic and abdominal organs, as will be seen in later dissections. For example, the xiphisternal joint indicates the approximate midline level of the inferior border of the heart and the superior limit of the liver.
The clavicle (collar bone) is curved, with the medial part being convex anteriorly and the lateral part being concave anteriorly (G11 1.9, 6.1, 6.13, 6.39B; G12 1.9A-B, 6.1A-B, 6.13, 6.40B; N179A-B, 406A-B-C, 407A-B). The clavicle is one of the most frequently fractured bones in the body. Its enlarged medial end articulates with the sternum at the sternoclavicular joint, and its flattened lateral end articulates with the acromion of the scapula at the acromioclavicular joint (G11 1.9A, 6.1, 6.39A, 6.47; G12 1.9A, 6.1A-B, 6.40A, 6.44A; N179A-B, 180 [lower], 406A-B-C, 407A-B). The sternoclavicular joint is the only true joint between the axial skeleton—the skeleton of the trunk—and the appendicular skeleton of the upper extremity. The coracoid process of the scapula is located slightly medial and inferior to the acromioclavicular joint.
1. Identify the manubrium, body, and xiphoid process on the sternum of a skeleton. Find the suprasternal (jugular) notch [R192.12], sternal angle [R192.8], and xiphisternal junction on a skeleton and palpate them on the cadaver. Attempt to count ribs on the cadaver by finding the second costal cartilages [R192.13]articulating at the sternal angle and using them for reference.
2. Identify the acromion [R372.6]and coracoid process [R372.13] of the scapula on the skeleton. Verify that the clavicle articulates with the sternum medially at the sternoclavicular joint and laterally with the acromion at the acromioclavicular joint. On the cadaver palpate the enlarged sternal end of the clavicle at the sternoclavicular joint. Run your fingers laterally along the anterior surface of the curved clavicle to the acromion of the scapula, which forms the bony point of the shoulder. Unless the acromioclavicular joint is enlarged, it may be difficult to palpate through the preserved skin. Note the position of the coracoid process inferomedial to the acromioclavicular joint on the skeleton but don’t attempt to palpate the process on the cadaver.
The male breast is unremarkable. On female cadavers, the breasts are superficial structures of clinical importance. Each breast overlies ribs 2-6 on the anterior chest wall, and an axillary tail may extend laterally as far as the midaxillary line (G11 1.3, 1.6B; G12 1.3, 1.6B; N176A-B, 177). The breast consists of the mammary gland, which is an accessory gland to reproduction, located in superficial fascia that contains a variable amount of fat. The mammary glands are atrophied in elderly females.
The nipple is a conical prominence surrounded by a circular pigmented area of skin, the areola. The nipple contains the openings of 15-20 lactiferous ducts, which converge toward it from the lobes of the surrounding mammary gland (G11 1.3, 1.4B; G12 1.3, 1.4B; N176A-B). Each lactiferous duct has a dilated portion, the lactiferous sinus, just proximal to its opening on the nipple for milk accumulation in the nursing mother. The lobes of the gland and associated fat are separated into compartments by connective tissue septa called suspensory ligaments (of Cooper), which are better developed superiorly (G11 1.3, 1.4; G12 1.3, 1.4A-B; N176A-B). Fibrosis and shortening of the suspensory ligaments or invasion of the lactiferous ducts in breast cancer may produce dimpling of the skin and retraction of the nipple. Puffy, edematous skin between pores due to obstruction of lymphatic vessels may give the skin an orange-peel appearance (peau d’orange sign).
The blood supply of the breast is mainly from the internal thoracic and lateral thoracic arteries with smaller contributions from the posterior intercostal arteries (G11 1.7; G12 1.7; N177). The venous drainage corresponds to the arterial supply, with most of the blood emptying into the internal thoracic and lateral thoracic veins. The posterior intercostal veins drain into the azygos system of veins located beside the bodies of vertebrae and have important connections with the vertebral venous plexuses of vein (G11 1.73, 1.74, 4.26; G12 1.75A-B, 4.20A-B; N166A-B-C, 186, 250). The connection of posterior intercostal veins with the vertebral venous plexuses provides a pathway for the metastasis of breast cancer to the vertebrae, spinal cord, and brain.
75% of the lymphatic drainage of the breast is to axillary lymph nodes located along the axillary vein and its main tributaries (G11 1.8, 6.19; G12 1.8, 6.19; N178). Lymph from the medial quadrants of the breast drains largely to the parasternal lymph nodes along the internal thoracic vein. Smaller amounts drain to the opposite breast and into upper abdominal lymph nodes. Although we will not attempt to dissect the lymphatic vessels and axillary lymph nodes, knowledge of the lymphatic drainage of the breast is essential in predicting the metastasis of breast cancer. It is worth noting that unexplained enlargement of the axillary lymph nodes in a female patient suggests the possibility of breast cancer and should be investigated. Breast cancer also occurs in males but accounts for only about 1.5% of cancer cases.
The nerve supply of the breast is from branches of the 2nd - 6th intercostal nerves (G11 1.6, 1.18; G12 1.6A-B, 1.18; N182). The anterior cutaneous branches of intercostal nerves pierce the overlying muscle to emerge into superficial fascia just lateral to the sternum. The lateral cutaneous branches arise near the midaxillary line (G11 1.2, 1.6, 1.18; G12 1.2, 1.6A-B, 1.18,182, 185).
The lateral cutaneous branch of the second intercostal nerve, the intercostobrachial nerve, is important for a different reason. It continues onto the medial surface of the arm (G11 6.15, 6.20A; G12 6.15, 6.20A-B; N183, 403A-B, 417) and provides a pathway for referred pain from the heart (i.e., heart pain is often referred to the medial side of the arm, usually the left arm but occasionally the right).
The upper part of the anterior thoracic wall, above the breast, receives its cutaneous innervation from branches of cervical spinal nerves 3-4 that descend across the clavicle, the supraclavicular nerves (G11 6.4, 6.13, 8.3A, Table 8.1 [p. 722]; G12 Table 6.6, 6.13, 8.5A, Table 8.1; N 30, 403A-B). The supraclavicular nerves pierce a thin subcutaneous sheet of muscle ascending across the clavicle from its origin in pectoral fascia. This is the platysma, a muscle of facial expression that will be studied later.
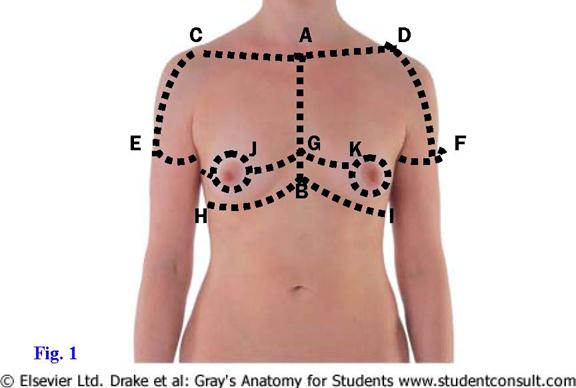
3. Make a vertical incision through the skin in the midline from the suprasternal notch to the xiphoid process (Fig. 1, A-B). From this incision, make three transverse incisions on each side as follows:
►From the suprasternal notch along the clavicle to the acromion (A-C and A-D) and continuing down the arm about 15 cm. Make a circular incision around the arm at that level (E and F). This may have been done during the first lab period.
►From the midline horizontally to the areola (G-J and G-K) and encircling it continue to the midaxillary line.
►From the xiphisternal junction laterally to the midaxillary line (B-H and B-I).
4. Reflect the skin from the underlying superficial fascia. Clean two or three anterior [R207.6] and lateral cutaneous branches [R207.8] of intercostal nerves in the superficial fascia. Look for the lateral cutaneous branches near the midaxillary line. Identify the intercostobrachial nerve [R410.8] emerging from the second (occasionally the third) intercostal space and continuing onto the medial side of the arm.
5. Attempt to find small branches of the supraclavicular nerves [R207.3] descending to skin of the upper part of the thorax but do not dissect above the clavicle. Look also for a thin subcutaneous sheet of muscle ascending across the clavicle. This is the platysma muscle (G11 6.13, 8.3; G12 6.13, 8.5A; N25).
6. In male cadavers reflect the superficial fascia of the pectoral region as a single layer. In female cadavers, make a vertical incision through the breast at the level of the nipple. Attempt to find a few lactiferous ducts and sinuses (G11 1.4B; G12 1.4B; N176A-B). Note that the lactiferous ducts radiate outward from the nipple, a fact taken into account when surgical incisions are necessary (e.g., to drain an abscess). Scoop fat from the superior part of the breast and clean some suspensory ligaments, which appear as thin, intersecting sheets of connective tissue. After studying the breast, reflect it and the rest of the superficial fascia laterally as a single layer or remove it and set it aside for later study. XXX
The breast can be reflected as a unit because it is separated from the underlying deep fascia covering the pectoralis major muscle (pectoral fascia) by a potential space, the retromammary bursa (retromammary space) (G11 1.3, 1.4B; G12 1.13A-B, 1.4B). This potential space allows movement of the healthy breast over the chest wall. In carcinoma of the breast, cancer cells may invade the retromammary bursa and the underlying pectoral fascia, fixing the breast to the pectoralis major muscle. Consequently, the breast contour changes (e.g., dimpling) and the breast may elevate when the muscle contracts. Having a patient tense her pectoral muscles with her hands on her hips is a standard part of clinical examinations for breast cancer.
The pectoralis major has clavicular and sternocostal heads (G11 6.13, 6.14, 6.17A, Table 6.1 [p. 479]; G12 6.13, 6.14, Table 6.2; N175, 411A-B). The clavicular head takes origin from the medial half of the clavicle. It is separated from the deltoid muscle by the deltopectoral triangle, which contains the terminal portion of the cephalic vein. The larger sternocostal head of pectoralis major attaches both to the anterior surface of the sternum and to costal cartilages deep to the muscle. The sternocostal head occasionally is congenitally absent. The two heads of pectoralis major converge to attach on the humerus at the crest of the greater tubercle (lateral lip of intertubercular groove) (G11 6.1, Table 6.1 [p. 479]; G12 6.1A-B, Table 6.2; N407A-B). The pectoralis major adducts and medially rotates the arm. It is innervated by both the lateral and medial pectoral nerves.
7. Clean and preserve the cephalic vein traversing the deltopectoral triangle [R384.3]. Remove the pectoral fascia from the pectoralis major muscle (G11 6.13, 6.18B; G12 6.13; N403A-B) [R384.6/7]. Carefully sever the attachment of the clavicular head of pectoralis major from the clavicle and begin to reflect it laterally. As you do so, insert a finger beneath the clavicular head and feel the lateral pectoral nerve [R208.15] and pectoral branches of the thoracoacromial artery [R409.17/18]entering the deep surface of the muscle (G11 6.18A, 6.23; G12 6.18, 6.24; N415A-B [Anterior view], 417). Preserve these structures.
8. Cut the attachments of the sternocostal head of the pectoralis major from the sternum and costal cartilages and reflect it laterally. Try to preserve the delicate medial pectoral nerve [R409.34], which usually pierces the pectoralis minor muscle [R208.17] to enter the deep surface of pectoralis major (G11 6.18, 6.23; G12 6.18, 6.24; N417). Note that the medial pectoral nerve actually is located lateral to the lateral pectoral nerve, but the pectoral nerves are named according to the cord of the brachial plexus from which they branch. XXX
Deep to the pectoralis major is clavipectoral fascia, which descends from the clavicle above to the axillary fascia in the base of the axilla (armpit) below. The clavipectoral fascia splits to enclose the pectoralis minor muscle (G11 6.18; G12 6.18; N416A-B).
The pectoralis minor arises from ribs 2-5 or 3-5 and inserts on the coracoid process of the scapula. The pectoralis minor stabilizes the scapula and tilts it forward and downward on the thoracic wall. It is supplied by the medial pectoral nerve.
9. Study the clavipectoral fascia descending from the clavicle to the medial border of the pectoralis minor muscle (G11 6.18; G12 6.18; N416A-B). Clean the pectoralis minor [R208.17] and cut its costal attachment. Reflect it toward the coracoid process of the scapula, preserving the medial pectoral nerve [R409.34]that usually pierces the muscle. XXX
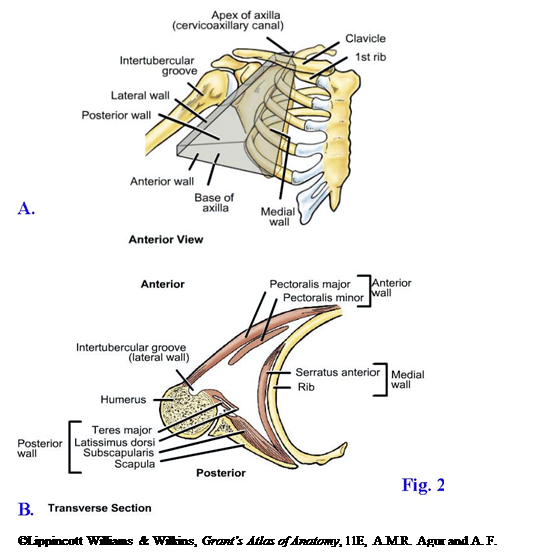
The axilla is a pyramidal space at the junction of the thorax and arm (Fig. 2; G11 6.20, 6.21; G12 6.20A-B, 6.21A-B-C; N416A-B [Oblique parasagittal section], 417). It is a passageway for important nerves and vessels passing between the root of the neck and the upper limb. The axilla has an apex, a base, and four walls (G11 6.20B; G12 6.20A-B).
The apex of the axilla is the passageway (cervicoaxillary canal) between the neck and the axilla bounded by the first rib, clavicle, and superior border of the scapula (Fig. 2A; G11 6.20B; G12 6.20A-B; N417). The base is the concave skin, superficial fascia, and deep axillary fascia of the axillary fossa (armpit) (G11 6.18B; N416A-B).
The anterior wall of the axilla is formed by the pectoralis major and minor muscles and their associated fasciae (G11 6.21; G12 6.21A-C; N416A-B). The anterior axillary fold is the most inferior part of the anterior wall (Fig. 2B; G11 1.1, 6.14; G12 1.1, 6.14). The posterior wall of the axilla is formed mainly by the subscapularis muscle covering the scapula. The most inferior part of the posterior wall, the posterior axillary fold, is formed by the latissimus dorsi and teres major muscles (G11 1.1, 6.14, 6.24; G12 1.1, 6.14, 6.25A; N412 (no image), 416A-B, 417). The medial wall is the upper ribs and intercostal spaces covered by the serratus anterior muscle, which passes from the upper 8 or 9 ribs to the medial (vertebral) border of the scapula. The lateral wall of the axilla is the intertubercular groove of the humerus (G11 6.21B; G12 6.21A-B-CB; N407A-B).
The contents of the axilla are the axillary artery and its branches, the axillary vein and its tributaries, axillary lymph nodes and vessels, and the brachial plexus of nerves. All of these structures are embedded in axillary fat. The axillary artery, axillary vein, and axillary portion of the brachial plexus are also enclosed by a sleeve-like extension of prevertebral fascia, the axillary sheath (G11 6.20; G12 6.20A-B; N416A-B [Oblique parasagittal section, not labeled]). Anesthetic sometimes is injected into the axillary sheath to block the brachial plexus for upper extremity surgery.
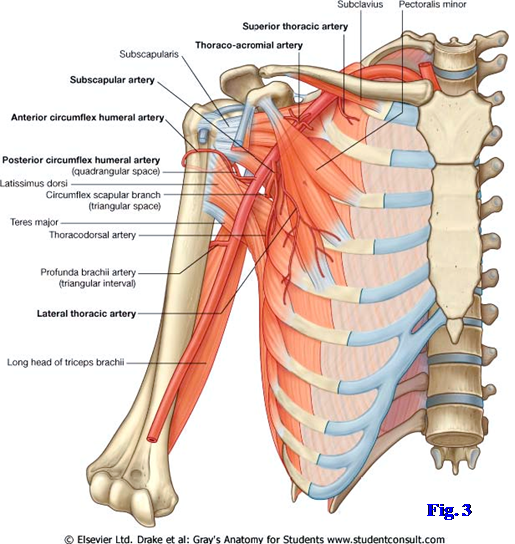
The axillary artery begins at the lateral border of the first rib and ends at the inferior border of the teres major muscle (G11 6.11, 6.22, 6.23, 6.24; Table 6.2 [p. 484]; G12 6.7A-B-C-D, 6.22A-B-C, 6.46, 6.24, 6.25A; N415A-B, 417, 422). It is the continuation of the subclavian artery and becomes the brachial artery. The pectoralis minor muscle is used as a landmark to divide the axillary artery into three parts. The first part of the axillary artery is medial to pectoralis minor, the second part is deep (posterior) to it, and the third part is lateral to it (Fig. 3; G11 6.23, 6.24, Table 6.2 [p. 484]; G12 6.24, 6.25A-B, 6.22A-B-C; N415A-B, 417).
The first part of the axillary artery has one branch, the superior (supreme) thoracic artery, which helps supply the first and second intercostal spaces. The second part has two branches, the thoracoacromial artery and the lateral thoracic artery. The thoracoacromial artery has a short trunk that quickly divides into pectoral, deltoid, acromial, and clavicular branches (G11 6.18; G12 6.18; N415A-B). The lateral thoracic artery is variable in origin. It often arises from the axillary artery near the lateral border of pectoralis minor and descends across the superficial surface of the serratus anterior muscle with the long thoracic nerve. Alternatively, the lateral thoracic may branch from the thoracodorsal or subscapular artery (described below).
The third part of the axillary artery has three branches—subscapular, anterior humeral circumflex, and posterior humeral circumflex (Fig. 3; G11 6.11A-B, 6.22A; G12 6.7A-B, 6.22C; N415A-B, 417). The subscapular artery is a large artery that descends a short distance before dividing into scapular circumflex and thoracodorsal branches (G11 6.11A-B, 6.23, 6.24; G12 6.7A-B, 6.24, 6.25A; N415A-B, 417). The scapular circumflex artery traverses the triangular space formed by the long head of triceps brachii, subscapularis (teres minor from a posterior view), and teres major muscle to reach the back of the scapula. The scapular circumflex joins the dorsal scapular and suprascapular arteries in forming arterial anastomoses around the scapula that may allow surgical ligation of the axillary artery proximal to the subscapular branch (G11 6.11A-B; G12 6.7A-B; N415A-B [Posterior view]).
The thoracodorsal artery accompanies the thoracodorsal nerve to supply the latissimus dorsi (G11 6.23, 6.24; Table 6.2 [p. 484]; G12 6.24, 6.25A, 6.22A; N417). The thoracodorsal artery frequently gives rise to a lateral thoracic branch to supply the serratus anterior and may completely replace that branch from the second part of the axillary artery.
The anterior humeral circumflex and posterior humeral circumflex arteries pass anteriorly and posteriorly, respectively, around the humerus. The posterior humeral circumflex artery traverses the quadrangular space with the axillary nerve (G11 6.24, 6.25, 6.36, 6.37; G12 6.25A, 6.26, 6.37, 6.38; N414, 415A-B, 417). The clinically important quadrangular space is formed by the long head of the triceps brachii, surgical neck of the humerus, teres major, and subscapularis (G11 6.25; G12 6.26; N414). The teres minor muscle substitutes for the subscapularis as a boundary of the quandrangular space from a posterior view (G11 6.36, 6.37; G12 6.37, 6.38; N414).
The axillary vein begins as the continuation of the basilic vein at the lower border of the teres major muscle and becomes the subclavian vein at the lateral border of the first rib (G11 6.8A, 6.19; G12 6.8A, 6.19; N183, 250, 417). The axillary vein is formed when the basilic vein is joined by the brachial veins, which accompany the brachial artery. It occupies a position anterior and slightly inferior to the axillary artery. The axillary vein receives tributaries roughly corresponding to branches of the axillary artery, but there are additional veins, which are highly variable. The cephalic vein, which was seen earlier, is a tributary of the terminal part of the axillary vein (G11 6.13, 6.18A, 6.19; G12 6.13, 6.18, 6.19; N183, 250, 416A-B).
10. Carefully abduct the upper extremity to about 45°--the bones of some cadavers with osteoporosis are fragile and easily broken--and prop or tie it in position. Bluntly remove the fat from the axilla. DO NOT USE A SCALPEL TO DISSECT THE AXILLA! Clean the cephalic vein [R408.6] where it ends as a tributary of the axillary vein. Note that the axillary vein, axillary artery, and major portion of the brachial plexus are enclosed within a sleeve of fascia, the axillary sheath, which is useful in performing an anesthetic nerve block of the brachial plexus. Leave the junction of the cephalic and axillary veins intact, but cut and remove the lateral part of the axillary vein and its tributaries.
11. Be able to explain the clinical importance of the axillary lymph nodes [R410.10], but do not attempt to dissect them.
12. Replace the pectoralis minor muscle in its original position to help visualize the three parts of the axillary artery. Clean the branches of the axillary artery. Look for the small superior thoracic artery [R412.24] descending from the first part of the artery to supply the first two intercostal spaces. It is frequently small and may be difficult to find.
13. The thoracoacromial and lateral thoracic arteries are the two branches from the second part of the axillary artery. The thoracoacromial artery [R409.17] arises near the medial border of the pectoralis minor and pierces the clavipectoral fascia beside it (G11 6.18A, 6.23; G12 6.18, 6.23A-B; N415A-B [Anterior view], 417). The short trunk of the thoracoacromial artery quickly divides into pectoral, acromial, deltoid, and clavicular branches. Look for the lateral thoracic artery [R412.25] descending across the serratus anterior [R412.13] muscle from near the lateral border of the pectoralis minor. The lateral thoracic artery is subject to much variation and may arise from the thoracodorsal or subscapular artery instead of the second part of the axillary artery.
14. Find the three branches of the third part of the axillary artery. The large subscapular artery [R413.19] descends near the lateral border of the subscapularis muscle. After 2-3 cm it divides into scapular circumflex [R412.8] and thoracodorsal arteries [R412.10]. The scapular circumflex artery passes backward through the triangular space [R404.5], which is defined by the subscapularis, teres major, and long head of the triceps muscles. The thoracodorsal artery [R410.12] descends on the posterior wall of the axilla to reach the latissimus dorsi muscle [R410.14].
15. Clean the anterior humeral circumflex and posterior humeral circumflex arteries. They may arise from a common trunk or arise from the axillary artery separately but near each other. The small anterior humeral circumflex artery passes anterior to the surgical neck of the humerus. The larger posterior humeral circumflex artery [R404.9] passes posteriorly around the surgical neck of the humerus. Find this artery as it disappears from the axilla through the quadrangular space with the axillary nerve [R404.9]. The quadrangular space is formed by the subscapularis (teres minor from a posterior view), teres major, long head of the triceps, and surgical neck of the humerus. XXX
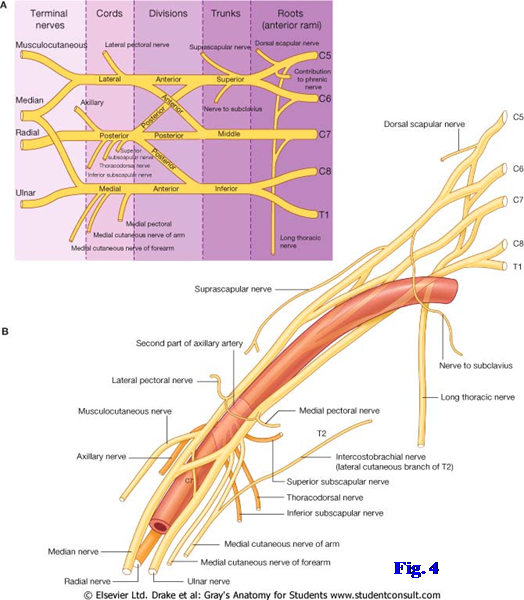
The brachial plexus is the major nerve supply of the upper extremity. Like other somatic nerve plexuses, it is formed by anterior rami and mixes nerve fibers from several spinal nerves (C5-T1) together to form peripheral nerves (Fig. 4; G11 Table 6.3 [pp. 486-487]; G12 6.23A; N417, 418). Only part of the brachial plexus can be seen at the present, but it is helpful to understand the general arrangement of the plexus: The anterior rami of C5 and C6 join to form the superior trunk, C7 forms the middle trunk, and C8 and T1 join to form the inferior trunk. Each trunk divides into an anterior division to supply the anterior (flexor) compartments of the extremity and a posterior division to supply the posterior (extensor) compartments (Fig. 4; G11 Table 6.3 [p. 486]; G12 6.23A; N418 lateral cord, and the anterior division of the inferior trunk forms the medial cord. The posterior divisions of all three trunks join to form the posterior cord.
The cords are named according to their relationship to the second part of the axillary artery. There are five principal terminal branches of the brachial plexus and several smaller branches. The lateral and medial cords contribute lateral and medial roots, respectively, to form the median nerve. The lateral cord continues as the musculocutaneous nerve, and the medial cord continues as the ulnar nerve. The posterior cord divides into the axillary nerve and the radial nerve.
16. Only the cords and the proximal portion of some branches of the brachial plexus will be exposed at this time. Using BLUNT DISSECTION, find the lateral cord and its continuation, the musculocutaneous nerve [R413.5/6]. The musculocutaneous nerve pierces the coracobrachialis muscle, which attaches to the coracoid process of the scapula beside the short head of the biceps brachii (G11 6.23, 6.25; G12 6.24, 6.26; N417, 419A-B). Trace the lateral root of the median nerve to the median nerve [R413.8]. Proximal to the lateral root of the median nerve, find where the lateral pectoral nerve branches from the lateral cord and again trace it to the clavicular head of the pectoralis major.
17. Clean the medial cord [R413.18] of the brachial plexus and the first part of its continuation, the ulnar nerve [R413.21] (Fig. 4; G11 6.23; Table 6.3 [p. 486]; G12 6.24, 6.23A; N417, 418 medial root of the median nerve branches from the medial cord to join the lateral root in forming the median nerve. Identify it. Proximal to the medial root of the median nerve, find the slender medial pectoral nerve and trace it through the pectoralis minor muscle or around its lateral edge to the sternocostal head of the pectoralis major. Find two larger branches of the medial cord descending parallel to the ulnar nerve. They are the medial brachial cutaneous nerve and the medial antebrachial cutaneous nerve [R415.12]. XXX
Before its terminal division, the posterior cord gives off three smaller branches—the upper subscapular, thoracodorsal (middle subscapular), and lower subscapular nerves. The upper and lower subscapular nerves enter the subscapularis muscle (G11 6.24, 6.25; G12 6.25A, 6.26; N412 (no image) [Note: the labels for the “Upper subscapular nerve” and “Lower subscapular nerve” are reversed], 417). The lower subscapular nerve also innervates the teres major. The thoracodorsal nerve descends with the thoracodorsal artery to enter the deep surface of the latissimus dorsi.
Another important branch of the brachial plexus, which is formed by direct contributions from the anterior rami of C5-7, is the long thoracic nerve (G11 6.23, 6.24, 6.25, 6.26; G12 6.24, 6.25A, 6.27; N414 [Lateral view], 417). It descends across the superficial surface of the serratus anterior muscle with the lateral thoracic artery.
Injuries of the brachial plexus from disease or trauma are an important cause of disability. Injuries of the upper brachial plexus involve the anterior rami of C5 and C6 and usually result from a forcible increase in the angle between the neck and the shoulder. This may occur, for example, when the rider is thrown from a motorcycle onto one side of the head and shoulder or when a baby’s head is pulled during a difficult delivery. The resulting Erb-Duchenne palsy (Erb’s palsy) results in a characteristic “waiter’s tip posture” with the arm adducted and medially rotated, the forearm extended and pronated, and the palm facing backward. What is the explanation for this posture?
The subscapularis muscle passes laterally from the subscapular fossa on the costal surface of the scapula to insert into the lesser tubercle of the humerus (G11 6.24, 6.25, 6.32; G12 6.25A, 6.26, 6.33A; N407A-B, 412 (no image), 413A-B, 414). The subscapularis crosses anterior to the shoulder (glenohumeral) joint and, therefore, is a medial rotator of the arm. The subscapular bursa is located between the subscapularis tendon and the articular capsule of the shoulder joint and communicates with the synovial cavity of the joint (G11 6.41, 6.43A; G12 6.42A-B-C; N410A-B). Bursae are thin connective tissue sacs with smooth internal surfaces lubricated by a small amount of synovial fluid to reduce friction. They are found where musculoskeletal structures move across each other.
Along with the supraspinatus, infraspinatus, and teres minor, the subscapularis is one of the rotator cuff muscles. These short muscles reinforce the capsule of the shoulder joint, helping to hold the large head of the humerus against the shallow glenoid cavity of the scapula (G11 Table 6.5 [p. 497]; G12 6.30C; N413A-B-C). They are dynamic stabilizers of the glenohumeral joint, and the rupture of a rotator cuff tendon due to trauma or degenerative changes produces a painful and debilitating injury.
The serratus anterior muscle overlies the upper ribs and helps to form the medial wall of the axilla (G11 6.21A-B, 6.23, 6.24, 6.26; G12 6.21A-B-C, 6.24, 6.27, N175,, 183, 411A-B, 414 [Lateral view]). It arises by pointed slips from the anterolateral surfaces of the upper 8-9 ribs, giving it a serrated appearance. The serratus anterior follows the curvature of the rib cage posteriorly and medially to attach to the entire length of the vertebral (medial) border of the scapula. It protracts and upwardly rotates the scapula under control of the long thoracic nerve. The long thoracic nerve’s relatively superficial position makes it vulnerable both to trauma and axillary surgery (e.g., a radical mastectomy for breast cancer). Injury to this nerve results in the medial border and inferior angle of the scapula pulling away from the posterior thoracic wall during arm movements (winging of the scapula). The patient is unable to raise the arm above the horizontal plane due to loss of upward rotation of the glenoid cavity of the scapula.
18. Identify the posterior cord [R413.17]of the brachial plexus behind the second part of the axillary artery (G11 6.24, 6.25; G12 6.25A, 6.26; N416A-B [Oblique parasagittal section], 417). Clean the proximal portions of its terminal branches, the radial [R413.10] and axillary nerves [R413.7]. Trace the axillary nerve until it disappears into the quadrangular space with the posterior humeral circumflex artery [R404.9]. Follow the larger radial nerve [R404.21] until it enters the arm.
19. Proximal to the posterior cord’s division into the radial and axillary nerves, find the smaller upper subscapular, thoracodorsal, and lower subscapular nerves. The short upper subscapular nerve, often double, pierces the subscapularis muscle and may be difficult to find. Clean the thoracodorsal nerve [R412.10] as it descends with the artery of the same name to supply the latissimus dorsi muscle [R412.12]. The lower subscapular nerve frequently appears to branch from the axillary nerve just proximal to that nerve’s entrance into the quadrangular space. Find the lower subscapular nerve’s branches to the subscapularis and teres major.
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.