Gluteal Area and Posterior Thigh
The lower extremity (lower limb) is specialized to support weight, to maintain balance, and to move the body from one place to another (locomotion). It is a more substantial structure than the upper extremity, which functions mainly to place the hand in the optimum position to manipulate objects. The skeleton of the lower extremity is divided into the pelvic girdle, which articulates with the axial skeleton, and the skeleton of the free portion of the extremity (Fig. 1; Gr 5.1). The pelvic girdle is formed by the hip bone (coxal bone, innominate bone), which articulates with the other hip bone in the anterior midline at the cartilaginous pubic symphysis (Gr 3.1, 3.2, 5.20A; Ne 332, 333). Posteriorly the hip bones articulate with the sacrum at the strong sacroiliac joints. The two hip bones join the sacrum and coccyx in forming the bony pelvis.
(See Figure 1)
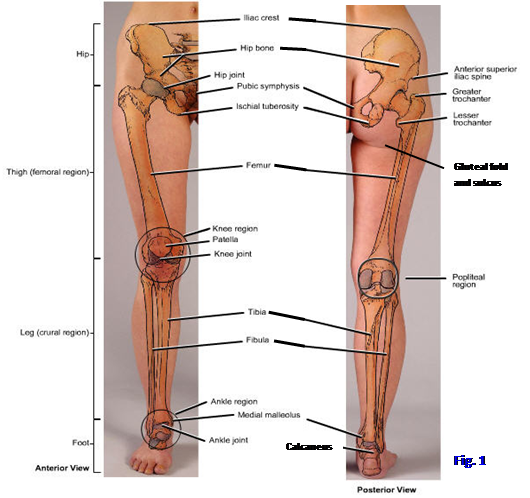
The skeleton of the free portion of the lower extremity consists of the femur, tibia and fibula, tarsal bones, metatarsal bones, and phalanges (Figs. 1, 2; Gr 5.1, 5.20, 5.60, 5.68; Table 5.8 [p. 405]; Ne 477, 501A, 501B, 511A, 511B, 512A, 512B). The head of the femur articulates with the pelvic girdle at the acetabulum, a deep cup-shaped fossa, to form the hip joint (Gr 5.20A, 5.30, 5.31; Ne 332, 333, 474-477). The distal portion of the femur, represented by the femoral condyles, articulates with the tibia at the knee joint. Both the tibia and the bone lateral to it, the fibula, articulate at the ankle joint with the most superior tarsal bone, the talus. The tibia bears approximately 5/6 of the weight transferred from the femur with the slender fibula serving mainly for muscle attachments.
(See Figure 2)
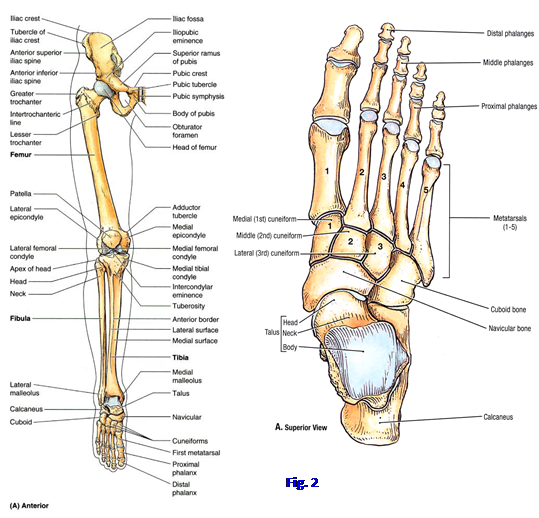
The bones of the foot are 7 tarsal bones, 5 metatarsal bones, and 14 phalanges (Fig. 2; Gr 5.68A; Table 5.8 [p. 405]; Ne 511, 512). The tarsal bones are the talus, calcaneus, cuboid, navicular, and three cuneiform bones. The talus articulates inferiorly with the calcaneus and anteriorly with the navicular bone. The medial (1st), intermediate (2nd), and lateral (3rd) cuneiform bones are located between the navicular bone posteriorly and the medial three metatarsal bones anteriorly. The cuboid bone is situated laterally between the calcaneus and the fourth and fifth metatarsal bones. It articulates medially with the navicular and lateral cuneiform bones.
The metatarsal bones and digits are numbered 1-5 beginning on the side of the great toe (Fig. 2; Gr 5.68; Ne 511). The great toe has only proximal and distal phalanges, but each of the lateral four toes has three phalanges—proximal, middle, and distal.
The lower extremity is subdivided into regions based on skeletal landmarks (Fig. 1; Gr 5.1; Ne 469). The hip (hip region) is located between the iliac crest and the greater trochanter of the femur. Some authors prefer to use the gluteal region in place of the hip as the transitional region between the trunk and lower extremity. The gluteal region lies posteriorly between the iliac crest above and a fold of skin, the gluteal fold, underlying the buttock. The thigh is the region between the greater trochanter of the femur and the knee. It contains most of the femur. The leg extends from the knee to the ankle joint. The skeleton of the leg is formed by the medial tibia and the lateral fibula. (Note: a layperson frequently refers to the entire lower extremity as “the leg,” but that is unacceptable terminology for health care professionals.) The foot is the part of the lower extremity distal to the ankle joint that makes contact with the ground. It is formed by 7 tarsal bones, 5 metatarsal bones, and 14 phalanges. The superior surface of the foot is the dorsum, and the part that contacts the ground is the plantar surface (sole).(See Figure 3)
BONES OF THE HIP AND THIGH
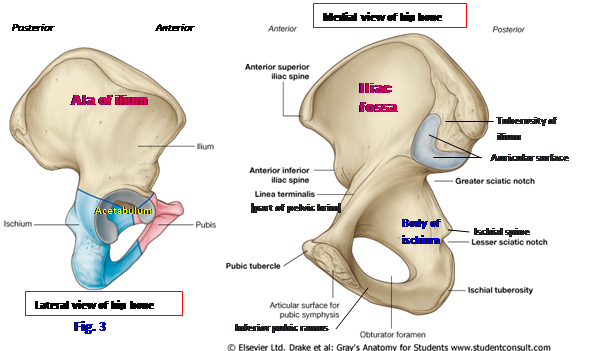
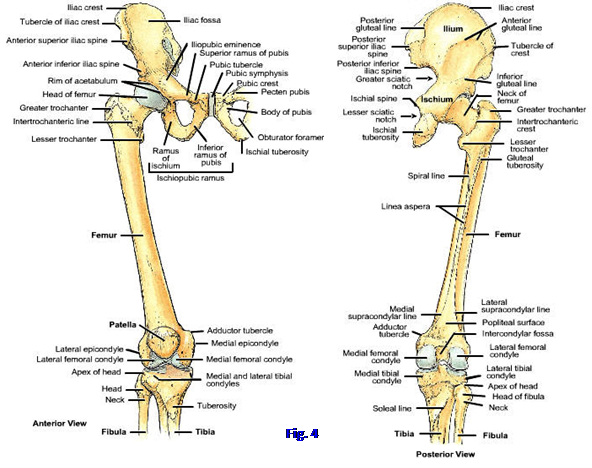
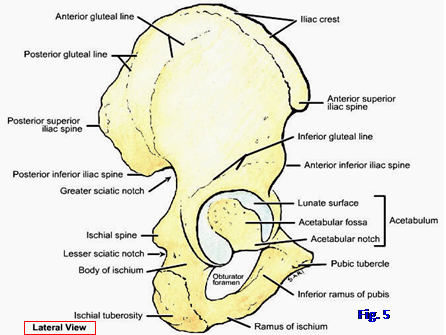
The ilium is the largest part of the hip bone. It consists of a wing-like superior portion, the ala of the ilium, and an inferior portion that fuses in the acetabulum, the body of the ilium. The ala of the ilium has a large, shallow depression medially, the iliac fossa (Figs. 3, 4; Gr 3.1, 3.2, 5.20A; Ne 332, 474). Laterally, the ala has three rough ridges, the posterior, anterior, and inferior gluteal lines (Figs. 4, 5; Gr 5.20C, 5.26A, 5.31A; Ne 336, 474). The thickened superior border of the ala is the iliac crest, which extends between two prominences, the anterior superior iliac spine (ASIS) and the posterior superior iliac spine (PSIS). About 6 cm posterior to the ASIS on the iliac crest is a prominence, the tubercle of the iliac crest (Gr 5.20A & C; Ne 332, 474). The highest point of the iliac crest lies at the level of the fourth lumbar vertebra and is a useful landmark in performing a lumbar puncture to collect cerebrospinal fluid for analysis or to inject anesthetic (spinal block). A contusion of the bone of the iliac crest is a “hip pointer.” The ASIS is frequently avulsed by the sartorius muscle in skeletally immature athletes. There are less prominent anterior inferior and posterior inferior iliac spines below their respective superior iliac spines (Ne 474).
(See Figure 4)
Posterior to the iliac fossa on the medial side of the ilium is an articular surface with a shape roughly resembling an ear (Fig. 3; Gr 3.1C, 4.16A, 4.18A; Ne 474). This auricular surface articulates with the sacrum in the synovial portion of the sacroiliac joint. Posterior and superior to the auricular surface is a heavy, roughened area, the iliac tuberosity, which participates in the syndesmotic (fibrous) part of the sacroiliac joint. Extending anteriorly and inferiorly from the auricular surface is the arcuate line. It joins with a sharp ridge on the pubic bone (pecten pubis or pectineal line) and the pubic crest anteriorly and with the sacral ala and promontory posteriorly to form the pelvic brim (border of the pelvic inlet) separating the false and true pelves (Gr 3.2B, 3.3A; Ne 332, 333, 336).
The ischium forms the posteroinferior part of the hip bone (Figs. 3, 4, 5; Gr 3.1C, 5.20C; Ne 474). It consists of a body and a ramus. The body of the ischium is the superior part of the bone that fuses with the ilium and pubis to form the acetabulum. Projecting from the posterior border of the body of the ilium is the triangular ischial spine separating two notches, a large greater sciatic notch superior to the spine and a smaller lesser sciatic notch inferior to it. The ischial spine of the articulated pelvis gives attachment to the sacrospinous ligament, which separates the greater and lesser sciatic foramina (Gr 3.3A & D, 5.26, 5.27; Ne 335, 336).
(See Figure 5)
The ischial tuberosity is a thick, roughened prominence on the posterior surface of the lower body (Figs. 3, 4, 5; Gr 5.1, 5.20C, 5.26A, 5.31A; Ne 332, 333, 336, 474-476). The two ischial tuberosities are the weight-bearing parts of the skeleton in a seated position and give attachment to the hamstring muscles. They may be avulsed by forceful contractions of the hamstring muscles in skeletally immature individuals. Decubitus ulcers (pressure sores) may develop over them in debilitated or paraplegic patients. The ramus of the ischium curves anteriorly and superiorly from the tuberosity to fuse with the inferior ramus of the pubis in the ischiopubic ramus. The ischiopubic ramus helps enclose the obturator foramen.
The pubic bone (pubis) forms the anteroinferior part of the hip bone (Figs. 3, 4, 5; Gr 3.1, 3.2A, 5.20A, 5.31; Ne 332, 333, 474). It consists of a body with superior and inferior rami projecting from it. The body of the pubis articulates with the body of the contralateral pubis at the fibrocartilaginous pubic symphysis. A ridge on the anterosuperior part of the body is the pubic crest, which ends laterally in the pubic tubercle. The pubic tubercle is the medial attachment of the inguinal ligament.
The superior pubic ramus extends laterally from the body of the pubis to help form the acetabulum (Figs. 3, 4, 5; Gr 5.20A, 5.30A, 5.31; Ne 336, 474). The superior ramus’ junction with the ilium is marked by a roughened raised area, the iliopubic eminence (Gr 3.1A & C, 5.20A; Ne 332, 474, 475). The posterior margin of the superior ramus has a thin, sharp ridge, the pecten pubis (pectineal line), which joins the arcuate line of the ilium to form the linea terminalis, a part of the pelvic brim (Fig. 3; Gr 3.1, 3.2B, 3.3; Ne 332, 333, 474).
The inferior pubic ramus descends from the body of the pubis in a slight posterolateral direction to fuse with the ischial ramus. The ischiopubic ramus thus formed helps bound the obturator foramen (Figs. 3, 5; Gr 3.1C, 5.20A, 5.31A; Table 3.1 [pp. 190-191]; Ne 332, 336, 474).
The acetabulum is a large cup-shaped socket on the lateral side of the hip bone, which is made deeper by a fibrocartilaginous acetabular labrum. The acetabulum is formed by fusion of the bodies of the ilium and the ischium and the superior ramus of the pubis (Figs. 3, 5; Gr 5.30, 5.31; Ne 336, 474, 475). The margin of the socket is deficient inferiorly at the acetabular notch. The acetabulum has a smooth semilunar lunate surface covered by articular cartilage. The lunate surface mostly surrounds a central non-articular depression, the acetabular fossa. The lunate surface articulates with the head of the femur at the hip joint (Fig. 4; Gr 5.30, 5.32, 5.35; Ne 475).
The neck of the femur joins the shaft at an angle, the angle of inclination, which changes during life but averages 126° in adults. A pathological decrease in the angle of inclination is coxa vara and an increase is coxa valga. The angle of inclination, although allowing greater movement at the hip joint, also imposes a great deal of stress on the neck of the weight-bearing femur. The femoral neck is a site of frequent fracture in elderly individuals, particularly postmenopausal women with osteoporosis. An intracapsular fracture of the femoral neck (“broken hip”) in adults often interrupts the blood supply to the femoral head, resulting in avascular necrosis of the head and necessitating hip replacement surgery (e.g., http://www.emedicine.com/emerg/topic198.htm ). That is because retinacular branches of the medial femoral circumflex artery, the main blood supply to the femoral head in the adult, course along the femoral neck and are torn by the fracture (Gr 5.34; Ne 492). Hip fracture in older adults affects not only their quality of life but is associated with a 15-20% increase in mortality within one year.
A second angle associated with the head and neck of the femur is the angle of torsion. When one sights down the length of the femur from above, it is obvious that a line drawn through the center of the head and neck of the femur isn’t parallel to a line drawn through the center of the two femoral condyles. In other words, during development the head and neck of the femur rotated slightly forward on the shaft. The angle of inclination and the angle of torsion contribute to mobility at the hip joint.
Two bony prominences at the junction of the neck and shaft of the femur are the greater and lesser trochanters (Figs. 1, 2, 4; Gr 5.1, 5.20A & C, 5.29A; Ne 475-477). The greater trochanter is the large, superolateral prominence that is used as the boundary between the hip and thigh regions. It is the site of attachment of the major abductor muscles of the thigh, the gluteus medius and gluteus minimus muscles. The medial surface of the greater trochanter features a depression, the trochanteric fossa, which is the site of attachment of several lateral rotator muscles of the thigh. The greater trochanter may be fractured by direct trauma or may be avulsed by the gluteus medius and minimus muscles in skeletally immature individuals.
The smaller lesser trochanter of the femur projects medially from the posteromedial part of the junction of the neck and shaft (Fig. 4; Gr 5.20A & C, 5.27, 5.29; Ne 475-477). It is the site of insertion of the powerful iliopsoas muscle, which occasionally avulses the lesser trochanter in skeletally immature individuals. The lesser trochanter also may be avulsed following weakening by an infection or metastatic tumor (e.g., http://www.ajronline.org/cgi/content/full/178/2/423 ). The greater and lesser trochanters are joined by a roughened intertrochanteric line anteriorly and a more prominent intertrochanteric crest posteriorly (Gr 5.20A & C, 5.29; Ne 475, 477). The intertrochanteric line provides attachment to a thickening of the articular capsule of the hip joint, the iliofemoral ligament (Gr 5.29A; Ne 475). The intertrochanteric crest has a slight rounded elevation near its middle, the quadrate tubercle, for attachment of the quadratus femoris muscle (Gr 5.20C-D, 5.23C-D, 5.26A; Ne 477, 479, 483). While the intertrochanteric line provides attachment to the articular capsule of the hip joint anteriorly, the posterior part of the joint capsule ends on the neck of the femur medial to the intertrochanteric crest (Gr 5.29C-D; Ne 475).
The shaft of the femur is slightly convex anteriorly. It is smooth and rounded in cross-section except for a rough vertical ridge posteriorly, the linea aspera (Fig. 4; Gr 5.20C-D; Ne 477, 479). In the middle third of the shaft, the linea aspera has distinct medial and lateral margins, the medial and lateral lips of the linea aspera. The lateral lip of the linea aspera is continuous superiorly with a rough ridge ascending toward the greater trochanter, the gluteal tuberosity, where the gluteus maximus muscle attaches. The medial lip is continuous superiorly with a ridge that ascends to the medial surface of the shaft below the lesser trochanter, the spiral line. Between the diverging gluteal tuberosity and spiral line is an intermediate ridge passing from the linea aspera toward the base of the lesser trochanter, the pectineal line of the femur. In the inferior third of the shaft, the medial and lateral lips of the linea aspera diverge as the medial and lateral supracondylar lines, respectively.
(See Figure 6)
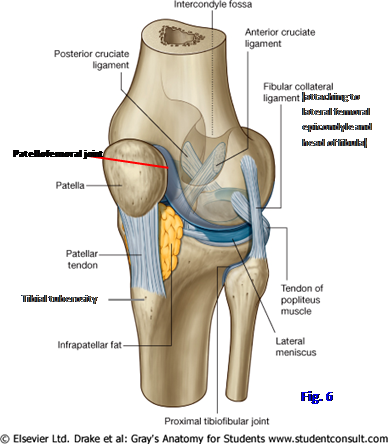
The distal end of the femur is formed by rounded medial and lateral femoral condyles (Fig. 4; Gr 5.20A & C, 5.43, 5.44A-B, 5.45A; Ne 477, 495-497). Their smooth articular surfaces merge anteriorly in a shallow groove for articulation with the patella (kneecap) at the patellofemoral joint (Fig. 6; Gr 5.43, 5.44, 5.49; Ne 477, 497, 499). Posteriorly the femoral condyles are separated by a deep intercondylar fossa, which is traversed by the cruciate ligaments of the knee joint (Gr 5.20C, 5.44A, 5.45A, 5.50A-B; Ne 477, 496, 497). Each femoral condyle has a roughed surface on its side, the medial and lateral epicondyles. The epicondyles give attachment to the tibial and fibular collateral ligaments of the knee joint, respectively (Fig. 6). The medial epicondyle has a slight prominence pointing superiorly, the adductor tubercle, for attachment of the adductor magnus muscle of the thigh (Gr 5.20, 5.23D; Ne 477, 481).
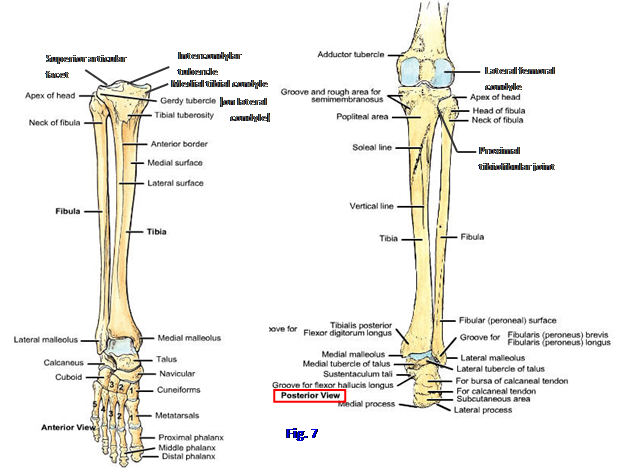
The tibia is the medial, weight-bearing bone of the leg (Figs. 1, 7; Gr 5.1, 5.20A & C, 5.60B; Table 5.8 [p. 405]; Ne 501, 502). It has expanded proximal and distal ends joined by a shaft. The wide proximal end of the tibial has prominent medial and lateral condyles, each with a superior articular facet (tibial plateau) for articulation with the corresponding femoral condyle in formation of the knee joint (Gr 5.43, 5.46A, 5.49A; Ne 497, 501, 502). In the intact knee joint, the tibial and femoral condyles are partially separated by crescent-shaped fibrocartilaginous discs, the medial and lateral menisci (Fig. 6; 5.45A, 5.46B, 5.50; Ne 495-497, 499), which help to distribute weight evenly and reduce wear on articular cartilage. The superior articular surfaces of the tibia are separated by an intercondylar eminence formed, in part, by medial and lateral intercondylar tubercles and bounded by roughened anterior and posterior intercondylar areas. The intercondylar tubercles fit into the intercondylar fossa between the femoral condyles (Fig. 7, Posterior; Gr 5.20C, 5.39, 5.49A; Ne 477, 498, 501).
(See Figure 7)
The lateral tibial condyle has a slight anterolateral prominence, the anterolateral tibial (Gerdy’s) tubercle due to attachment of the iliotibial tract there (Fig. 7; Gr 5.8B, 5.22, 5.42; Ne 501-503, 509). An articular facet for the head of the fibula is directed laterally and slightly posteriorly from the inferior surface of the lateral condyle. This is the site of the superior (proximal) tibiofibular joint (Figs. 6, 7; Gr 5.20A & C, 5.45A, 5.50A & C, 5.54B-C; Ne 497, 501, 502).
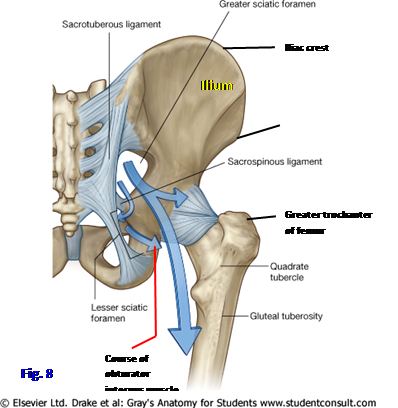 (See Figure 8)
(See Figure 8)
The anterior surfaces of the medial and lateral tibial condyles converge in a large triangular area. Bordering this triangular area at the upper end of the anterior border of the shaft of the tibia is a protuberance of variable size, the tibial tuberosity (Fig. 7; Gr 5.20A, 5.40; Ne 501, 502). The tibial tuberosity is the attachment site of the patellar ligament (quadriceps femoris tendon) connecting the tuberosity to the patella (Fig. 6; Gr 5.20B, 5.40, 5.41, 5.42; Ne 502, 503, 507). The tibial tuberosity may be quite large in individuals who suffered traction apophysitis of the tibial tuberosity during adolescence (Osgood-Schlatter disease). Alternatively, the tibial tuberosity may be avulsed by the quadriceps femoris muscle in young athletes.
The hip bone is bound to the sacrum by two strong ligaments that define foramina (Fig. 8; Gr 3.3A & D, 5.26, 5.27, 5.29C; Ne 335, 336). The sacrospinous ligament runs between the sacrum and the ischial spine, forming the lower boundary of the greater sciatic foramen and the upper boundary of the lesser sciatic foramen. The sacrotuberous ligament attaches to the sacrum and the ischial tuberosity to form the lower boundary of the lesser sciatic foramen. The greater sciatic foramen connects the gluteal region and the pelvis, while the lesser sciatic foramen is a passageway between the gluteal region and the perineum. Structures that traverse those foramina will be described below.
1. Study the gluteal region of a skeleton or articulated pelvis. Identify the spine and tuberosity of the ischium. Determine the locations of the sacrospinous and sacrotuberous ligaments. Visualize the positions of the greater and lesser sciatic foramina.
2. Examine the cup-shaped acetabulum, where the head of the femur articulates to form the hip joint. Note the contributions of the three bones—ilium, ischium, and pubis—that fuse in the acetabulum to form the hip bone (Fig. 3; Gr 5.31B; Ne 474). XXX
The gluteal region contains three large gluteal muscles and several smaller muscles (Figs. 9, 10; Gr 5.23; Tables 5.4, 5.5 [pp. 368-369]; Ne 479, 482, 483). The most superficial of the gluteal muscles is also the largest, the gluteus maximus. It passes from the posterior surface of the ilium, sacrum, coccyx, and sacrotuberous ligament to the iliotibial tract and gluteal tuberosity of the femur. Three-fourths of the muscle inserts into the iliotibial tract, and only the lower half of the deep portion inserts into the femur. The gluteus maximus is a powerful extensor of the thigh (e.g., when standing up from a seated position and walking up stairs) but is little used during ordinary walking. Through its insertion into the iliotibial tract (Gr 5.22; Ne 482), it may play a role in keeping the extended knee in extension.
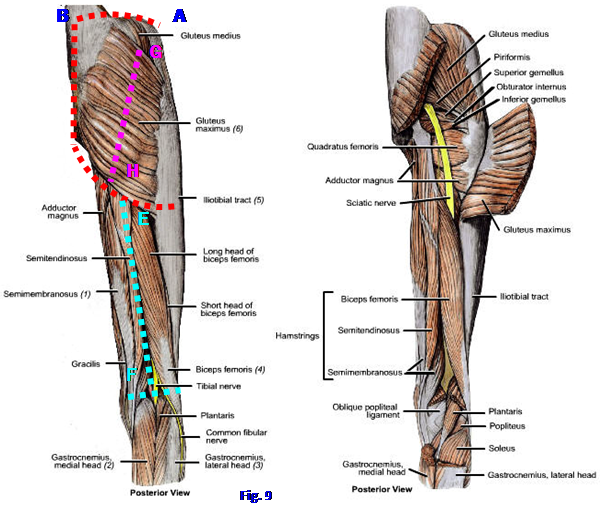 (See Figure 9)
(See Figure 9)
The inferior border of the gluteus maximus slides superiorly when we sit (hip flexion). Therefore, we sit on our ischial tuberosities, not on our gluteus maximus muscles. The tissue over the ischial tuberosity is a frequent site for the development of pressure (decubitus) ulcers in paraplegic and debilitated patients. The gluteus maximus is innervated by the inferior gluteal nerve (L5, S1, S2) and receives its blood supply from the inferior gluteal artery and the superficial branch of the superior gluteal artery (Gr 5.25; Ne 490).
Fibers of the gluteus maximus are separated from the greater trochanter of the femur by the large trochanteric bursa (Gr 5.24A) and from the ischial tuberosity by a smaller ischial bursa. Repetitive movements that cause the gluteus maximus to move back and forth over the trochanteric bursa (e.g., repeatedly walking up and down stairs carrying a heavy load) result in a friction bursitis (trochanteric bursitis). This condition is characterized by tenderness over the greater trochanter and pain that may radiate a variable distance down the iliotibial tract. The iliotibial band also may be irritated by friction as it moves over the greater trochanter (iliotibial band syndrome).
3. Make incisions through the skin and superficial fascia along the iliac crest from the ASIS to the PSIS (A⇒B), along the gluteal sulcus (C⇒D), and down the sacroiliac junction (B⇒C) (Fig. 9). Remove the skin and superficial fascia. Incise the skin down the middle of the posterior thigh (E⇒F) and make cuts to both sides of the lower end. Reflect the flaps laterally. The usually thick subcutaneous fat of the gluteal region contains cutaneous nerves, the superior clunial (L1-3), middle clunial (S1-3), and inferior clunial (S1-3) nerves, which are formed by fibers in the posterior rami of spinal nerves (Gr 5.3B; Ne 472). Be aware of their distribution but don’t spend time looking for them. There is also a lateral cutaneous branch of the iliohypogastric nerve (L1) descending over the iliac crest toward the greater trochanter but don’t dissect it. As part of the lumbar plexus, the iliohypogastric nerve is an anterior ramus.
4. Remove any remaining subcutaneous fat overlying the gluteus maximus muscle. Mobilize the superior and inferior borders of the gluteus maximus so that you can pass your fingers deep to the edges of the thick muscle. Make an incision through the thickness of the gluteus maximus from the middle of the superior border to the middle of the inferior border (G⇒H) (Fig. 9). As you reflect the two halves of the gluteus maximus, attempt to the preserve some branches of the inferior gluteal nerve and artery entering the muscle’s deep surface (Gr 5.25; Ne 490). Look also for the superficial branch of the superior gluteal artery entering the upper part of the deep surface. Under the lateral half of the gluteus maximus, look for the thin-walled trochanteric bursa separating it from the greater trochanter of the femur (Gr 5.24). XXX
The fan-shaped gluteus medius is partly hidden by the upper portion of the gluteus maximus and by thick overlying gluteal fascia (Fig. 9; Gr 5.22, 5.23B-C, 5.33; Table 5.4 [p. 368]; Ne 483, 490). The gluteus medius arises between the anterior and posterior gluteal lines of the ilium and from the overlying gluteal fascia and passes distally to attach to the greater trochanter of the femur (Gr 5.20C-D; Ne 474, 479).
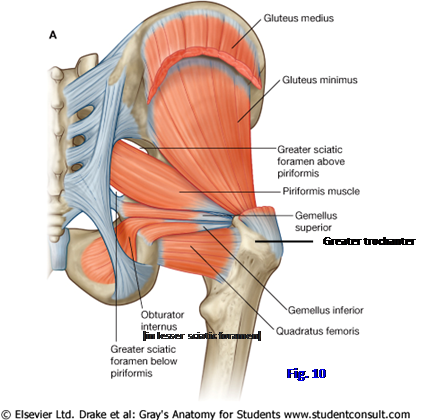
The smaller gluteus minimus lies deep to the gluteus medius (Fig. 10; Gr 5.20C-D, 5.23B-C, 5.25; Ne 474, 479, 483). It passes from the external surface of the ilium between the anterior and inferior gluteal lines to the greater trochanter of the femur anterior to the attachment of the gluteus medius. The gluteus medius and minimus muscles work together to abduct the thigh and to rotate it medially. They are innervated by the superior gluteal nerve (L4, L5, S1), which courses laterally deep to the gluteus medius, in the fascial interval between it and the gluteus minimus (Gr 5.25; Ne 491).
Weakness of the gluteus medius and minimus muscles or a superior gluteal nerve lesion result in dropping of the unsupported side of the pelvis when the patient stands on one foot on the affected side (positive Trendelenburg sign). There is a characteristic gluteus medius gait in which the patient leans the trunk toward the affected side when bearing weight on it during the stance phase. Avulsion of the greater trochanter of the femur results in similar signs.
The tensor fasciae latae is another abductor muscle of the thigh innervated by the superior gluteal nerve (Gr 5.17; Table 5.2 [p. 358]; Ne 482). However it is located in the anterior thigh and will be dissected with that region.
The smaller muscles of the gluteal region located deep to the gluteus maximus are the piriformis, obturator internus, superior and inferior gemelli, and the quadratus femoris (Figs. 9, 10; Gr 5.23C-D, 5.24-5.27; Table 5.5 [p. 368]; Ne 483, 490, 491). The piriformis is the principle muscular landmark of the gluteal region. It passes from the anterior surface of the sacrum within the pelvis through the greater sciatic foramen to the upper border of the greater trochanter of the femur. The superior gluteal nerve and vessels traverse the greater sciatic foramen superior to the piriformis, and the inferior gluteal nerve and vessels traverse the foramen inferior to the piriformis (Gr 5.25; Ne 490, 491). Other nerves and vessels pass inferior to the piriformis as described below.
The obturator internus muscle takes origin from the internal surface of the obturator membrane and the margins of the obturator foramen (Fig. 10; Gr 5.27; Ne 340, 479, 483, 491). It traverses the lesser sciatic foramen to insert into the trochanteric fossa on the medial side of the greater trochanter. The small superior and inferior gemelli muscles are closely related to the obturator internus and insert mainly into its tendon but also into the trochanteric fossa. The superior gemellus takes origin from the ischial spine. The inferior gemellus takes origin from the ischial tuberosity. It isn’t unusual for a gemellus muscle to be congenitally absent. When both gemelli are present, they join the obturator internus in forming the triceps coxae muscle. The obturator internus and superior gemellus are innervated by the nerve to the obturator internus (L5, S1, S2) (Gr Table 5.6 [p. 374]; Ne 491). The inferior gemellus is innervated by the nerve to the quadratus femoris (L4, L5, S1).
The quadratus femoris passes transversely from the lateral border of the ischial tuberosity to the quadrate tubercle of the femur (Figs. 9, 10; Gr 5.23, 5.25, 5.26; Ne 483, 491). It is a short, thick, rectangular muscle located just inferior to the inferior gemellus. The quadratus femoris is innervated by the nerve to the quadratus femoris.
The piriformis, obturator internus and gemelli, and the quadratus femoris laterally rotate the femur. If the thigh is flexed at the hip joint, all except the quadratus femoris may help to abduct the thigh, but abduction is mainly due to the actions of gluteus medius and minimus.
The superior (L1-3), middle (S1-3), and inferior (S1-3) clunial (cluneal) nerves are cutaneous nerves of the gluteal region that may have been seen earlier (Gr 5.3B; Ne 472). The clunial nerves may be damaged in harvesting bone from the ilium for grafting.
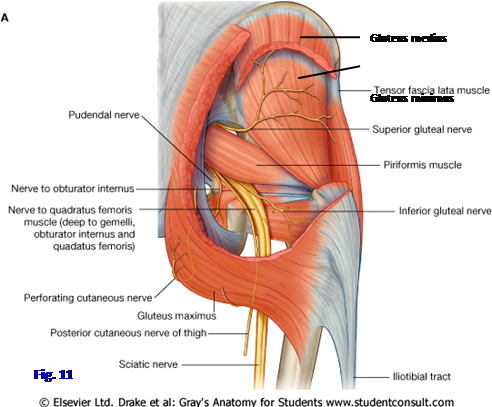
The superior gluteal nerve (L4, L5, S1) emerges from the greater sciatic foramen above the piriformis muscle (Fig. 11; Gr 5.25; Ne 490). It passes laterally in the fascial interval between the gluteus medius and gluteus minimus with the deep branch of the superior gluteal artery. The superior branch of the superior gluteal nerve supplies only the gluteus medius. The inferior branch supplies both the gluteus medius and minimus and continues anteriorly to innervate the tensor fasciae latae. A lesion of the superior gluteal nerve results in weakness abducting the thigh and a positive Trendelenburg sign. The patient also has difficulty in medial rotation of the thigh.
The inferior gluteal nerve (L5, S1, S2) traverses the greater sciatic foramen inferior to the piriformis muscle (Fig. 11; Gr 5.24, 5.25; Ne 490, 491). It divides into multiple branches to supply the large gluteus maximus. The inferior gluteal nerve is accompanied by the inferior gluteal artery and vein. A lesion of the inferior gluteal nerve results in weakness during resisted extension of the thigh, as in standing up from a seated position or walking up stairs, both of which are resisted by gravity. An inferior gluteal lesion has little or no effect on ordinary walking on level ground because the hamstring muscles can extend the thigh during this motion.
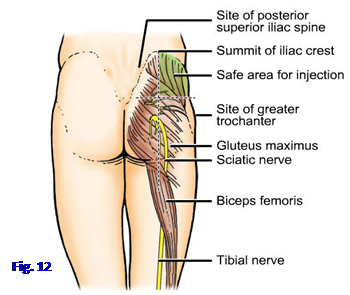
The sciatic nerve (L4-S3) is the largest nerve in the body (Figs. 9, 11; Gr 5.23A & C, 5.24-5.26; Tables 5.1 [p. 349]; Ne 490, 491, 528). It leaves the greater sciatic foramen inferior to the piriformis muscle, slightly lateral and deep to the inferior gluteal nerve. The sciatic nerve descends deep to the gluteus maximus midway between the ischial tuberosity and greater trochanter. It supplies no structures in the gluteal region before emerging into the posterior thigh, where it supplies the hamstring muscles. Branches of the sciatic nerve supply the joints of the lower extremity other than the hip joint and all of the muscles below the knee, so injury to the nerve by an improperly placed gluteal injection or a posterior dislocation of the hip joint causes major functional deficits. An intramuscular injection in the gluteal region can only be made safely in the superior lateral quadrant (Fig. 12). The sciatic nerve receives the artery to the sciatic nerve from the inferior gluteal artery (Gr 5.28B; Ne 490). Occasionally this artery is large, and the femoral artery (of the anterior thigh) is correspondingly smaller
The sciatic nerve is really two nerves, the tibial nerve and common fibular nerve (formerly common peroneal nerve), bound together by connective tissue epineurium (Ne 487). In about 12-15% of the population the two nerves emerge separately from the greater sciatic foramen with the common fibular division passing through the piriformis muscle or superior to it (Gr 5.26B). The muscle may compress the nerve to produce pain in the buttock and posterior thigh (piriformis syndrome, e.g., see http://www.emedicine.com/pmr/topic106.htm ). Individuals in whom the common fibular nerve pierces the piriformis muscle or passes above it are predisposed. Hypertrophy of the piriformis muscle, producing piriformis syndrome, is more likely in some sports (e.g., skiers, tennis players). Blunt trauma followed by fibrosis may have the same result. Half of the cases of piriformis syndrome are idiopathic.
Another large nerve that enters the gluteal region below the piriformis muscle is the posterior femoral cutaneous nerve (posterior cutaneous nerve of the thigh) from S1, S2, S3 (Fig. 11; Gr 5.3B, 5.24, 5.25; Table 5.6 [p. 374]; Ne 472, 491, 528). It has an extensive distribution to skin of the inferior part of the gluteal region (through inferior clunial branches) and of the posterior thigh and proximal part of the leg. The posterior femoral cutaneous nerve varies from most cutaneous nerves in that it descends deep to the deep fascia of the thigh (fascia lata) and only the terminal branches enter subcutaneous tissue to innervate skin. It sends a perineal branch to help innervate the scrotum or labium majus (Gr 3.44, 3.52B, 3.53; Ne 393, 491, 528). The perineal branch of the posterior femoral cutaneous nerve may be a source of continuing perineal pain during childbirth following injection of an anesthetic agent to block the pudendal and ilioinguinal nerves.
Three other small nerves emerge below the piriformis (Fig. 11; Gr 5.24, 5.25; Table 5.6 [p. 374]; Ne 491). From medial to lateral are the pudendal nerve, nerve to the obturator internus, and nerve to the quadratus femoris. The pudendal nerve (S2-4) has a short course through the gluteal region accompanied by the internal pudendal artery and vein. The nerve enters the gluteal region from the pelvis through the greater sciatic foramen and leaves it through the lesser sciatic foramen to enter the perineum. The pudendal nerve is the main nerve of the perineum and will be studied later.
The nerve to obturator internus (L5-S2) also enters the gluteal region through the greater sciatic foramen and leaves it through the lesser sciatic foramen (Fig. 11; Gr 5.24, 5.25; Ne 491). It sends a small branch to the superior gemellus before traversing the lesser sciatic foramen to pierce the medial surface of the obturator internus.
The nerve to quadratus femoris (L4-S1) leaves the pelvis anterior to the sciatic nerve and passes over the posterior surface of the hip joint deep to the obturator internus and gemelli (Ne 491). It gives an articular branch to the joint and supplies the inferior gemellus and quadratus femoris muscles.
The arteries of the gluteal region arise from the internal iliac arteries (Gr Tables 3.3 [pp. 212-213], 3.5 [pp. 234-235]; Ne 382, 383). The superior gluteal artery is the largest branch of the internal iliac. It traverses the greater sciatic foramen superior to the piriformis muscle and divides into superficial and deep branches (Gr 3.10, 5.24, 5.25; Ne 490). The superficial branch of the superior gluteal artery supplies the upper part of the gluteus maximus muscle. The deep branch accompanies the superior gluteal nerve deep to the gluteus medius to supply it, the underlying gluteus minimus, and the tensor fasciae latae.
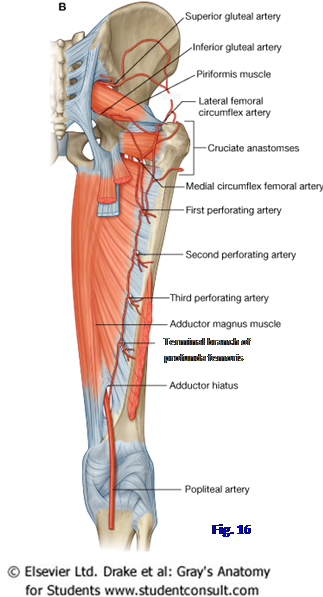
The inferior gluteal artery exits the pelvis through the greater sciatic foramen inferior to the piriformis. It supplies the inferior part of the gluteus maximus and the small inferior muscles of the gluteal region. The inferior gluteal artery often anastomoses with the medial and lateral femoral circumflex arteries and the first perforating artery (from the profunda femoris) to form the cruciate anastomosis (Gr 5.9B, 5.28A). When it is present, the cruciate anastomosis allows safe ligation of the femoral artery.
The internal pudendal artery branches from the internal iliac artery and follows the pudendal nerve into the gluteal region (Gr 3.24, 5.24, 5.25; Table 3.3 [p. 212]; Ne 382, 383). It does not supply structures in the gluteal region before entering the perineum, where it will be studied.
5. Identify and clean the piriformis muscle traversing the greater sciatic foramen to attach to the greater trochanter (Gr 5.25, 5.26A; Ne 483, 490). Look for the superficial branch of the superior gluteal artery (perhaps now torn) emerging between the piriformis and the gluteus medius muscles to enter the superior part of the gluteus maximus. Again find the inferior gluteal nerve and artery passing below the piriformis to reach the lower part of the gluteus maximus. If the medial half of the gluteus maximus was not completely reflected earlier, do so now.
6. Clean the gluteal fascia from the gluteus medius muscle. Cut the gluteus medius 5 cm inferior and parallel to the iliac crest. Reflect the muscle downward toward the greater trochanter. The gluteus mimimus is now exposed. In the fascial interval between the gluteus medius and minimus, clean the superior gluteal nerve and deep branch of the superior gluteal artery.
7. Clean the large sciatic nerve and the more medial posterior femoral cutaneous nerve emerging inferior to the piriformis muscle. Verify the course of the sciatic nerve close to the posterior aspect of the hip joint and halfway between the ischial tuberosity and greater trochanter (Figs. 9, 11, 12). Does the common fibular division of the sciatic pass above or through the piriformis muscle in the gluteal region on either side of the cadaver? Follow the sciatic nerve inferiorly until it disappears deep to the long head of the biceps femoris muscle.
8. Follow the posterior femoral cutaneous nerve to where it disappears deep to the fascia lata. Be aware of, but don’t attempt to find, the inferior clunial and perineal branches of the posterior femoral cutaneous nerve. The inferior clunial nerves curve upward around the inferior border of the gluteus maximus muscle to reach subcutaneous tissue of the lower part of the gluteal region. The perineal branch of the posterior femoral cutaneous nerve passes medially.
9. Identify the obturator internus muscle and tendon. The tendon may be hidden by the insertion of the gemelli. If you have trouble identifying the obturator internus, palpate the ischial spine just below the piriformis and then insert the tip of a finger into the lesser sciatic foramen just below the ischial spine and sacrospinous ligament. Your finger is now on the belly of the obturator internus. Following the muscle laterally by palpation, you should be able to distinguish the firm tendon as it passes to the trochanteric fossa of the femur. Clean the superior gemellus arising from the ischial spine and the inferior gemellus from the ischial tuberosity. Separate the attachments of the gemelli from the obturator internus tendon distally to expose the tendon.
10. Below the inferior gemellus find the rectangular quadratus femoris muscle. The sciatic and posterior femoral cutaneous nerves descend across its posterior surface. Spread apart the lower border of the inferior gemellus and the upper border of the quadratus femoris to expose the tendon of the obturator externus, which originates in the medial (adductor) compartment of the thigh (Gr 5.27, 5.29; Gr 489) and will be studied during the next lab.
11. Look for the nerve to the obturator internus entering the gluteal region via the greater sciatic foramen (Gr 5.24, 5.25; Ne 490, 491). Follow the nerve onto the surface of the obturator internus muscle and into the lesser sciatic foramen. Be aware that the nerve sends a branch to the superior gemellus but don’t attempt to find it. The small nerve to the quadratus femoris is usually difficult to find but be aware of it. A short segment of the nerve may be visible descending in the interval between the piriformis and superior gemellus muscles lateral to the nerve to the obturator internus. XXX
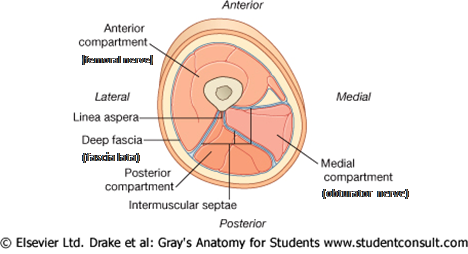
The thigh is the part of the lower extremity between the greater trochanter of the femur and the knee joint (Fig. 1). Muscles of the thigh are enclosed by the deep fascia of the thigh, the fascia lata. Thigh muscles are separated into three compartments by intermuscular septa that pass from the deep surface of the fascia lata to the linea aspera of the femur (Fig. 13; Gr 5.8A & D; Ne 493). The three compartments are a posterior (flexor) compartment, medial (adductor) compartment, and anterior (extensor) compartment. They are designated according to their position or the major action of their muscles at the knee joint. In general, the posterior thigh muscles are innervated by the tibial division of the sciatic nerve, the medial thigh muscles by the obturator nerve, and the anterior thigh muscles by the femoral nerve.
(See Figure 13)
The anterior and medial compartments will be studied during the next period. The posterior compartment of the thigh contains the three hamstring muscles—semitendinosus, semimembranosus, and long head of biceps femoris (Fig. 9; Gr 5.23B-D; Table 5.5 [p. 369]; Ne 483). It also contains the short head of the biceps femoris, which is not considered a hamstring muscle. The hamstring muscles all take origin from the ischial tuberosity (Gr 5.20D, 5.23C; Ne 479, 483, 490), cross both the hip and knee joints (i.e., they are two-joint muscles, which makes them more susceptible to injury), and are innervated by the tibial division (L4-S3) of the sciatic nerve. The hamstring muscles extend the thigh and flex the knee but, like other two-joint muscles, they cannot perform both actions effectively at the same time. The hamstrings contract eccentrically at the end of forceful flexion of the thigh (e.g., when punting a football) to decelerate the extremity. They are especially susceptible to injury during these eccentric contractions when they are stretched over both the hip and knee joints.
The semitendinosus muscle is so named because of its long tendon (Figs. 9, 14; Gr 5.23B-C, 5.36, 5.37; Table 5.5 [p. 369]; Ne 483, 490). After taking origin from the ischial tuberosity, it descends superficial to the semimembranosus muscle along the medial side of the posterior compartment of the thigh. The semitendinosus inserts on the upper medial surface of the tibia with the tendons of the gracilis and sartorius muscles (Gr 5.41; Table 5.8, Left [p. 405]; Ne 494, 495, 503). The tendons of the three muscles reminded some early anatomist (who may have stopped at a tavern on his way to the lab) of a goose’s foot; therefore, the insertion of the three tendons is the pes anserinus.
The semimembranosus consists of a broad flat tendon in its upper half, which gives the muscle its name (Fig. 14; Ne 483). The semimembranosus descends from the ischial tuberosity along the medial side of the posterior compartment deep to the semitendinosus to attach to the posterior surface of the medial tibial condyle. Its distal tendon sends a fibrous band superolaterally to reinforce the posterior part of the knee joint capsule as the oblique popliteal ligament. In addition to extending the thigh and flexing the leg, the semitendinosus and semimembranosus muscles can medially rotate the flexed leg.
The biceps femoris has two heads as the name implies (Figs. 9, 14; Gr 5.23B-D; Table 5.5 [p. 369]; Ne 482, 483, 490). The long head of the biceps femoris muscle is classified as a hamstring muscle and takes origin from the ischial tuberosity. After being joined by the short head, the biceps femoris inserts on the head of the fibula. Theactions of the long head of the biceps femoris are extension of the thigh and flexion of the knee. Along with the short head, it can laterally rotate the flexed leg.
(See Figure 14)
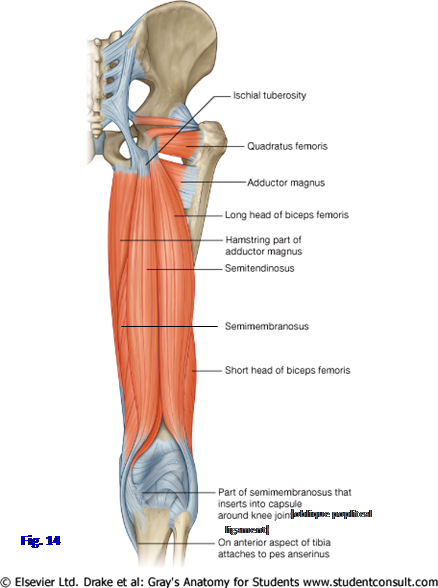
The short head of the biceps femoris crosses the knee joint but not the hip joint (Gr 5.23D; Ne 483); therefore, it is not classified as a hamstring muscle. The short head takes origin from the lower part of the lateral lip of the linea aspera and the lateral supracondylar line. The short head joins the long head to act with it at the knee joint. Unlike the hamstring muscles, the short head of the biceps femoris is innervated by the common fibular division (L4-S2) of the sciatic nerve. It has been suggested that the different innervations of the two heads of the biceps femoris may result in uncoordinated contractions and increase the likelihood of injury. (Note: since we now have studied a "biceps" muscle in both the upper [biceps brachii] and lower [biceps femoris] extremities, be sure to use the full name on the lab practical exam if one is tagged)
(See Figure 15)
The posterior femoral cutaneous nerve (posterior cutaneous nerve of the thigh) (S1-S3) was seen earlier descending from the inferior border of the gluteus maximus muscle deep to the fascia lata of the posterior thigh (Fig. 11; Gr 5.24, 5.25; Ne 472, 528). After giving off inferior clunial branches to the gluteal region and a perineal branch, the posterior femoral cutaneous continues down the thigh, giving off branches that pierce the fascia lata to enter subcutaneous tissue. It innervates most of the skin of the posterior thigh and of the posterior part of the upper leg.
(See Figure 16)
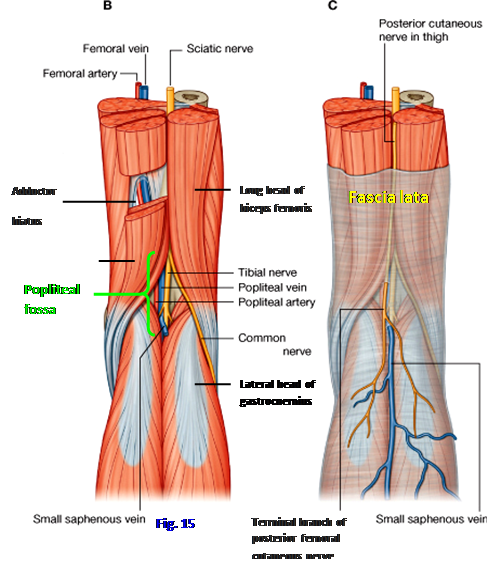
The sciatic nerve was seen descending from the gluteal region deep to the long head of the biceps femoris muscle (Gr 5.23C; Ne 490). The sciatic is formed by two nerves that are usually bound together by a connective tissue epineurium, but the level of division is quite variable—sometimes the nerves emerge separately through the greater sciatic foramen, but on average they separate in the distal thigh near the superior border of the popliteal fossa (Figs. 9, 15, 17; Gr 5.23B, 5.26B, 5.37, Table 5.1 [pp. 348-349]; Ne 483, 487, 490, 504, 528). The more medial part of the sciatic nerve is the tibial nerve formed by the anterior rami of L4-S3. It supplies the three hamstring muscles and the hamstring portion of the adductor magnus. The tibial nerve descends near the middle of the popliteal fossa as the most superficial of the three main structures in the fossa—the popliteal artery, popliteal vein, and tibial nerve (Figs. 15, 17; Gr 5.36B, 5.38, 5.62C; Ne 490, 504, 505). The tibial nerve innervates the muscles in the posterior compartment of the leg and the plantar part of the foot.
(See Figure 17)
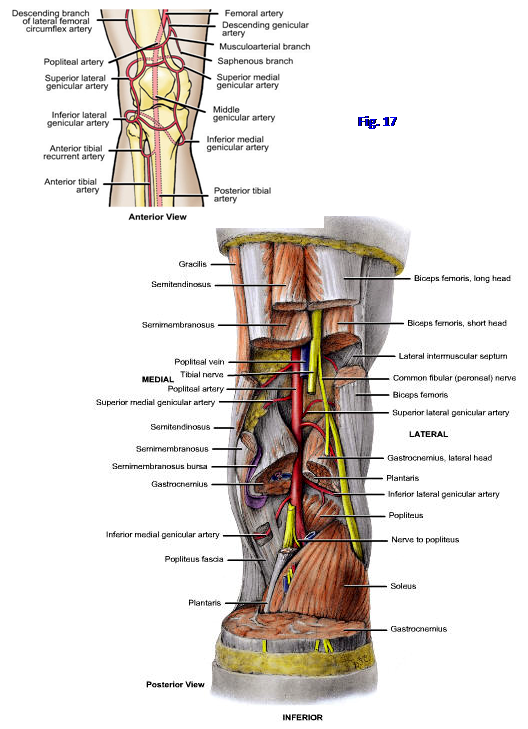
The common fibular branch of the sciatic nerve (L4-S2) descends along the inferior border of the biceps femoris belly and passes across the lateral head of the gastrocnemius muscle (Figs. 15, 17; Gr 5.61B; Ne 490, 504). It innervates the short head of the biceps femoris muscle before leaving the popliteal fossa. The common fibular nerve passes around the neck of the fibula (Gr 5.55, 5.58; Ne 494, 508, 530), where the nerve is vulnerable to injury (to be considered in a later lab). The common fibular innervates the muscles of the lateral and anterior compartments of the leg and the dorsum of the foot.
The major blood supply of the posterior compartment of the thigh is by perforating arteries (Fig. 16; Gr 5.9, 5.28, Table 5.3, Right [p. 360]; Ne 489, 490, 500) that branch from the profunda femoris artery (deep artery of the thigh) in the anterior compartment, as will be seen during the next period. The perforating arteries pierce the adductor magnus (a muscle of the medial thigh) near its attachment to the linea aspera and medial supracondylar line to enter the posterior compartment. (Note: Perforating arteries pierce the adductor magnus medial to the femur, so the figures from Grant’s Atlas are deceptive.) There typically are four perforating arteries with the fourth one being the terminal branch of the profunda femoris. The first perforating artery often anastomoses with the inferior gluteal and the medial and lateral femoral circumflex arteries to form the cruciate anastomosis (Fig. 16; Gr 5.9B, 5.28A; Ne 490). (Note: the superior gluteal artery is not considered to contribute to the cruciate anastomosis despite the appearance of Fig. 12.) The fourth perforating artery typically anastomoses with the popliteal artery in the popliteal fossa.
The deep veins accompany the arteries of the same name in the gluteal region and thigh (Gr 5.10). The superior and inferior gluteal veins and the internal pudendal vein are tributaries of the internal iliac vein. The perforating veins are tributaries of the profunda femoris vein (deep vein of the thigh) and pierce the adductor magnus with the arteries. Since some of these tributaries of the internal and external iliac veins communicate, there is an alternative route of venous return if the femoral vein becomes occluded or has to be ligated.
12. Briefly probe through the superficial fascia of the posterior thigh to find branches of the posterior femoral cutaneous nerve. Be aware of, but don’t attempt to find, other cutaneous nerves (Gr 5.3; Ne 472). Along the lateral aspect of the thigh are branches of the lateral femoral cutaneous nerve. Small cutaneous branches of the obturator nerve may pass into subcutaneous tissue of the posterior compartment along the upper medial border of the thigh.
13. Clean away any remaining superficial fascia over the posterior compartment of the thigh. The posterior femoral cutaneous nerve may be visible through the fascia lata. Incise the fascia lata down the middle of the posterior thigh and make lateral cuts at the superior and inferior ends of the first incision. Remove the flaps of fascia lata to expose the contents of the posterior compartment. Clean the posterior femoral cutaneous nerve and try to preserve it.
14. Clean the hamstring muscles. Find the semitendinosus descending from the ischial tuberosity along the medial side of the posterior thigh. Note the long tendon characteristic of the inferior part of the muscle but don’t attempt to follow it to its attachment as part of the pes anserinus at this time. Elevate the semitendinosus to get a better view of the wider semimembranosus muscle. Verify that the origin and superior half of the semimembranosus consist of a flat, wide tendon.
15. Clean the long head of the biceps femoris muscle and note that it shares a common origin from the ischial tuberosity with the semitendinosus. Follow the long head distally to where it is joined on its deep surface by the short head of the biceps femoris. Follow the tendon to the head of the fibula.
16. Clean the sciatic nerve where it emerges from deep to the long head of the biceps femoris. The point at which the sciatic nerve divides into the tibial and common fibular nerves may vary on the two sides of the body. Find the site of division but don’t follow the two branches into the popliteal fossa yet.
17. Find and clean a couple of the perforating arteries as they pierce the adductor magnus to enter the posterior compartment of the thigh. Recognize the importance of, but don’t attempt to demonstrate, the anastomosis between the first perforating artery and the inferior gluteal artery, which forms part of the cruciate anastomosis. XXX
The popliteal fossa is a diamond-shaped depression posterior to the knee joint (Figs. 9, 15; Gr 5.23B, 5.36, 5.61B; Ne 469, 483, 504). It is bounded superolaterally by the biceps femoris and superomedially by the semitendinosus and semimembranosus. The inferolateral and inferomedial boundaries are the lateral and medial heads, respectively, of the gastrocnemius muscle. The roof is formed by skin and popliteal fascia. The floor, which is clinically important, is formed, from superior to inferior, by the distal femur, the posterior capsule of the knee joint, and the popliteus fascia covering the popliteus muscle. The popliteus muscle and fascia will not be seen until the leg is dissected in a later period.
In the subcutaneous tissue overlying the popliteal fossa are the terminal branches of the posterior femoral cutaneous nerve (Fig. 15C; Gr 5.3B; Ne 472) and the termination of the small saphenous vein. The upper portions of the medial sural cutaneous nerve, a branch of the tibial nerve, and the lateral sural cutaneous nerve, a branch of the common fibular nerve, may be seen in the subcutaneous tissue overlying the lower part of the fossa.
The small saphenous vein begins laterally on the dorsum of the foot from a dorsal venous arch, passes posterior to the lateral malleolus, and ascends along the middle of the calf to pierce the popliteal fascia (Gr 5.5B-C, 5.6A, 5.36B; Ne 472, 490). It is a tributary of the popliteal vein. As with other superficial veins of the upper and lower extremities, perforating veins carry blood from the small saphenous vein through deep fascia to deep veins (Gr 5.5). This enables muscle contractions to help push the blood toward the heart against the pull of gravity (musculovenous pump).
The contents of the popliteal fossa include fatty connective tissue, the popliteal artery and vein, tibial and common fibular nerves, and popliteal lymph nodes and lymphatic vessels (Gr 5.36, 5.37, 5.38, 5.61B-C; Ne 473, 483, 504, 505). The popliteal artery is the deepest structure in the popliteal fossa. It is the continuation of the femoral artery at the adductor hiatus, a gap in the insertion of the adductor magnus muscle (Figs. 15, 16, 17; Gr 5.9B, 5.23D, 5.28A; Ne 489, 490, 500). The popliteal artery lies against the distal femur, where it may be injured by a fracture if the gastrocnemius muscle rotates the distal fragment of bone posteriorly. Likewise, rupture of a popliteal aneurysm (more frequently seen in equestrians) may result in fatal hemorrhage. Since the artery crosses the capsule of the knee joint posteriorly, dislocation of the knee joint also may damage the artery. Traumatic injury of the popliteal artery and the closely related popliteal vein (see below) may result in an arteriovenous fistula with loss of the leg and foot or more serious consequences if not promptly recognized and treated (e.g., see http://www.belsurg.org/uploaded_pdfs/107/107_208_210.pdf ).
The popliteal artery has five genicular branches that participate in a genicular anastomosis to provide collateral circulation around the knee joint (Fig. 17; Gr 5.28A, 5.38, 5.48; Ne 500, 505, 506). The genicular branches are the superior medial genicular, superior lateral genicular, inferior medial genicular, inferior lateral genicular, and middle genicular arteries. The genicular anastomosis maintains blood circulation to the leg and foot when the knee is fully flexed, which folds the popliteal artery on itself, compromising blood flow. The other vessels that contribute to the genicular anastomosis will be studied later.
The terminal branches of the popliteal artery are the anterior and posterior tibial arteries (Gr 5.9, 5.48; Table 5.11 [p. 423]; Ne 500, 506). They arise from division of the popliteal artery at the inferior border of the popliteus muscle. The anterior tibial artery passes through a gap in the superior part of the interosseous membrane, which unites the tibia and fibula, to enter the anterior compartment of the leg. The larger posterior tibial artery continues inferiorly into the deep posterior compartment of the leg and will be studied later.
The popliteal vein courses superficial to the artery in the popliteal fossa (Fig. 15; Gr 5.38, 5.62C; Ne 490, 504, 505). It is formed by the union of the anterior and posterior tibial veins and receives the small saphenous vein as a tributary. The other tributaries of the popliteal vein generally correspond to branches of the popliteal artery. The popliteal vein ascends through the adductor hiatus in the adductor magnus muscle to become the femoral vein.
The deep popliteal lymph nodes surround the popliteal vein (Gr 5.7C; Ne 473). They receive lymph from lymphatic vessels that accompany the deep veins of the leg and from the lymphatic vessels accompanying the small saphenous vein. Lymph from the deep popliteal lymph nodes follows the femoral vein to the deep inguinal lymph nodes (Gr 5.7A; Ne 473).
The sciatic nerve typically divides into the tibial and common fibular nerves at or near the superior border of the popliteal fossa (Figs. 9, 15; Gr 5.23B, 5.37; Ne 483, 490, 529). The tibial nerve (L4-S3) is the medial, larger terminal branch of the sciatic nerve. It descends through the middle of the popliteal fossa superficial to the popliteal artery and vein (i.e., the main structures in the popliteal fossa from deep to superficial are the popliteal artery, popliteal vein, and tibial nerve). The tibial nerve continues downward into the deep posterior compartment of the leg. It provides innervation to the muscles of the posterior compartment and continues into the sole of the foot to supply the intrinsic muscles there through medial and lateral plantar branches (Gr 5.62A, 5.63A; Ne 506, 529). The tibial nerve will be followed into the posterior compartment in a later dissection.
Laterally within the popliteal fossa the common fibular (common peroneal) nerve (L4-S2) descends laterally along the inferior border of the biceps femoris muscle (Figs. 9, 15; Gr 5.55, 5.58B; Table 5.9, Left [p. 411]; Ne 490, 508, 529, 530). It leaves the popliteal fossa by passing superficial to the lateral head of the gastrocnemius muscle and winds around the neck of the fibula to divide into its terminal branches deep to the fibularis longus muscle. The common fibular nerve and its branches will be followed distally during the leg dissection.
(See Figure 18)
18. Make a skin incision down the middle of the popliteal region and posterior leg as far inferiorly as the ankle (Fig. 18 A⇒B ). Make medial and lateral skin incisions from the inferior end of the first incision (C⇒D). Reflect the flaps of skin laterally to expose the lower part of the popliteal fossa and subcutaneous tissue of the leg. Be careful not to injure the small saphenous vein (Fig. 15C; Gr 5.5B-C; Ne 472) and medial and lateral sural cutaneous nerves in the superficial fascia of the calf (Gr 5.3B).
19. Find the small saphenous vein ascending from the middle of the calf to enter the popliteal fossa. You may see the medial sural cutaneous nerve accompanying the small saphenous vein in the groove between the medial and lateral heads of the gastrocnemius muscle. Carefully remove the fat from the popliteal fossa piecemeal to trace the small saphenous vein to where it enters the popliteal vein. Look for the medial sural cutaneous nerve at its origin from the tibial nerve. Clean the tibial nerve descending through the middle of the popliteal fossa superficial to the popliteal vessels. Spread apart the two heads of the gastrocnemius and find branches of the tibial nerve innervating them.
20. Clean the popliteal vein, beginning where it was identified by tracing the small saphenous vein to it. The popliteal vein and artery are bound together by tough fascia and must be separated by blunt dissection. It may be necessary to remove the vein to study the artery. Clean the popliteal artery and find its genicular branches (Fig. 17). Trace the popliteal artery from the adductor hiatus as far inferiorly as possible.
21. The superior medial genicular and superior lateral genicular arteries lie against the bone on the superior surface of the medial and lateral femoral condyles, respectively. If you find an artery entering a muscle, it is a muscular branch of the popliteal artery and not a deeper genicular branch. The inferior medial genicular artery descends obliquely deep to the medial head of the gastrocnemius and crosses the inferior surface of the medial tibial condyle. The inferior lateral genicular artery passes deep to the lateral head of the gastrocnemius muscle and toward the front of the leg in the groove between the lateral femoral condyle and the head of the fibula. The middle genicular artery passes deeply from the popliteal artery to pierce the capsule of the knee joint and may be difficult to find.
22. Study the floor of the popliteal fossa. Verify that the popliteal artery lies directly against the bone of the distal femur and against the articular capsule of the knee joint. The popliteus fascia and popliteus muscle, which form the lower third of the floor of the popliteal fossa, will be studied when the posterior compartment of the leg is dissected. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.
