Anterior Thigh and Knee Joint
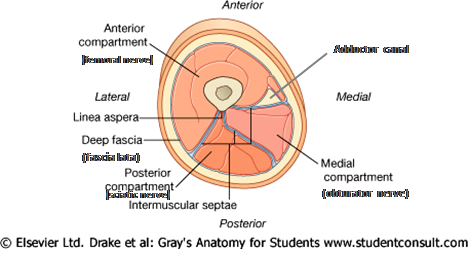
The anterior thigh (extensor) and medial thigh (adductor) compartments are compartments of the thigh bounded by intermuscular septa that pass from the deep surface of the deep fascia (fascia lata) to the linea aspera of the femur (Fig. 1). The posterior (flexor) compartment, which was studied during the last period, is the third compartment of the thigh. The actions “extensor” and “flexor” refer to the major action of the muscles in that compartment at the knee joint. Each compartment has one nerve that innervates the majority of its muscles. The anterior compartment of the thigh is innervated by the femoral nerve, the medial compartment by the obturator nerve, and the posterior compartment by the tibial division of the sciatic nerve.
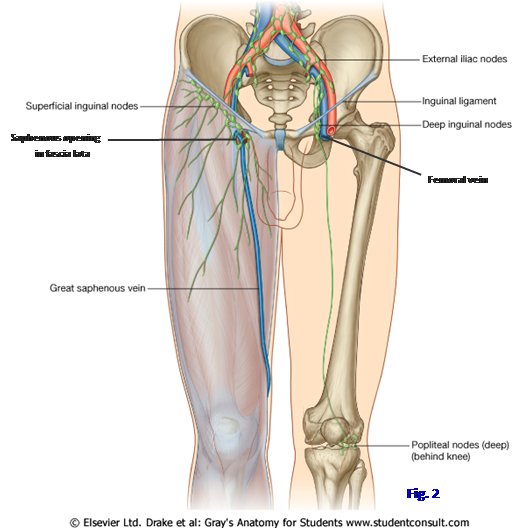
The superficial fascia, or subcutaneous connective tissue, over the anterior and medial thigh contains a variable amount of fat, a large superficial vein, lymphatic vessels and lymph nodes, and several cutaneous nerves. The great saphenous vein enters the thigh posterior to the axis of the knee joint and ascends anteriorly to pass through an opening in the fascia lata (saphenous opening or saphenous hiatus) below the medial half of the inguinal ligament (Gr 2.5, 5.5A, 5.6C, 5.8A, 5.13B-C; Ne 469, 471. It is a tributary of the femoral vein (Gr 5.10). Near the saphenous opening the great saphenous vein receives three smaller superficial veins that will be dissected later—the superficial circumflex iliac, superficial epigastric, and superficial external pudendal veins (Gr 2.4, 5.5, 5.11; Ne 250, 471).
The superficial epigastric vein may anastomose with the lateral thoracic vein to form a thoracoepigastric vein, which provides a collateral route for blood to return to the heart if either the superior vena cava or the inferior vena cava is blocked (Ne 250). The terminal portion of the great saphenous vein may become dilated (saphenous varix) and be confused with other groin swellings (e.g., a femoral hernia, psoas abscess).
The lower portion of the great saphenous vein will be seen later. It originates from the medial side of the dorsal venous arch of the foot, ascends anterior to the medial malleolus, and then inclines slightly posteriorly to pass behind the axis of the knee joint. The great saphenous vein freely communicates with the small saphenous vein of the leg seen during the last period.
The great saphenous vein is connected with deep veins of the lower extremity by numerous perforating veins that carry blood to the deep veins (Gr 5.5A, 5.6A), where the contractions of surrounding muscles can help return blood to the heart (musculovenous pump). The great saphenous vein has numerous valves that, when competent, prevent the reflux of blood down the extremity due to gravity. If the valves in perforating veins or in the great saphenous vein itself become incompetent, blood pools in the great saphenous vein and it becomes tortuous and dilated (varicose veins) (Gr 5.6B). The presence of valves also means that a segment of the great saphenous vein that is transplanted in coronary artery bypass surgery must be reversed to allow blood to flow past the site of coronary artery obstruction.
The lower extremity has superficial and deep lymphatic vessels (Fig. 2; Gr 5.7 Ne 473). Superficial lymphatic vessels accompany the great saphenous vein and its tributaries to end in the superficial inguinal lymph nodes, which are located just below the inguinal ligament (Gr 5.7, 5.11B, 5.12., Ne 473). The superficial inguinal nodes also receive lymph from the abdominal wall below the umbilicus, the perineum, and the gluteal region. Unexplained enlargement of the superficial inguinal lymph nodes (lymphadenopathy) is an indication to examine the entire field of drainage for possible cancer or infection. Two points to keep in mind are that scrotal cancer in males, but not testicular cancer, characteristically metastasizes to the superficial inguinal nodes (Gr 3.50A) and that uterine cancer in females occasionally metastasizes along the round ligament of the uterus to the labium majus to reach the superficial inguinal nodes (Gr 3.37A).
The superficial inguinal nodes send lymph through the saphenous opening to deep inguinal lymph nodes, which lie medial to the femoral vein and also receive the lymph from the deep lymphatic vessels that accompany the deep veins of the lower extremity. Some lymph from the superficial inguinal nodes also drains directly to the external iliac lymph nodes, bypassing the deep inguinal nodes.
The cutaneous nerves of the anterior and medial thigh are branches of the lumbar plexus of nerves. They include the lateral femoral cutaneous nerve and branches of the femoral, genitofemoral, and obturator nerves (Gr 2.73, 3.26, 5.3, 5.13A; Ne 471, 485, 486, 526, 527). The lateral femoral cutaneous nerve (L2-3) descends deep to the inguinal ligament lateral to the femoral nerve to supply the skin of the anterolateral and lateral thigh. Anterior cutaneous branches of the femoral nerve (L2-4) supply cutaneous innervation to most of the anterior thigh. The femoral branch of the genitofemoral nerve (L1-2) supplies the central part of the upper anterior thigh just below the inguinal ligament (Gr 2.12A; Ne 471). The cutaneous branch of the obturator nerve (L2-4) innervates the upper medial thigh below a small area innervated by the ilioinguinal nerve (L1). The ilioinguinal nerve was previously seen emerging from the superficial inguinal ring and forms the afferent limb of the cremasteric reflex arc in males.
The tough deep fascia of the thigh is the fascia lata. It is continuous inferiorly with the deep fascia of the leg (crural fascia). Superiorly, the membranous layer of superficial abdominal fascia (Scarpa’s fascia) fuses with the fascia lata just below the inguinal ligament, preventing the spread into the thigh of extravasated urine from a ruptured penile urethra or other fluids from the lower abdominal wall.
The fascia lata is thickened laterally between the tubercle of the iliac crest and the anterolateral tibial (Gerdy’s) tubercle as the iliotibial tract (iliotibial band) (Gr 5.8B, 5.22; Ne 482). The iliotibial tract helps to stabilize the knee joint laterally. It gives attachment to the gluteus maximus and tensor fasciae latae muscles. The iliotibial tract may be a source of pain at the hip or at the knee, where it causes inflammation due to friction (iliotibial band syndrome, e.g., http://www.aafp.org/afp/20050415/1545.html ).
The saphenous opening is a gap in the fascia lata inferior to the medial portion of the inguinal ligament (Gr 5.8A, 5.11B, 5.13A; Ne 250, 471). It has a sharp crescentic falciform margin superiorly, laterally, and inferiorly. The opening is filled by sieve-like cribriform fascia, which is traversed by lymph vessels and the great saphenous vein.
1. The cadaver needs to be placed in a supine position for this dissection.
2. Palpate the anterior superior iliac spine and the pubic tubercle, which are the attachment sites for the inguinal ligament. Incise the skin along the flexion crease between the thigh and anterior abdominal wall. The crease is located just inferior to the inguinal ligament. From the midpoint of the inguinal ligament, make a vertical incision through the skin down the front of the thigh to 5 cm below the patella. From the lower end of this cut, make incisions laterally and medially until you encounter the incisions made earlier in the posterior leg. Remove the skin of the thigh.
3. Locate the great saphenous vein ascending through superficial fascia along the medial side of the thigh and carefully clean it (Fig. 2). Be aware of three small tributaries that join it near its termination: the superficial circumflex iliac, superficial epigastric, and superficial external pudendal veins (Gr 5.5A, 5.11A; N250, 471). Find the saphenous opening of the fascia lata, which the great saphenous vein traverses to reach the femoral vein. Note the sharp falciform margin of the saphenous opening laterally and the sieve-like cribriform fascia that fills it. Find several large superficial inguinal lymph nodes just inferior to the inguinal ligament and in the region of the saphenous opening (Fig. 2).
4. Identify, and study the distribution of, the cutaneous nerves of the anterior and medial thigh compartments but don’t spend a lot of time cleaning them (Gr 5.3, 5.11B, 5.13A; N471). The lateral femoral cutaneous nerve descends deep to the inguinal ligament just medial to the anterior superior iliac spine. It supplies the skin of the anterolateral thigh. The femoral branch of the genitofemoral nerve passes under the midpoint of the inguinal ligament. The ilioinguinal nerve leaves the superficial inguinal ring to supply skin of the upper medial thigh.
5. The anterior cutaneous branches of the femoral nerve supply most of the skin over the anterior thigh and the lower third of the medial thigh. The obturator nerve sends cutaneous innervation to the middle part of the medial thigh, between areas innervated by the ilioinguinal and femoral nerve.
6. Leave the iliotibial tract intact, but remove the rest of the fascia lata covering the anterior thigh. To do this, define the iliotibial tract and make a vertical incision along its anterior margin from the lower end of the anterior margin of the tensor fasciae latae muscle to the lateral condyle of the tibia (Gr 5.8A-B, 5.17, 5.22B; N482). Remove the fascia lata medial to the tensor and the iliotibial tract to expose the anterior thigh muscles. XXX
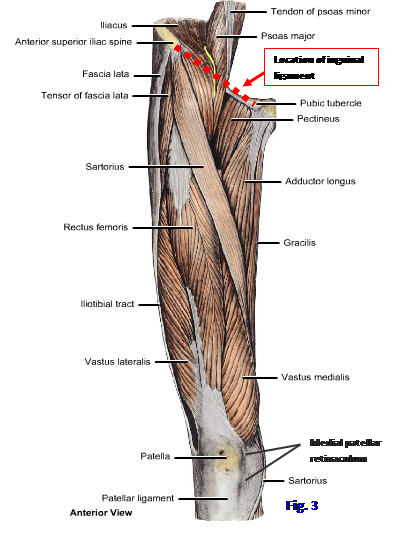
The anterior thigh muscles are the iliopsoas, pectineus, sartorius, tensor fasciae latae, and quadriceps femoris (Fig. 3; Gr 5.16, 5.17, 5.18, 5.22; Table 5.2 [p. 358]; Ne 256, 480, 486, 488). The iliopsoas muscle is formed by two muscles, the psoas major and the iliacus, that arise separately within the abdomen and join to pass deep to the inguinal ligament and insert on the lesser trochanter of the femur (Gr Table 2.5 [p. 164]). The psoas major attaches proximally to vertebrae Tv12-Lv5 and the intervening intervertebral discs. The iliacus muscle takes origin from the iliac crest, iliac fossa, and anterior sacroiliac ligament. The iliopsoas muscle is the most powerful of the hip flexor muscles, but isn’t always recruited during routine movements. Its powerful contractions may avulse the lesser trochanter in skeletally immature individuals and those with metastatic lesions at the site.The iliopsoas receives innervation from the femoral nerve (L2-4) and the psoas major receives additional innervation from the anterior rami of spinal nerves L1-3.
A pyogenic retroperitoneal infection of the posterior abdominal cavity (e.g., tuberculosis of the lumbar vertebral column) may result in a psoas abscess that spreads between the muscle and its fascia (psoas fascia). The abscess passes deep to the inguinal ligament and into the proximal thigh (Fig. 3), where it may be mistaken for a femoral hernia, saphenous varix, or enlarged superficial inguinal lymph nodes. Due to the iliopsoas muscle’s close relationships to the kidneys and ureters, pancreas, cecum and appendix in the abdomen, inflammation of any of these structures (e.g., acute appendicits) may cause pain when the patient extends the affected thigh against resistance (positive iliopsoas maneuver or psoas sign ( http://radiographics.rsnajnls.org/cgi/reprint/15/6/1285 )).
The pectineus is included here with the muscles of the anterior compartment of the thigh because it is usually innervated by the femoral nerve. However, some anatomists classify the pectineus as a medial thigh muscle because of its location (Fig. 3; Gr 5.14, 5.15, 5.17; Ne 480, 488) and its occasional innervation by the obturator nerve (L2-4) (Gr Table 5.1 [pp. 348-349]; Ne 489) and/or accessory obturator nerve (L3-4). The pectineus passes from the superior ramus of the pubis to the pectineal line of the femur. It adducts and flexes the thigh at the hip joint.
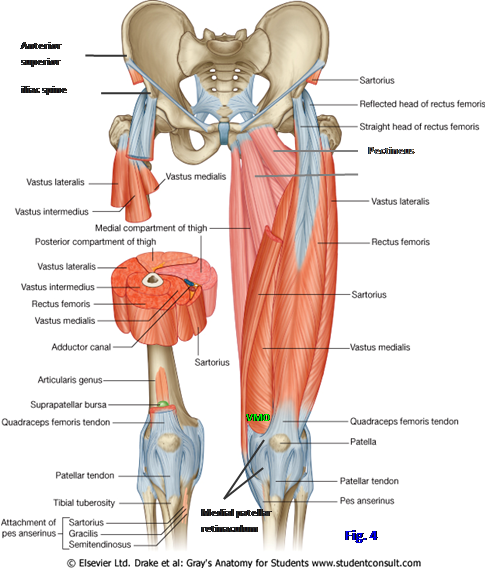
The sartorius is the longest muscle in the body (Figs. 3, 4; Gr 5.14, 5.16, 5.17; Table 5.2 [p. 358]; Ne 469, 480, 488). It passes from the anterior superior iliac spine to insert into the medial side of the upper tibia as part of the pes anserinus (Gr 5.41; Ne 480, 494) with the gracilis and semitendinosus muscles. The sartorius, therefore, crosses both the hip and knee joints and acts on both. It flexes, abducts, and laterally rotates the thigh at the hip joint and flexes the leg at the knee joint. It is called the “tailor’s muscle” because its actions place the lower extremity in the traditional cross-legged sitting posture of a tailor. The sartorius muscle may avulse the ASIS in skeletally immature individuals.
The tensor fasciae latae muscle takes origin from the ASIS and the anterior portion of the iliac crest just behind it (Fig. 3; Gr 5.8B, 5.17, 5.22; Ne 480, 482). It descends somewhat posteriorly to insert into the iliotibial tract opposite the gluteus maximus muscle. The tensor flexes and medially rotates the thigh. Following paralysis of the iliopsoas muscle, the tensor fasciae latae may hypertrophy in a largely futile effort to help compensate for weakened hip flexion. It may act through the iliotibial tract with the gluteus maximus to help keep the extended knee in extension. The tensor fasciae latae is unusual among the anterior thigh muscles due to its innervation by the superior gluteal nerve.
The quadriceps femoris muscle forms most of the muscle mass of the anterior thigh (Figs. 3, 4; Gr 5.16-5.18, 5.22; Table 5.2 [p. 358]; Ne 480, 488, 489, 526). As its name indicates, the quadriceps has four heads—the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis—that share a common insertion into the tibial tuberosity with the patella as a sesamoid bone in the tendon. The part of the quadriceps tendon between the patella and tibial tuberosity is the patellar ligament. (Note: some anatomists describe the quadriceps as inserting into the patella, which is then joined to the tibial tuberosity by the patellar ligament). The rectus femoris is the only part of the quadriceps femoris that crosses the hip joint. It arises from the anterior inferior iliac spine (straight head) and from the ilium just above the acetabulum (reflected head) and runs straight down the thigh. The rectus femoris can flex the thigh and extend the leg, although it doesn’t do both effectively at the same time. It may avulse the AIIS in immature athletes (see http://www.learningradiology.com/archives06/COW%20205-Ischial%20Avulsion%20Fx/avulseischiumcorrect.htm) e.g. while kicking a football.
The vasti muscles are the vastus lateralis, vastus medialis, and vastus intermedius, which work together with each other and with the rectus femoris to extend the leg (Gr 5.18, Table 5.2 [p. 358]; Ne 478-480, 482, 488). The vastus lateralis takes origin from the greater trochanter of the femur and the lateral lip of the linea aspera. The vastus medialis takes origin from the intertrochanteric line and medial lip of the linea aspera. Its lower fibers approach the patella almost horizontally (vastus medialis obliquus, VMO) and play a role in preventing lateral subluxation of the patella. In addition to their contributions to the quadriceps femoris tendon per se, the vastus lateralis and medialis have tendinous expansions at the sides of the patella and the patellar ligament (lateral and medial patellar retinacula, respectively) that help to form the capsule of the knee joint anteriorly (Figs. 3, 4; Ne 480, 495).
The vastus intermedius lies deep to the rectus femoris between the vastus medialis and vastus lateralis muscles. It takes origin from the anterior and lateral surfaces of the femoral shaft. The vastus intermedius has a few deep fascicles (articularis genus) that attach to synovium of the suprapatellar bursa of the knee and elevate it during leg extension to prevent pinching between the patella and femur (Fig. 4; Gr 5.47A-B, 5.52 A-B; Ne 495, 499).
Most of the muscles of the anterior compartment of the thigh are innervated by the femoral nerve (L2-4) from the lumbar plexus Ne 526). The psoas major receives additional innervation from the anterior rami of L1-3. The pectineus may be innervated by the obturator nerve and/or accessory obturator nerve. The tensor fasciae latae is developmentally related to the gluteus medius and minimus muscles and is innervated by the superior gluteal nerve.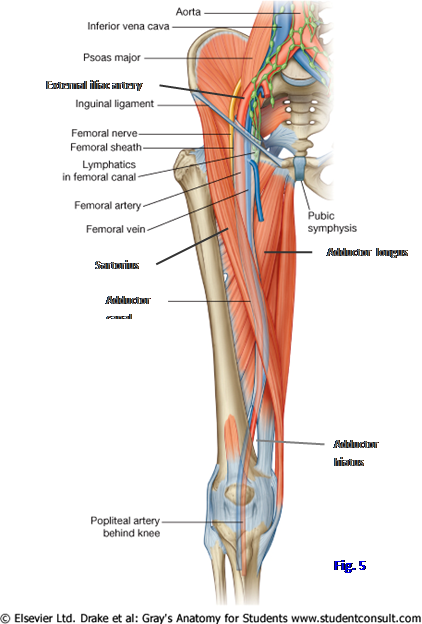
The medial thigh muscles, the adductor group, are the adductor longus, adductor brevis, adductor magnus, gracilis, and obturator externus (Figs. 3, 4; Gr 5.16-5.19; Table 5.3 [p. 360]; Ne 480, 481). As a group they adduct the thigh, although some have additional actions. All receive innervation from the obturator nerve (L2-4). The adductor longus is the most anteriorly placed of the medial thigh muscles and lies just inferior to the pectineus. The adductor longus arises from the anterior aspect of the body of the pubis and fans out to attach distally to the middle third of the linea aspera.
The adductor brevis is hidden by the pectineus and adductor longus muscles (Gr 5.17, 5.18, 5.21; Ne 489, 527). It arises from the body and inferior ramus of the pubis and inserts into the proximal part of the linea aspera. The obturator nerve splits into anterior and posterior divisions/branches around the adductor brevis (Gr 5.21; Ne 489, 527), which is helpful in identifying the muscle during dissection. The obturator artery descends only a short distance into the medial compartment, which is supplied mainly by the profunda femoris artery.
The adductor magnus muscle is the largest of the adductor muscles (Gr 5.19A, 5.21, 5.23D, Table 5.3 [p. 360]; Ne 481, 483, 489). It consists of adductor and hamstring parts, which have different attachments, actions, and nerve supplies. The adductor part takes origin from the ischiopubic ramus and fans out to insert on the gluteal tuberosity, entire length of the linea aspera, and on the medial supracondylar line. It is innervated by the obturator nerve and functions mainly in adduction of the thigh. The hamstring part of the adductor magnus takes origin from the ischial tuberosity and inserts into the adductor tubercle on the superior surface of the medial femoral epicondyle. It is innervated by the tibial division of the sciatic nerve and may help the other hamstring muscles to extend the thigh; however, it doesn’t cross the knee joint and cannot act on it.
The adductor hiatus is a gap in the adductor magnus between the insertions of its adductor and hamstring parts into the femur (Fig. 5; Gr 5.15B, 5.23D, 5.28A; Ne 481, 489, 527). Therefore, the adductor hiatus is located just superolateral to the adductor tubercle. It transmits the femoral artery and vein from the adductor canal into the popliteal fossa, where the names change to the popliteal artery and vein.
The obturator externus muscle lies deep to the pectineus muscle (Gr 5.20B,5.27, 5.29A; Ne 481, 489). It takes origin from the external surface of the obturator membrane and bony margins of the obturator foramen. It passes posterior to the capsule of the hip joint and neck of the femur to insert into the trochanteric fossa. It is a lateral rotator of the thigh. Some authors include the obturator externus with the gluteal region, but its innervation from the obturator nerve and the location of its origin argue for inclusion as a medial thigh muscle.
The femoral triangle is a triangular space just deep to the fascia lata of the upper thigh (Fig. 5; Gr 5.14, 5.15; Ne 480, 488). It is bounded superiorly by the inguinal ligament, laterally by the sartorius, and medially by the medial border of the adductor longus. The floor of the femoral triangle is formed by the iliopsoas, pectineus, and adductor longus muscles.
The contents of the femoral triangle, from lateral to medial, are the femoral nerve, femoral artery, and femoral vein (Fig. 5; Gr 5.13B & E, 5.14, 5.15, Table 5.1 [pp. 348-349]; Ne 488, 526). The femoral nerve is formed by the anterior rami of spinal nerves L2-4 and is the largest branch of the lumbar plexus. It is formed within the substance of the psoas major muscle on the posterior abdominal wall and descends posterolateral to the muscle, in the groove between it and the iliacus. The femoral nerve leaves the abdominal cavity deep to the inguinal ligament to enter the femoral triangle. It innervates most of the muscles of the anterior thigh and sends articular branches to both the hip and knee joints. The femoral nerve’s innervation of both joints provides a path for referred pain from the hip to the knee; therefore, unexplained knee pain is an indication to examine the hip for problems. The femoral nerve leaves the femoral triangle to enter the adductor canal (discussed below). The saphenous nerve is a branch of the femoral nerve that arises within the adductor canal and passes medial to the knee to accompany the great saphenous vein in superficial fascia of the leg (Gr 5.3, 5.21, 5.63A; Ne 471, 488, 489).
The femoral artery is the continuation of the external iliac artery at the inguinal ligament (Fig. 5; Gr 2.82C, 5.9A, 5.13A, 5.14; Ne 257, 488, 500). It occupies an intermediate position between the femoral nerve and femoral vein. The femoral artery changes position from lateral to the femoral vein to anterior to it as it descends through the femoral triangle and the adductor canal. That means that when the artery traverses the adductor hiatus and becomes the popliteal artery, it lies directly against the distal femur, where it is vulnerable to injury following a fracture.
The profunda femoris artery (deep artery of the thigh) is the largest branch of the femoral artery and the main blood supply of the thigh (Gr 5.9A, 5.14, 5.21, 5.34A; Ne 488, 489, 500). It arises in the femoral triangle and descends posterior to the adductor longus muscle, which separates it from the femoral artery. Two large arteries that usually branch from the profunda femoris, but may branch directly from the femoral artery, are the medial femoral circumflex and lateral femoral circumflex arteries. The medial femoral circumflex artery passes posteriorly between the iliopsoas and pectineus muscles (Gr 5.15; Ne 489).
The lateral femoral circumflex artery passes laterally in front of the iliopsoas muscle and behind the sartorius and rectus femoris. It divides into ascending, transverse, and descending branches (Ne 489, 492, 500). The ascending branch of the lateral femoral circumflex passes deep to the tensor fasciae latae to anastomose with the superior gluteal artery. The transverse branch enters the vastus lateralis muscle. It participates in the cruciate anastomosis. The descending branch descends behind the rectus femoris muscle to supply the vastus intermedius and vastus lateralis. It also participates in the genicular anastomosis around the knee joint (Gr 5.9, 5.48A; Ne 500).
Both femoral circumflex arteries supply muscles, but the medial femoral circumflex is also the major blood supply to the head of the adult femur via its retinacular branches (Gr 5.34, 5.35; Ne 492, 500). Interruption of this blood supply by a fracture of the femoral neck (common in postmenopausal women with osteoporosis) frequently results in avascular necrosis of the femoral head and necessitates hip replacement surgery. Both femoral circumflex arteries also participate with the inferior gluteal and first perforating arteries in the cruciate anastomosis (Gr 5.28A).
The profunda femoris artery gives off four perforating arteries to supply the posterior compartment of the thigh (Gr 5.9, 5.25, 5.28; Ne 489, 490, 500). They pierce the adductor magnus muscle near its femoral attachment to reach the posterior compartment and then pierce the lateral intermuscular septum to help supply the vastus lateralis of the anterior compartment. The first perforating artery sends an ascending branch to participate in the cruciate anastomosis. The fourth perforating artery is usually the continuation of the profunda femoris artery itself.
A femoral pulse is easily taken in a supine patient just inferior to the inguinal ligament midway between the ASIS and pubic tubercle. The femoral artery may be compressed posteriorly against the superior pubic ramus and femoral head through the overlying iliopsoas muscle (Figs. 5, 6; Gr 5.14, 5.15, G5.33, 5.34A; Ne 488, 489, 500) to control bleeding from the lower extremity. Femoral or popliteal laceration may cause rapid exsanguination. If both the femoral artery and vein are lacerated, an arteriovenous shunt may form. The femoral artery is readily accessible for cannulation for cardiac angiography ( http://www.newportbodyscan.com/Downloads/CTAgioEBvMDCT.htm ).
The femoral vein is the superior continuation of the popliteal vein at the adductor hiatus and becomes the external iliac vein at the inguinal ligament (Gr 5.10, 5.13B-C, 5.14, 5.15A; Ne 488, 489). It moves from a position posterior to the femoral artery to a position medial to the artery as it ascends from the adductor hiatus toward the inguinal ligament. The femoral vein, therefore, is medial to the femoral artery and nerve in the femoral triangle. It receives the great saphenous vein as a tributary via the saphenous opening. The femoral vein receives the profunda femoris vein (deep vein of the thigh) as a deep tributary approximately 5 cm below where it receives the great saphenous vein.
The femoral vein may be cannulated to access the right side of the heart or to administer intravenous fluids. The hip joint may be seeded with infection that may destroy the joint (septic arthritis) during femoral venipuncture due to poor technique. Some clinicians, unfortunately, use the term “superficial femoral vein” to refer to the femoral vein. That makes it easy to forget that the femoral vein is a deep vein and may be a site of deep venous thrombosis, the most common source of pulmonary thromboemboli. Massive pulmonary embolism is the second leading cause of sudden death.
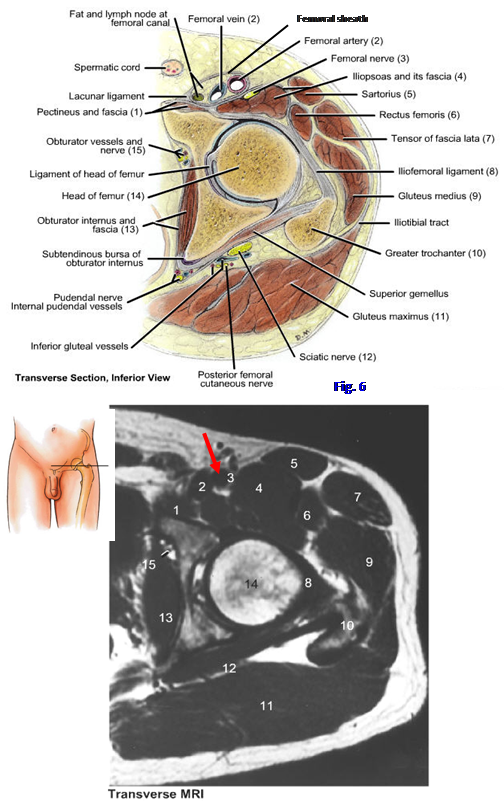
The femoral sheath is a 3-4 cm tubular extension of transversalis and iliopsoas fascia below the inguinal ligament (Fig. 6; 5.13A; Ne 244, 255, 473, 488). The femoral sheath is subdivided into three compartments by vertical connective tissue septae. The lateral compartment of the femoral sheath contains the proximal part of the femoral artery. The femoral nerve is lateral to the femoral sheath and is not contained within it. The intermediate compartment contains the terminal part of the femoral vein. The medial compartment of the femoral sheath is the femoral canal (Gr 5.13F-G; Ne 255) and contains a deep inguinal lymph node (Cloquet’s node) and lymph vessels, along with fat and loose connective tissue. The proximal opening into the femoral canal is the femoral ring, which is filled by a condensation of extraperitoneal connective tissue (femoral septum). The femoral ring is larger in females due to a wider pelvis. The femoral ring is bounded anteriorly by the inguinal ligament, medially by the lacunar ligament, posteriorly by the pectineus and its fascia, and laterally by the femoral vein.
In a femoral hernia, which is more common in females, a loop of intestine or other viscera protrudes through the femoral ring from the abdominal cavity. The hernia is covered by peritoneum and extraperitoneal connective tissue and may escape through the saphenous opening into superficial fascia of the thigh. Femoral hernias are distinguished from inguinal hernias by the protrusion being inferior and lateral to the pubic tubercle rather than superior to it. Femoral hernias are in danger of strangulation by the lacunar ligament at the femoral ring and by the sharp falciform margin at the saphenous opening.
7. Clean the sartorius muscle as it descends medially across the thigh from the anterior superior iliac spine toward the pes anserinus. Identify the other boundaries of the femoral triangle, the inguinal ligament and the adductor longus muscle. Clean the three main structures in the femoral triangle. The most lateral structure is the femoral nerve. It is a large nerve emerging into the thigh below the inguinal ligament and quickly dividing into multiple cutaneous and motor branches.
8. Clean the femoral artery medial to the femoral nerve. Look for the femoral sheath covering the proximal portion of the vessel. Just medial to the femoral artery, also partly invested by the femoral sheath, clean the femoral vein. The great saphenous vein was previously seen entering it via the saphenous opening. Medial to the femoral vein within the femoral sheath identify the location of the femoral canal. It typically contains a large deep inguinal lymph node. Insert a probe superiorly into the femoral canal. Note that when the probe traverses the femoral ring, it is bounded by the inguinal ligament anteriorly, lacunar ligament medially, pectineus and pectineal fascia posteriorly, and the femoral vein laterally. Palpate the sharp edge of the lacunar ligament, which may strangulate a femoral hernia.
9. Clean the fascia from the iliopsoas muscle, pectineus, and adductor longus muscles, which form the floor of the femoral triangle. Return to the femoral artery and look for large branches arising from it. The profunda femoris artery branches from the posterolateral surface of the femoral artery and disappears posterior to the adductor longus muscle. Find the medial femoral circumflex and lateral femoral circumflex arteries branching either from the profunda femoris or the femoral artery itself. The medial femoral circumflex artery and accompanying vein pass posteriorly in the interval between the iliopsoas and pectineus muscles. Follow the lateral femoral circumflex artery laterally and identify, but don’t attempt to follow, the ascending, transverse, and descending branches.
10. Cut the sartorius muscle near its middle and reflect the two halves. In one lower extremity, cut the rectus femoris muscle transversely and reflect the two parts toward their attachments. Identify the vastus lateralis, vastus intermedius, and vastus medialis muscles. Note how the tendons of the rectus femoris and vasti muscles join to attach to the tibial tubercle with the patella as a sesamoid bone within the quadriceps femoris tendon.
MEDIAL COMPARTMENT OF THE THIGH
11. Turn your attention to the adductor compartment of the thigh. Again define the borders of the pectineus and adductor longus muscles. Divide the pectineus and adductor longus muscles of one lower extremity about mid-length and reflect the two halves toward their respective attachments. This will expose the adductor brevis muscle. Identify and clean the anterior and posterior divisions/branches of the obturator nerve superficial and deep, respectively, to the adductor brevis. Look for small branches of the obturator artery, which normally are present only in the upper part of the compartment. Attempt to find one or more perforating arteries passing from the profunda femoris through the adductor magnus to reach the posterior compartment of the thigh. Two of the perforating arteries frequently pierce the adductor brevis to reach the magnus.
12. Posterior to the reflected pectineus muscle, clean the origin of the obturator externus muscle. The posterior division of the obturator nerve pierces the obturator externus muscle, and the anterior division passes anterior to it. Attempt to verify these relationships. XXX
The knee joint is a hinge type of synovial joint formed by three articulations (Figs. 7, 8; Gr 5.1, 5.20A & C; Ne 495-499). The two larger articulations are between the medial femoral condyle and medial tibial condyle and between the lateral femoral condyle and lateral tibial condyle. The third articulation is the patellofemoral articulation, which is formed between a shallow groove on the anterior surface of the lower femur (patellar surface) and the wedge-shaped posterior surface of the patella (Figs. 7, 8; Gr 5.43, 5.44, 5.49; Ne 495, 499). The patellofemoral articulation is best seen in a silhouette or skyline (sunset) view x-ray (Figs. 7, 8). The fibula is not involved in formation of the knee joint.
The knee joint is relatively unstable mechanically because it has incongruent femoral and tibial articular surfaces (Fig. 8; Gr 5.20, 5.41B, 5.42B; Ne 497-499). Essentially the femorotibial articulations consist of rounded femoral condyles sitting atop almost flat articular surfaces on the tibial condyles (tibial plateaus). The congruity between the articular surfaces is increased slightly by crescentic plates of fibrocartilage between the femoral and tibial surfaces, the medial and lateral menisci. They will be discussed in
more detail below. The main stabilizing structures of the knee joint are the surrounding muscles, with their tendons, and the ligaments connecting the femur and tibia.
The patella is a seasmoid bone withing the tendon of the quadriceps femoris muscle. It acts as a fulcrum that holds the quadriceps femoris tendon away from the joint axis of rotation to increase its mechanical advantage (Fig. 9B). The patella also reduces friction on the quadriceps tendon during knee flexion and extension and pressure on the tendon when kneeling.
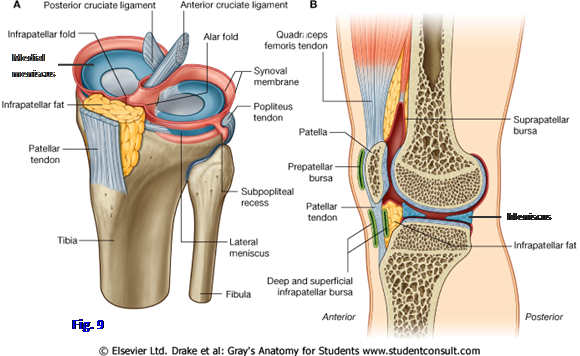
The articular capsule of the knee joint is a typical synovial joint capsule except that it is replaced anteriorly by the quadriceps femoris tendon, patella, and patellar ligament (patellar tendon). The fibrous capsule is lined internally by synovial membrane except over articular surfaces (Fig. 9; Ne 495, 496). In transverse section, the synovial cavity is horseshoe-shaped with the posterior indentation occupied by the cruciate ligaments in the intercondylar fossa of the femur (i.e., the cruciate ligaments are intracapsular but extrasynovial). A median infrapatellar synovial fold covers an infrapatellar fat pad anteriorly between the lower border of the patella and the intercondylar fossa of the femur (Gr 5.43; Ne 495, 499).
A large superior extension of the synovial cavity anteriorly, the suprapatellar bursa, is clinically important. Because the bursa is continuous with the joint cavity, infection in either space easily spreads to the other. The suprapatellar bursa also can accommodate a large amount of joint effusion during synovitis of the knee joint and may mask the swelling characteristic of inflammation unless the bursa is “milked” downward toward the joint cavity.
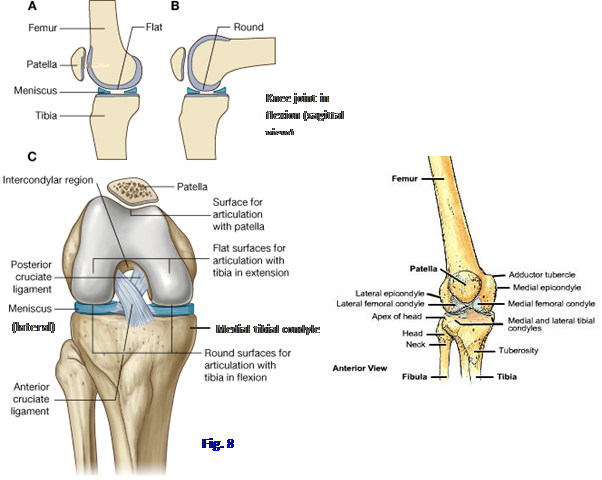
The articular capsule of the knee joint is strengthened by several ligaments. Many are essentially thickenings of the capsule. The collateral ligaments on the sides of the knee are the tibial (medial) collateral ligament and the fibular (lateral) collateral ligament (Gr 5.41, 5.42, 5.44A, 5.45; Ne 494, 497, 499). Both become tense in extension of the knee, contributing to stability. The tibial collateral ligament passes from the medial epicondyle of the femur to the medial condyle and superior part of the shaft of the tibia. The deep fibers of the tibial collateral ligament firmly attach to the medial meniscus. Therefore, injury to the tibial collateral ligament typically is accompanied by injury to the medial meniscus (see below).
The fibular collateral ligament is a cord-like structure that passes from the lateral epicondyle of the femur to the head of the fibula (Gr 5.42A, 5.44A, 5.45A, 5.47B-C; Ne 494, 497, 499, 509). It is separate from the capsule of the knee joint and does not attach to the lateral meniscus. The tendon of the biceps femoris is split into two parts at the fibular head by the fibular collateral ligament.
The oblique popliteal ligament is a superolateral expansion from the tendon of the semimembranosus muscle (Gr 5.23C-D; Ne 499). It reinforces the capsule of the knee joint posteriorly over the intercondylar fossa of the femur. The arcuate popliteal ligament is a variable thickening of the capsule over the popliteus muscle as it emerges through the capsule. This ligament ascends from the head of the fibula to spread out over the posterior capsule and strengthen it.
The major intracapsular ligaments of the knee joint are the cruciate ligaments, so called because they cross each other during their course (Figs. 8C, 9A; Gr 5.44A & C, 5.45, 5.46, 5.50; Ne 496, 497). Although they are enclosed within the area bounded by the fibrous capsule of the joint, the cruciate ligaments are located outside the synovial cavity (i.e., they are intracapsular but extrasynovial structures) (Fig. 9A). The anterior cruciate ligament ascends from the anterior intercondylar area of the tibia posteriorly and laterally to attach to the medial side of the lateral femoral condyle. It limits anterior displacement of the flexed tibia on the femur and helps restrict rotation at the joint.
The posterior cruciate ligament ascends from the posterior intercondylar area of the tibia anteriorly and medially to attach to the lateral side of the medial femoral condyle (Figs. 8C, 9A). A slender posterior meniscofemoral ligament passes from the lateral meniscus behind the posterior cruciate ligament to the medial femoral condyle (Gr 5.45A; Ne 497). The posterior cruciate ligament limits posterior displacement of the flexed tibia on the femur. At least one of the cruciate ligaments is tense in every position of the joint.
The menisci are intracapsular plates of fibrocartilage (Figs. 8A-C, 9; Gr 5.44A & C, 5.45A, 5.46B, 5.50; Ne 495-497, 499). They are crescent-shaped from a superior view and wedge-shaped in section, thicker externally where they attach to the joint capsule and tapering to a thin free edge in the interior of the joint. They are attached to the margins of the tibial condyles by portions of the joint capsule called coronary ligaments (Gr 5.44A). The menisci deepen the articular surfaces of the tibia to receive the rounded femoral condyles, increasing joint congruity. They also disperse pressure on the articular cartilages, and function in shock absorption.
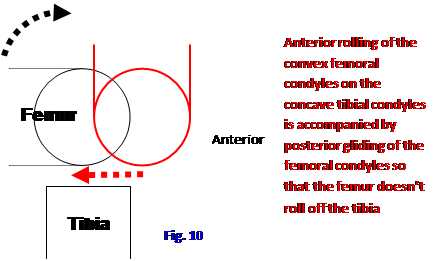
Anterior rolling of the convex femoral condyles on the concave tibial condyles is accompanied by posterior gliding of the femoral condyles so that the femur doesn’t roll off the tibia (Fig. 10)
The medial meniscus has anterior and posterior horns attached to the anterior and posterior intercondylar areas, respectively, of the tibia (Gr 5.44A & C, 5.45, 5.46; Ne 496). Its periphery is attached to the margin of the medial tibial condyle by the coronary ligament. Importantly, the medial meniscus is firmly attached to deep fibers of the tibial collateral ligament. Its attachments mean that the medial meniscus is relatively immobile and, therefore, susceptible to injury. The anterior cruciate ligament is often injured together with the tibial collateral ligament and medial meniscus as part of the unhappy triad of athletic knee injuries. (Note: some authors have attempted to change the definition of the unhappy triad to substitue the lateral meniscus for the medial meniscus, but the original definition is still the predominant one and will be used for testing purposes.)
The lateral meniscus is smaller and rounder than the medial meniscus (Gr 5.46; Ne 496). The anterior and posterior horns attach to the intercondylar area of the tibia much closer together than the attachments of the medial meniscus. The tendon of the popliteus muscle has an attachment to the lateral meniscus and pulls the meniscus out of the way when the popliteus muscle laterally rotates the femur on the tibia to unlock the knee from the position of full extension. The anterior horns of the medial and lateral menisci may be connected by a slender fibrous transverse ligament of the knee (Gr 5.44C; Ne 497).
The main movements at the knee joint are flexion and extension, but as the knee moves the final few degrees into full extension, the femur also rotates 5° medially on the weight-bearing tibia to lock the knee. Achieving flexion and extension requires a combination of rolling and gliding movements (Fig. 10). As the knee moves into extension, the convex femoral condyles roll forward on the tibial condyles (Arrow Right), which are made slightly concave by the menisci. If concurrent posterior sliding of the femoral condyles on the tibia didn’t occur (Arrow Left), the femoral condyles would roll off the front of the tibia and the joint would dislocate. (Note: it’s beyond the scope of this description, but joint movement differs if a concave surface moves on a convex surface.) The cruciate ligaments help to direct these movements.
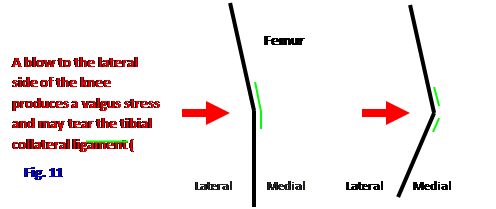
The most common injuries to the knee joint are ligament sprains. A blow to the lateral side of the knee (e.g., a tackle in football) produces a valgus stress, often tearing the tibial collateral ligament (Fig. 11). Since the medial meniscus is firmly attached to the ligament, the meniscus often is torn together with it. The anterior cruciate ligament may be torn with the medial meniscus and the tibial collateral as part of the unhappy triad of athletic knee injuries. (See http://www.emedicine.com/emerg/topic288.htm for a description of common knee injuries.)
A blow to the medial side of the knee produces a less common varus stress that stretches and may tear the fibular collateral ligament. Since the ligament has no attachment to the lateral meniscus, the meniscus typically is not torn with it. The common fibular nerve may be injured during a severe varus stress and should be examined along with the fibular collateral ligament.
The ACL may be sprained by different mechanisms, but they often involve a rapid change of direction (rotation of the femur on the tibia) with the foot firmly planted and/or a blow to the knee. A common mechanism is knee valgus with external tibial rotation. Acute extravasation of blood into the joint cavity (hemarthrosis) is common. If the anterior cruciate ligament is torn, the flexed tibia can be pulled forward on the fixed femur (anterior drawer sign). If the stronger PCL is torn, the flexed tibia can be pulled backward on the fixed femur by the examiner (posterior drawer sign). The posterior cruciate may be injured when the upper tibia of an unrestrained front seat passenger strikes the dashboard of an auto during a collision.
Meniscal tears usually involve the medial meniscus rather than the more mobile lateral meniscus. Injury commonly involves flexion-rotation or extension-rotation during weight-bearing. Symptoms include joint line pain, popping, catching, and locking. Effusion or hemarthrosis may be present. Only the peripheral third of the adult meniscus has a vascular supply and, therefore, a capacity for healing. Injury to the inner two-thirds of a meniscus may require surgical repair or removal of part or all of the meniscus. Efforts are made to spare (or transplant) a meniscus if possible because the concentrated weight on the femoral and tibial articular surfaces following meniscectomy predisposes to the early development of osteoarthritis.
Injuries of the extensor mechanism of the knee include rupture of the quadriceps tendon, rupture of the patellar ligament, patellar fracture, and patellar dislocation. Rupture of the quadriceps tendon typically occurs over the age of 40 years following a preexisting condition that weakens the tendon, such as tendinitis. Quadriceps rupture results in inability to extend the knee, with a gap developing in the suprapatellar region during the attempt. Rupture of the patellar ligament (patellar tendon) usually occurs in individuals younger that 40. Active knee extension is lost and the patella rides high (patella alta) because it has lost its anchor to the tibial tuberosity.
Transverse fractures of the patella often result from forceful contraction of the quadriceps femoris muscle against resistance (e.g., see http://emedicine.medscape.com/article/394270-overview ). The fracture is typically near the middle of the patella, and the proximal fragment is displaced upward by the pull of the quadriceps. Active extension is lost and the defect in the bone may be palpable. Comminuted fractures of the patella result from direct trauma, and the fragments often remain nondisplaced. Occasionally the fractured patella must be excised, which means that a much stronger quadriceps femoris is necessary to extend the knee with the same force due to the loss of mechanical advantage. Fractures of the patella must be differentiated from normal variations in patellar structure resulting from lack of fusion of secondary ossification centers (e.g., bipartite patella).
The patella may partially dislocate (sublux) or dislocate from its articulation with the groove on the patellar surface of the femur as a result of trauma or congenital factors. Patellar dislocation is almost always lateral and occurs more frequently in females due to the larger Q angle (formed by a line drawn between the ASIS and middle of the patella and a line drawn from the center of the patella through the tibial tubercle). Other factors that predispose to lateral subluxation include a shorter anterior projection of the lateral femoral condyle and a weak vastus medialis obliquus. Self-reduction of the dislocated patella usually occurs, but the patient shows a positive patellar apprehension sign if the examiner pushes the patella laterally with the knee of the supported extremity flexed to 30° or so.
There are a number of bursae associated with the knee region (Fig. 9B). The knee bursa most commonly inflamed overlies the patella and is subject to repeated friction, producing inflammation (prepatellar bursitis or “housemaid’s knee”). There are superficial and deep infrapatellar bursae related to the patellar ligament. Superficial infrapatellar bursitis may be confused with Osgood-Schlatter disease. Anserine bursitis involving the pes anserinus bursa may be confused with a tibial collateral ligament injury.
On the posterior aspect of the knee, the semimembranosus bursa between the medial head of the gastrocnemius and the semimembranosus tendon (Gr 5.38, 5.47C) may become inflamed to form a Baker’s (popliteal) cyst (e.g., http://emedicine.medscape.com/article/387399-overview ). This bursa usually communicates with the synovial cavity of the knee joint and may enlarge when the knee joint becomes inflamed (e.g., in rheumatoid arthritis). Rarely, a Baker’s cyst may become large enough to interfere with knee flexion or compress popliteal neurovascular structures. If the cyst ruptures, irritating fluid enters the posterior compartment of the leg and may cause symptoms resembling thrombophlebitis.
The following dissection is to be performed only at even-numbered tables on one lower extremity!
13. ON ONE LOWER EXTREMITY ONLY OF EVEN-NUMBERED TABLES, make a transverse incision across the quadriceps femoris tendon 3-4 cm superior to the patella. The incision should extend down to the bone of the femur. Now make a vertical incision on each side parallel to the patella and patellar ligament about 1 cm away. Reflect the patella and patellar ligament downward to open the anterior joint cavity. Studying the interior of the joint will be facilitated if the knee is tied or blocked in a position of flexion.
14. Identify the infrapatellar synovial fold that ascends posteriorly from the inferior pole of the patella to the intercondylar notch of the femur (Fig. 9; Gr 5.43; N495). Verify that the infrapatellar synovial fold covers an infrapatellar fat pad. Remove the infrapatellar fold to expose the anterior attachments of the anterior and posterior cruciate ligaments (Fig. 8C, 9A; Gr 5.44A; N497). The anterior cruciate ligament courses posterosuperiorly and laterally from the anterior intercondylar area of the tibia toward the lateral femoral condyle. It is medial to the posterior cruciate ligament, of which only the anterior attachment on the medial femoral condyle is visible in this dissection.
15. Identify the medial meniscus and find its attachment to the deep portion of the tibial collateral ligament. To do this the tendons of the pes anserinus—sartorius, gracilis, and semitendinosus—may have to be cut and reflected. Clean the tibial collateral ligament. It is a flat, wide band mostly consisting of a thickening of the articular capsule (Gr 5.41, 5.45A; N494, 497).
16. Locate the lateral meniscus. Verify that it does not have an attachment to the fibular collateral ligament. To expose the fibular collateral ligament, palpate the head of the fibula and a strong cord-like band connecting it to the lateral femoral epicondyle. Remove the more superficial tissue to expose the fibular ligament. If you have difficulty finding it, remember that the tendon of the biceps femoris muscle splits around the ligament and may obscure your view (Gr 5.47B-C; N494, 495).
17. Place a gloved finger into the suprapatellar bursa extending superiorly deep to the vastus intermedius. The bursa’s continuity with the knee joint cavity provides a ready pathway for the spread of infection and a place for joint effusion to hide. Carefully reflect the vastus intermedius to expose a few deep fascicles of muscle attaching to the synovium of the suprapatellar bursa. This is the articularis genus muscle (Gr 5.47A-B, 5.52A; N495, 499). XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.