Leg and Popliteal Area
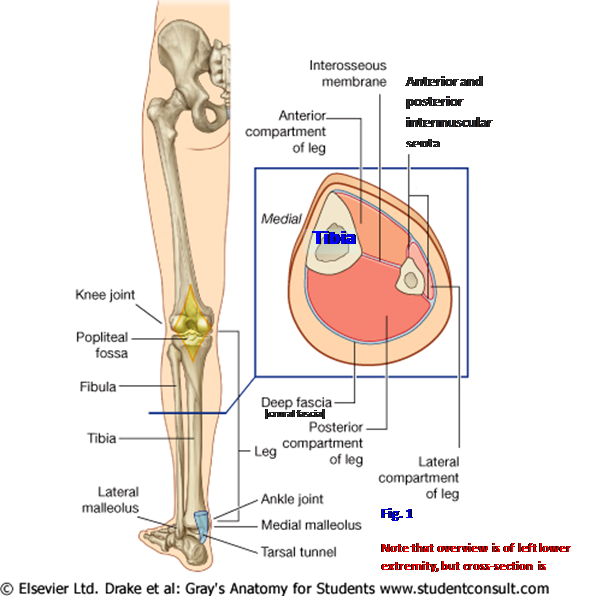
The leg is the region of the lower extremity between the knee and the ankle (Gr 5.1). It has a skeleton consisting of the medial tibia and the lateral fibula (Gr 5.60, Table 5.8 [p. 405]; Ne 501, 502). The tibia helps to form both the knee and ankle joints, but the fibula contributes only to the ankle joint. The tibia and fibula are connected by a tough interosseous membrane (Gr 5.54B, 5.55A; Ne 502), which helps to divide the leg into compartments—anterior, lateral, and posterior (Fig. 1; Gr 5.89; Ne 510).
The tibia consists of a stout shaft (body) and enlarged superior (proximal) and inferior (distal) ends (Gr 5.1, 5.60; Table 5.8 [p. 405]; Ne 501). The features of the proximal tibia were described previously in the “Gluteal Region and Posterior Thigh” dissection instructions.
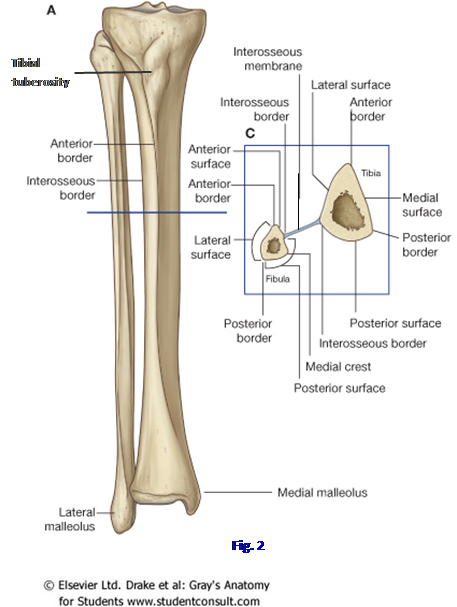
The shaft of the tibia is vertically oriented within the leg, unlike the angled femur within the thigh. The shaft is roughly triangular in cross-section, with three borders—anterior, medial, and interosseous—and three surfaces—medial, lateral, and posterior. The anterior border is the most prominent and is easily palpable (Fig. 2). The anterior border and the adjacent medial surface are subcutaneous through most of their length and, therefore, are vulnerable to traumatic injury. A fracture involving the subcutaneous
portion of the tibia is likely to be a compound fracture (i.e., a fracture that tears the skin) with the associated danger of bone infection (osteomyelitis). The tibial tuberosity is located at the upper end of the anterior border, where it provides attachment for the patellar ligament. The tuberosity may be enlarged as a result of Osgood-Schlatter disease during adolescence. The tibial shaft is thinnest at the junction of the middle and distal thirds, and this is the most frequent site of fracture.
The interosseous border of the tibia faces the fibula laterally. It gives attachment to the crural interosseous membrane. The posterior surface of the tibia has a rough diagonal ridge, the soleal line, for attachment of one of the superficial calf muscles, the soleus (Gr 5.60, 5.61C-D; Ne 501, 503, 505).
The inferior end of the tibia is expanded on the medial side as the medial malleolus (Fig. 2). The lateral surface of the medial malleolus and the inferior surface of the shaft are covered with articular cartilage and articulate with the talus at the ankle (talocrural) joint. The medial malleolus gives attachment to the strong deltoid ligament, which reinforces the articular capsule of the ankle joint medially.
The fibula is the slender lateral bone of the leg (Figs. 1, 2). It bears minimal weight and serves mainly for muscle attachments and to help form the ankle joint. The fibula has a proximal head, which articulates with the lateral condyle of the tibia; therefore, the fibula does not normally participate in the knee joint. The head of the fibula is attached to the shaft by the neck of the fibula, where the common fibular nerve is frequently injured (Gr 5.23A-B, 5.37, 5.55; Table 5.1 [pp. 348-349]; Ne 504, 508, 530A).
The fibula has a slender, twisted shaft (body). The middle of the shaft is frequently used for vascularized bone grafts. Distally the fibula is expanded laterally as the lateral malleolus, which ends more inferiorly than the medial malleolus (Gr 5.60B, 5.69, 5.70, 5.73; Ne 501, 502, 514). The medial surface of the lateral malleolus articulates with the talus as part of the ankle joint. The lateral malleolus gives attachment to three ligaments that reinforce the capsule of the ankle joint—the anterior talofibular, calcaneofibular, and posterior talofibular ligaments (Gr 5.70, 5.71, 5.72A; Ne 513, 515). The anterior talofibular ligament is the most frequently sprained ligament at the ankle joint, followed by the calcaneofibular ligament. This usually occurs when the plantarflexed foot is forced into inversion. The deltoid ligament resists eversion and is so strong that its attachment to the medial malleolus usually is avulsed before the ligament ruptures.
The tibia and fibula are connected by superior and inferior tibiofibular joints and by the crural interosseous membrane (Gr 5.54B-C, 5.55A, 5.69, 5.70, 5.71; Ne 501, 502). The superior tibiofibular joint is a plane synovial joint between the head of the fibula and a facet located posterolaterally on inferior surface of the lateral tibial condyle. The fibrous articular capsule is reinforced by anterior and posterior superior tibiofibular ligaments.
1. Study the features of the tibia and fibula on a skeleton or on individual bones. Identify the anterior, medial, and interosseous borders of the shaft of the tibia. Realize that the medial surface of the shaft, which is located between the anterior and medial borders, is subcutaneous. Verify this by palpating the anterior border and medial surface of your own tibia. The medial malleolus is also subcutaneous. Look at the smooth articular surface on its lateral side, which is continuous with the articular surface on the distal surface of the shaft.
2. Identify the head and neck of the fibula. Find the interosseous border facing the tibia. Study the lateral malleolus and its relationships. Verify that it extends more inferiorly than the medial malleolus. XXX
The crural interosseous membrane connects the interosseous borders of the tibia and fibula and provides for muscle attachments. The anterior tibial artery reaches the anterior compartment of the leg through an oval opening in the upper part of the interosseous membrane (Gr 5.55A, 5.57B, Table 5.11 [p. 423]; Ne 506, 508). The perforating branch of the fibular artery pierces the membrane inferiorly to reach the dorsum of the foot.
The inferior tibiofibular joint is a fibrous (syndesmotic) joint between a convex surface on the medial side of the lower fibula and the concave fibular notch of the tibia (Gr 5.69-5.71, Table 5.9 [p. 411, right]; Ne 502, 515). The two bones are connected at the joint by an interosseous tibiofibular ligament, which is continuous above with the crural interosseous membrane. The joint is strengthened by anterior and posterior inferior tibiofibular ligaments. The lower deep portion of the posterior inferior tibiofibular ligament forms the inferior transverse tibiofibular ligament, which extends below the junction of the tibia and fibula to help form part of the surface that articulates with the talus at the ankle joint (Gr 5.71, 5.75).
Only limited movement is allowed between the tibia and fibula. The most important of these movements is a slight forced separation of the distal portions of the tibia and fibula by the wider anterior portion of the trochlea of the talus during dorsiflexion (upward movement) of the foot. This makes the dorsiflexed position of the foot more stable than plantar flexion, which is the position in which most ankle injuries occur.
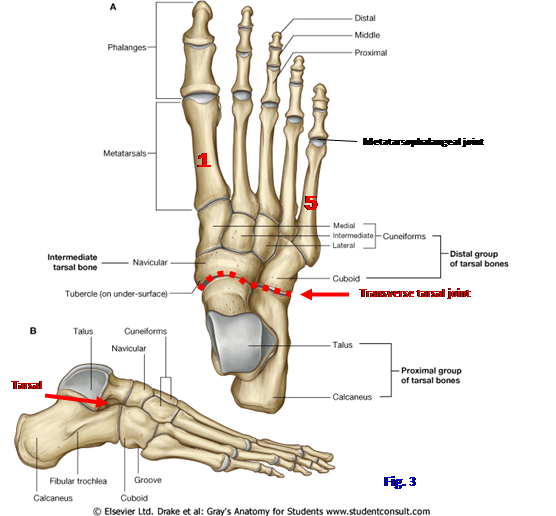
The foot will be studied in more detail during the next dissection, but an overview of its skeleton is helpful in understanding the distal attachments of the leg muscles (Fig. 3; Gr 5.68, Tables 5.13 [p. 429] and 5.15 [p. 431]; Ne 511, 512). The foot has 7 tarsal bones, 5 metatarsal bones, and 14 phalanges. The tarsal bones are the talus, calcaneus, navicular, three cuneiform bones, and the cuboid. The talus consists of a head, neck, and body. The body has a superior part (trochlea) that articulates with the tibia and fibula at the ankle (talocrural) joint. The anterior part of the trochlea is wider than the posterior part so that the ankle joint is more stable when the foot is rotated upward toward the leg (dorsiflexion) than downward toward the floor (plantar flexion). Inferiorly the talus forms the subtalar joint with the calcaneus. The head of the talus articulates anteriorly with the navicular bone at the talonavicular (talocalcaneonavicular) joint, which is the medial part of the transverse tarsal joint (Fig. 3 -- -- -- -- , Gr Table 5.16 [p. 442]; Ne 511, 512).
The large calcaneus is the heel bone (Fig. 3; Gr 5.68; Ne 511-513). Its tuberosity is the posterior, weight-bearing portion that transmits 50% of the weight on that foot to the ground. Medially the calcaneus has a horizontal shelf, the sustentaculum tali, which helps to support the talus (Gr 5.68B & D-E; Ne 511-513). The calcaneus articulates superiorly with the talus and anteriorly with the cuboid. The latter articulation, the calcaneocuboid joint, forms the lateral part of the transverse tarsal joint (Fig. 3 -- -- -- -- , Gr Table 5.16 [p. 442]; Ne 511, 512).
The navicular bone is interposed between the head of the talus posteriorly and the three cuneiform bones anteriorly (Fig. 3). It articulates with those and laterally with the cuboid bone. The most prominent feature of the navicular is the navicular tuberosity. The three cuneiform bones are the medial (1st), intermediate (2nd), and lateral (3rd) cuneiforms. They form tarsometatarsal joints with the first three metatarsal bones. The lateral cuneiform also articulates laterally with the cuboid bone.
The cuboid is the tarsal bone located lateral to the navicular and lateral cuneiform bones between the calcaneus proximally and the fourth and fifth metatarsal bones distally (Fig. 3). Its most notable features are on its plantar (inferior) surface, where an almost transverse ridge is the tuberosity of the cuboid. It is located just behind the groove for the tendon of the fibularis longus muscle (Gr 5.68B, 5.82; Ne 511, 512).
The five metatarsal bones of the foot correspond to the metacarpal bones of the hand but are more substantial in structure (Fig. 3; Gr 5.68; Ne 511, 512). They articulate proximally at tarsometatarsal joints and distally at metatarsophalangeal joints (Gr Table 5.16 [p. 442]; Ne 511, 512). Each consists of a proximal base, intermediate shaft (body), and distal head (Gr 5.68C; Ne 511). The metatarsals are numbered 1 to 5 from the medial (great toe) side. The first metatarsal is shorter and thicker than the more lateral metatarsal bones because its head bears twice as much weight. The second metatarsal is the longest, and its base fits into a recess formed because the intermediate cuneiform bone is shorter than the medial and lateral cuneiforms (Gr 5.68A-B; Ne 511). The fifth metatarsal bone has a prominent lateral tuberosity on its base for attachment of the fibularis brevis tendon.
The great toe has only proximal and distal phalanges (Fig. 3; Gr 5.68A-B; Ne 511). Toes 2-5 have proximal, middle, and distal phalanges. Like the larger metatarsal bones, the phalanges are miniature long bones with a base, shaft, and head. The proximal interphalangeal (PIP) joint is formed between the proximal and middle phalanges, and the distal interphalangeal (DIP) joint is formed between the middle and distal phalanges.
3. Examine the bones of the foot on an intact skeleton and on an x-ray. Find the head, neck, and body of the talus. Note that the body of the talus forms a superior tenon (projection) that fits into a mortise (slot or recess) formed by the medial and lateral malleoli and the distal end of the tibial shaft at the ankle (talocrural) joint. Verify that the superior part of the body, or trochlea, is wider anteriorly than posteriorly. The head of the talus articulates anteriorly with the navicular bone at the talonavicular joint, which is the medial part of the transverse tarsal joint. Identify the lateral part of the transverse tarsal joint, the calcaneocuboid joint (Fig. 3A).
4. Identify the prominent posterior tuberosity of the calcaneus, which transfers body weight to the ground. On the medial side of the calcaneus find the horizontal sustentaculum tali, which helps to support the talus. On the lateral side look for a small projection, the fibular trochlea, which may be present. Superiorly the calcaneus articulates with the talus at the subtalar joint. Look at the talus and calcaneus from the lateral side. Identify a gap between articular surfaces of the two bones, the tarsal sinus, which is apparent on radiographs (Fig. 3; Gr 5.80; N512).
5. Note the tuberosity of the navicular bone. It is easily palpable on your own foot. Identify the medial, intermediate, and lateral cuneiform bones. Each articulates proximally with the navicular bone and distally with a metatarsal bone at a tarsometatarsal joint. The lateral cuneiform also articulates with the cuboid bone.
6. Turn your attention to the cuboid bone. Proximally it articulates with the calcaneus at the calcaneocuboid joint. Medially it articulates with the navicular and lateral cuneiform bones. Distally the cuboid forms tarsometatarsal joints with the fourth and fifth metatarsal bones.
7. The metatarsal bones are numbered 1-5 from the side of the great toe. Each has a proximal base, intermediate shaft, and distal head. Note in the articulated foot that only the heads of the metatarsal bones make contact with the floor. The weight on a lower extremity is normally transmitted to the ground only at the tuberosity of the calcaneus (50%) and the heads of the metatarsal bones (50%).
8. The great toe has only proximal and distal phalanges. The other four digits also have a middle phalanx. Verify this. XXX
The subcutaneous connective tissue (superficial fascia) of the leg contains superficial veins and lymphatic vessels and cutaneous nerves (Fig. 4; Gr 5.3, 5.5-5.7; Ne 471-473). The great saphenous vein was seen in the “Anterior and Medial Thigh” dissection ascending through the thigh to end in the femoral vein. The great saphenous arises from the medial end of the dorsal venous arch of the foot and ascends anterior to the medial malleolus. It is accompanied in the leg by the saphenous nerve (Gr 5.63A; Ne 471), which is a branch of the femoral nerve descending from the adductor canal. These relationships are important because the great saphenous vein can be accessed rapidly in an emergency by a skin incision anterior to the medial malleolus (saphenous cutdown). During this procedure the saphenous nerve may be injured to produce pain or numbness along the medial side of the foot.
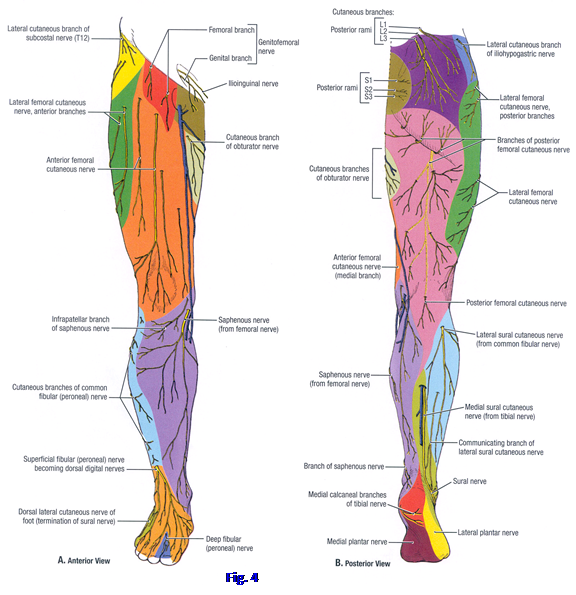
The small saphenous vein arises from the lateral side of the dorsal venous arch of the foot. It ascends posterior to the lateral malleolus and passes up the middle of the calf to pierce the popliteal fascia and drain into the popliteal vein. The small saphenous vein is accompanied by a nerve that changes names as it descends: the medial sural cutaneous nerve, sural nerve, and dorsal lateral cutaneous nerve of the foot (Fig. 4; Gr 5.3; Ne 472).
The cutaneous nerves of the leg are branches of the femoral, tibial, and common fibular nerves (Fig. 4; Gr 5.3, 5.5A; Ne 471, 472). The saphenous nerve was seen earlier descending from the adductor canal onto the medial side of the leg. This branch of the femoral nerve supplies the skin of the medial side of the leg and foot. It may inadvertently be included in a ligature or cut during a saphenous cutdown to provide intravenous access via the great saphenous vein.
The medial sural cutaneous nerve is a branch of the tibial nerve that accompanies the small saphenous vein distally (Fig. 4B; Gr 5.3, 5.5B; Ne 472, 504, 528). It is joined by a communicating branch from the lateral sural cutaneous nerve (sural communicating nerve) to form the sural nerve at a variable level on the calf. The lateral sural cutaneous nerve is a branch of the common fibular nerve. The lateral sural cutaneous nerve innervates the skin on the lateral side of the leg, extending onto the anterior surface. The superficial fibular branch of the common fibular nerve supplies cutaneous innervation to the lower anterolateral leg and dorsum of the foot.
9. Remove any remaining skin from the front and sides of the leg. Clean the superficial veins and cutaneous nerves in the superficial fascia of the leg. Find the great saphenous vein ascending anterior to the medial malleolus with the saphenous nerve. Verify this relationship. More laterally on the anterior leg find the superficial fibular nerve piercing the crural fascia to supply the lower third of the leg and the dorsum of the foot. Its distribution to the foot will be studied during the next lab. XXX
The deep fascia of the leg is the tough crural fascia (Gr 5.8A & C; Ne 471, 510). It is continuous superiorly with the fascia lata of the thigh and inferiorly with fascia on the dorsal and plantar surfaces of the foot. Medially the crural fascia blends with the periosteum of the subcutaneous anterior border and medial surface of the tibia (Figs. 1, 5; Gr 5.89, 5.91; Ne 510). Laterally it sends anterior and posterior intermuscular septa to attach to the fibula.
The bones and connective tissue septa of the leg subdivide it into osseofibrous compartments (Figs. 1, 5; Gr 5.89, 5.91; Ne 510). The anterior compartment is located anterior to the interosseous membrane and parts of the tibia and fibula. It is medial to the anterior intermuscular septum. The crural fascia over the upper part of the anterior compartment is especially dense and gives attachment to muscles of the compartment. The anterior compartment is referred to as the dorsiflexor compartment because its muscles rotate the dorsal surface of the foot upward toward the leg. The nerve supply is from the deep fibular nerve, and the blood supply is mainly from the accompanying anterior tibial artery (Gr 5.54A, 5.55A; Ne 508, 530).

The lateral compartment is located between the anterior and posterior intermuscular septa anterolateral to the fibula (Figs. 1, 5; Gr 5.55A, 5.58, 5.89, 5.91; Ne 509, 510). It is the evertor compartment because the main action of its two muscles is to turn the sole of the foot outward. Its nerve is the superficial fibular nerve. The lateral compartment doesn’t have a large artery coursing through it. Rather it is supplied by branches, mainly from the fibular artery of the posterior compartment, that perforate the intermuscular septa.
The posterior compartment of the leg has a more complicated organization than the anterior and lateral compartments (Figs. 1, 5; Gr 5.61A-C, 5.62A & C, 5.89, 5.91; Ne 504-506, 510, 529). It is located posterior to the tibia, interosseous membrane, fibula, and posterior intermuscular septum. A transverse intermuscular septum subdivides the muscles of the posterior compartment into superficial and deep groups. The posterior compartment is the plantar flexor compartment because the main actions of its muscles are to move the sole of the foot and toes toward the ground (plantar flexion). The terms “dorsiflexion” and “plantar flexion” are typically employed by anatomists to describe ankle movements to avoid confusion with the use of the terms “flexion” and “extension” by neurophysiologists, which is based on movements relative to gravity rather than on the angle between two body segments.
The posterior crural compartment is supplied by the tibial nerve and the posterior tibial artery. A large lateral branch of the posterior tibial artery, the fibular artery, supplies the lateral part of the posterior compartment (Gr 5.62A & C, Table 5.11 [p. 423]; Ne 506). The fibular artery also sends branches through the posterior intermuscular septum to the lateral compartment, and sends a perforating branch through the interosseous membrane to the anterior compartment.
The compartments of the leg are confined spaces with unyielding walls formed by bone and dense fascia. An increase in the volume of the contents of a compartment (e.g., due to inflammation or bleeding) may compromise the blood supply and result in ischemic necrosis of nerves and muscles (compartment syndrome) (e.g., see http://www.merck.com/mmpe/sec21/ch309/ch309c.html ). The anterior compartment is a frequent location, often as a result of tibial injuries. Muscle is replaced by scar tissue that undergoes contracture (Volkmann’s ischemic contracture [Note: the term “Volkmann’s ischemic contracture” is reserved for the upper extremity by some clinicians, although the process in the lower extremity, though less frequent, is exactly the same]). Early intervention by surgical incision of the crural fascia (fasciotomy) may prevent or reduce injury to compartmental structures.
The crural fascia has thickened bands distally that form retinacula to help to prevent bowstringing of the tendons of leg muscles during foot movements (Gr 5.5B, 5.56, 5.59B-C; Ne 507, 509, 517, 518). The superior extensor retinaculum passes between the tibia and fibula just superior to the malleoli. The inferior extensor retinaculum is a Y-shaped thickening of crural fascia that attaches laterally to the anterosuperior surface of the calcaneus. The upper limb of the Y attaches medially to the medial malleolus, and the lower limb blends with fascia of the foot.
The superior fibular retinaculum spans the groove between the lateral malleolus and calcaneus and overlies a common synovial sheath for the fibularis longus and fibularis brevis tendons (Gr 5.59B-C; Ne 509, 517). The inferior fibular retinaculum passes between two points on the calcaneus. The common synovial sheath of the tendons of fibularis longus and brevis split into separate synovial sheaths as the tendons begin to diverge to pass deep to the inferior fibular retinaculum.
The flexor retinaculum passes from the medial malleolus to the tuberosity of the calcaneus (Gr 5.62A & C; Ne 504-506, 517). The space so formed is the tarsal tunnel, which may be a site of entrapment for the tibial nerve. Also traversing the tarsal tunnel are the posterior tibial artery and the tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles. These structures have a specific relationship within the tarsal tunnel that will be discussed later.
10. Remove the skin from the dorsal surface and sides of the foot. Clean the crural fascia and find the extensor retinacula at the ankle. Anteriorly clean the superior extensor retinaculum passing between the tibia and fibula just above the malleoli. Clean the inferior extensor retinaculum. Its lateral attachment is to the calcaneus and its medial attachments are a superior limb to the medial malleolus and an inferior limb blending with fascia of the foot. The superior and inferior fibular retinacula and the flexor retinaculum will be studied later in the period. XXX
The anterior compartment of the leg is located between the anterior border of the tibia medially and the anterior intermuscular septum laterally (Fig. 5; Gr 5.53, 5.54A, 5.58, 5.89, 5.91A-C; Table 5.8 [p. 405]; Ne 507-510). It is, therefore, anterior to the interosseous membrane and portions of the tibia and fibula. There are four muscles in the anterior compartment. The most medial of these is the tibialis anterior. It takes origin from the lateral condyle and superior half of the lateral surface of the tibia, the adjacent interosseous membrane, and the overlying crural fascia. The tibialis anterior’s long tendon begins halfway down the leg and passes deep to the extensor retinacula to insert into the medial and inferior surfaces of the medial cuneiform and base of the first metatarsal bone (Gr 5.64A-B; Ne 516-519). The muscle dorsiflexes the ankle and works with the tibialis posterior to turn the sole of the foot medially (inversion).
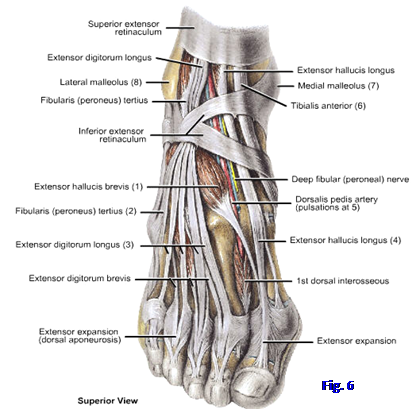
The most lateral of the anterior leg muscles is the extensor digitorum longus (Fig. 5; Gr 5.53B, 5.56, 5.58B; Table 5.8 [p. 405]; Ne 507, 509, 518). It takes origin mainly from the upper ¾ of the fibula and adjacent interosseous membrane and from the anterior intermuscular septum. It gives rise to four tendons just above the ankle. The four tendons enter the dorsum of toes 2-5, where each forms an extensor expansion (extensor hood) over its proximal phalanx (Fig. 6; Gr 5.56B; Ne 518, 519). Each tendon divides into two lateral bands that attach to the distal phalanx of its digit and a central band that inserts into the middle phalanx. The extensor expansions of digits 2-4 are joined on their lateral side by the tendons of the extensor digitorum brevis, which is an intrinsic muscle of the foot. The extensor digitorum longus extends toes 2-5 and helps to dorsiflex the ankle.
The fibularis tertius is usually considered a separate part of the extensor digitorum longus muscle (Fig. 6; Gr 5.56B, 5.58B, 5.59B-C; Ne 509, 517, 518). It takes origin from the inferior 1/3 of the fibula and adjacent interosseous membrane, where it is fused with the extensor digitorum longus. Its tendon diverges from those of the extensor digitorum longus to attach to the dorsal surface of the fifth metatarsal bone near its base. The fibularis tertius is a weak muscle that aids in dorsiflexion and eversion of the foot. It may be absent.
The fourth muscle in the anterior compartment of the leg is the extensor hallucis longus (Fig. 6; Gr 5.53B, 5.54A, 5.56B, 5.89; Ne 507, 518, 519). It is hidden by the tibialis anterior and extensor digitorum longus at its origin from the middle third of the anterior fibula and interosseous membrane. Its tendon emerges into view in the distal third of the leg and passes deep to the extensor retinacula. The extensor hallucis longus tendon courses distally on the dorsum of the foot and into the great toe, where it attaches into the base of the distal phalanx. This muscle extends the great toe and helps to dorsiflex the ankle. The tendon of the extensor hallucis longus is a useful landmark for taking the pulse of the dorsalis pedis artery, which lies just lateral to it (Gr 5.56B, 5.57B; Ne 518, 519).
The deep fibular nerve, which is a branch of the common fibular nerve, supplies the muscles of the anterior compartment (Gr 5.54A, 5.55A, Table 5.1 [pp. 348-349]; Ne 508, 530). It descends deep within the compartment in company with the anterior tibial artery. Leaving the anterior surface of the interosseous membrane distally, it crosses the lower end of the tibia to enter the foot and supply its intrinsic dorsal muscles. The nerve supplies a small cutaneous area between the great and second toes (Fig. 4).
The common fibular nerve is the most commonly injured nerve in the lower extremity because of its exposed position where it winds around the neck of the fibula. In addition to direct trauma or a fracture of the fibula, it may be damaged by severe stretching during dislocation of the knee. A lesion of the common fibular nerve or its deep fibular branch results in footdrop with inability to dorsiflex the foot. In order to prevent his toes from dragging on the ground during the swing phase of gait, the patient compensates by swinging the limb out laterally or flexing his hip and knee joints to raise the foot high off the ground (steppage gait).
The anterior tibial artery is the smaller terminal branch of the popliteal artery (Gr 5.54A, 5.55A, 5.62A; Table 5.11 [p. 423]; Ne 500, 506, 508). It enters the anterior compartment through a gap in the upper part of the crural interosseous membrane and descends on its anterior surface in company with the deep fibular nerve. As the anterior tibial artery passes an imaginary line joining the malleoli, it changes names to become the dorsalis pedis artery.
11. Make a vertical incision in the crural fascia down the length of the anterior compartment of the leg. Clean and preserve the superior and inferior extensor retinacula on one leg as you reflect and remove the fascia. The retinacula can be cut on the other leg. The crural fascia may be difficult to remove, especially over the upper part of the compartment, because the underlying muscles attach to it.
12. Clean the muscles in the anterior compartment. The tibialis anterior is the most medial of these. It lies just lateral to the shaft of the tibia, from which it takes part of its origin. Clean the stout tendon of the tibialis anterior inferiorly as far as the extensor retinacula. Its attachment to the medial cuneiform and the base of the first metatarsal will be seen during the dissection of the foot, but examine the attachment sites on a skeleton.
13. Lateral to the belly of the tibialis anterior identify the belly of the extensor digitorum longus. Trace its tendons distally to where they pass deep to the extensor retinacula. At what level do the four tendons form? Their course to digits 2-5 will be seen later.
14. Find the fibularis tertius, if one is present. It is considered a separate part of the extensor digitorum longus. The fibularis tertius’ tendon attaches to the dorsum of the fifth metatarsal and may be seen starting to diverge from the tendons of extensor digitorum longus near the inferior extensor retinaculum.
15. The extensor hallucis longus is covered by the tibialis anterior and extensor digitorum longus in the upper 2/3 of the leg. Find the extensor hallucis longus tendon just lateral to that of tibialis anterior in the lower 1/3 of the leg and follow it proximally to the muscle belly by bluntly separating the bellies of the tibialis anterior and extensor digitorum longus muscles. The tendon’s attachment to the distal phalanx of the great toe will be seen during dissection of the foot.
16. Just lateral to the extensor hallucis longus tendon, near the inferior extensor retinaculum, locate the anterior tibial artery and deep fibular nerve. The artery becomes the dorsalis pedis at an imaginary line connecting the medial and lateral malleoli. Attempt to find branches of the anterior tibial artery. Near the malleoli are small anterior medial and anterior lateral malleolar arteries. Find the perforating branch of the fibular artery piercing the interosseous membrane to anastomose with the anterior lateral malleolar artery. Follow the anterior tibial artery proximally along the interosseous membrane. Near where it traverses a gap in the interosseous membrane to enter the anterior compartment, look for the anterior tibial recurrent artery (Gr 5.48A & D, 5.55A; N500, 508). Don’t follow it through the substance of the tibialis anterior muscle, but be aware of its contribution to the genicular anastomosis around the knee.
17. The thin deep fibular nerve accompanies the anterior tibial artery, usually on its lateral side. It is one of the terminal branches of the common fibular nerve, which will be seen dividing during dissection of the lateral compartment. The deep fibular nerve pierces the anterior intermuscular septum and extensor digitorum longus muscle as it enters the anterior compartment. XXX
The lateral compartment of the leg (lateral crural compartment) is located between the anterior and posterior intermuscular septa, superficial to the fibula (Figs. 1, 5; Gr 5.55, 5.58, 5.89, 5.91B-C, Table 5.9 [p. 411]; Ne 508-510, 517). It contains two muscles. The longer and more superficial muscle is the fibularis (peroneus) longus. It takes origin from the head and upper 2/3 of the lateral surface of the fibula and from the two intermuscular septa. The fibularis longus tendon descends posterior to the lateral malleolus and deep to the superior fibular retinaculum (Gr 5.59; Ne 515, 517). It continues anteriorly and inferiorly deep to the inferior fibular retinaculum, where it is inferior to the fibular trochlea of the calcaneus. The tendon turns around the lateral surface of the cuboid bone and crosses the plantar part (sole) of the foot to reach the medial cuneiform and base of the first metatarsal bone. The fibularis longus is an evertor of the foot. Along with the tibialis anterior, which also inserts on the medial cuneiform and first metatarsal bones, it forms a sling that probably helps to support the medial longitudinal arch of the foot.
The fibularis (peroneus) brevis muscle is shorter than the fibularis longus and has a belly that lies deep to it (Fig. 5; Gr 5.55, 5.58B, 5.89; Ne 507-510). It takes origin from the inferior 2/3 of the lateral surface of the fibula and the intermuscular septa. The tendon lies anterior to that of fibularis longus, with which it shares a tendon sheath as it passes behind the lateral malleolus. The fibularis brevis tendon continues anteriorly deep to the inferior fibular retinaculum, superior to the fibular trochlea. By the time it reaches the inferior fibular retinaculum it has acquired its own tendon sheath. The insertion is into the tuberosity at the base of the fifth metatarsal bone. The fibularis brevis is an evertor of the foot. If the foot is forcefully inverted while the fibularis brevis is contracting, the muscle may avulse the tuberosity of the fifth metatarsal.
The nerve of the lateral compartment is the superficial fibular nerve (Gr 5.55, 5.58B, Table 5.1[pp. 348-349]; Ne 508, 530). It is one of the terminal branches of the common fibular nerve, which enters the lateral compartment to divide deep to the fibularis longus muscle (Gr 5.55A; Ne 530). After supplying the fibularis longus and brevis muscles, the superficial fibular nerve pierces the crural fascia to innervate the skin of the distal third of the anterolateral leg and most of the dorsum of the foot (Fig. 4).
The lateral compartment has no major artery traversing it. The compartment is supplied mainly by branches of the fibular artery that pierce the posterior intermuscular septum from the posterior compartment (Gr 5.62C, Table 5.11 [p. 423]; Ne 506). A small upper part of the lateral compartment receives branches from the anterior tibial artery that pierce the anterior intermuscular septum.
18. Clean the superior and inferior fibular retinacula. Find the superior retinaculum as a thickening of deep fascia passing between the lateral malleolus and the upper surface of the calcaneus. The inferior fibular retinaculum attaches to the superolateral part of the calcaneus, where it is continuous with the inferior extensor retinaculum. Preserve the fibular retinacula on the same lower extremity where the extensor retinacula were preserved. Remove the rest of the crural fascia over the lateral compartment.
19. Clean the fibularis longus muscle. Trace its tendon behind the lateral malleolus until it passes deep to the superior fibular retinaculum. Its further course will be seen during dissection of the foot.
20. Once again find the common fibular nerve at the neck of the fibula. Push a probe through the fibularis longus superficial to the nerve and carefully incise the overlying muscle. Free the inferior segment of the fibularis longus belly from its attachment to the fibula and reflect it downward to expose the fibularis brevis. Follow the tendon of fibularis brevis as it descends behind the lateral malleolus, deep to the superior fibular retinaculum and anterior to the tendon of fibularis longus.
21. Turn your attention back to the common fibular nerve. Clean it where it divides into the superficial and deep fibular nerves. Follow the superficial fibular nerve distally until it enters the dorsum of the foot. XXX
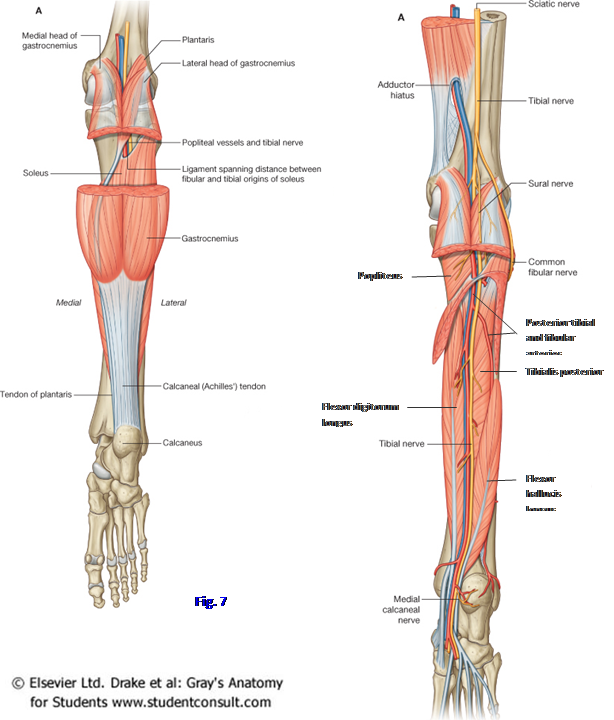
The posterior compartment of the leg (posterior crural compartment) is the largest of the three compartments (Figs. 1, 5, 7; Gr 5.61, 5.62A-C, 5.89, 5.91, Table 5.10 [p. 414]; Ne 504-506, 510). It is subdivided into superficial and deep muscle groups by the transverse intermuscular septum, which passes medially from the posterior intermuscular septum laterally to blend with periosteum of the tibia. The superficial group of muscles in the posterior compartment are the gastrocnemius, soleus, and plantaris. The most superficial calf muscle is the gastrocnemius (Gr 5.61A-B; Ne 469, 504). It has medial and lateral heads of origin from the femur just superior to the medial and lateral femoral condyles, respectively. The two heads converge to form the prominent muscular mass of the upper calf. Approximately halfway down the leg, the muscle gives rise to the thick calcaneal (Achilles) tendon, which inserts on the posterior surface of the calcaneal tuberosity. The calcaneal tendon bursa separates the calcaneal tendon from the upper part of the bone’s posterior surface (Gr 5.63B, 5.71; Ne 509). The gastrocnemius is a powerful plantar flexor of the foot, acting when we “stand on our toes” or jump off the ground by rapid plantar flexion of the foot. It is a two-joint muscle that also crosses the knee joint, so it can flex the knee when it is not plantar flexing the ankle.
The soleus is located deep to the gastrocnemius (Gr 5.58A-B, 5.61, 5.62A; Ne 505, 509, 510). It is a large, thick muscle, but flatter than the prominent gastrocnemius. The soleus takes origin from the head of the fibula, the soleal line of the tibia, and a tendinous arch between them. Inferiorly, the soleus joins the gastrocnemius in forming the calcaneal tendon. The soleus is a plantar flexor of the foot at the ankle joint. It consists predominantly of fatigue-resistant type 1 skeletal muscle fibers and is a postural muscle that is continuously active during quiet standing. The soleus pulls posteriorly on the tibia and fibula to counteract the natural tendency toward dorsiflexion (and falling down) that exists because the line of gravity passes anterior to the axis of the ankle joint. The soleus does not cross the knee joint and cannot move it.
Together the gastrocnemius and soleus form the triceps surae, which is so-named because it has two heads from the gastrocnemius and one from the soleus. Paralysis of the triceps surae or rupture of the calcaneal tendon (third degree strain) greatly weakens plantar flexion, making it impossible to stand on the toes and making ambulation difficult. The tendon is prone to rupture after a history of chronic tendinitis. The patient with a paralyzed gastroc-soleus develops a triceps surae gait, in which the pelvis drops on the affected side during the (weight-bearing) stance phase of walking. How does this differ from a gluteus medius gait?
The plantaris is a vestigial muscle with a small, triangular belly and a long, slender tendon (Fig. 7; Gr 5.23B-D, 5.37; Ne 505). It is absent in up to 10% of the population. The plantaris takes origin from the inferior end of the lateral supracondylar line of the femur, just above the lateral head of the gastrocnemius. Its tendon descends medially between the gastrocnemius and soleus to insert into the calcaneus, usually fusing with the calcaneal tendon. The tendon is frequently mistaken for a nerve during dissection. The plantaris contributes little force of contraction to plantar flexion and is sometimes transplanted in reconstructive surgery of the forearm and hand.
The deep group of posterior compartment muscles lies deep to the transverse intermuscular septum (Fig. 5). It includes one muscle that acts on the knee joint and three muscles that send tendons into the foot to move the ankle joint or/and the toes (Fig. 7; Gr 5.62A-C, 5.63A-B, 5.64A-B, Table 5.10 [p. 414]; Ne 499, 506, 510, 529). The popliteus is a flat triangular muscle that forms the inferior part of the floor of the popliteal fossa and, therefore, is located superior to the other three deep muscles. It is covered by popliteal fascia. The popliteus takes origin inside the articular space enclosed by the capsule of the knee joint but outside the synovial membrane (i.e., it is intracapsular but extrasynovial). From the lateral femoral epicondyle and the lateral meniscus (Gr 5.42, 5.47B-C; Ne 499, 506), the muscle emerges through an opening in the articular capsule to attach to the posterior surface of the tibia above the soleal line. The articular capsule is reinforced to form the arcuate popliteal ligament where the popliteus pierces it (Ne 499). The popliteus contracts to unlock the fully extended knee joint at the beginning of flexion by rotating the femur 5° laterally on the weight-bearing tibia. It also pulls the lateral meniscus posteriorly to protect it as the lateral femoral condyle moves on the lateral tibial plateau.
The other three muscles in the deep group of the posterior compartment are located inferior to the popliteus (Fig. 7; Gr 5.62A-C, Table 5.10 [p. 414]; Ne 506, 529). From medial to lateral are the flexor digitorum longus, tibialis posterior, and flexor hallucis longus. The flexor digitorum longus takes origin mainly from the posterior surface of the tibia inferior to the soleal line. It descends straight down the leg and becomes tendinous just above the medial malleolus. The tendon passes behind the medial malleolus, deep to the flexor retinaculum, posterior to the tendon of the tibialis posterior muscle (Fig. 7; Gr 5.62A & D, 5.64A-B; Ne 505, 506, 517). In the sole of the foot, the flexor digitorum longus tendon divides into four tendons, one to each of the lateral four toes. Each tendon inserts into the distal phalanx of its digit. The flexor digitorum longus flexes the distal interphalangeal (DIP) joints of toes 2-5 and helps to flex the proximal interphalangeal (PIP) joints. It also can help to plantar flex the foot at the ankle joint.
The tibialis posterior muscle lies between the flexor digitorum longus and flexor hallucis longus muscles at its origin and is largely hidden by them there (Gr 5.62, 5.64A-B; Ne 503, 506). It takes origin from the posterior surfaces of the tibia and fibula and the interosseous membrane. The tibialis posterior descends between the other two muscles until just superior to the medial malleolus, where its tendon crosses anterior to the flexor digitorum longus; therefore, the tibialis posterior tendon is the most anterior structure passing behind the medial malleolus (Fig. 7; Gr 5.62D-E, 5.63, 5.64A-B; Ne 505, 506, 517). The main insertion of the tibialis posterior is into the tuberosity of the navicular bone, but its tendon sends slips to the cuneiform and cuboid bones and the bases of metatarsal bones 2-4. The tibialis posterior inverts the ankle and helps to plantar flex it. It also contributes support to the arches of the foot.
The flexor hallucis longus muscle is the most lateral of the deep posterior compartment muscles (Fig. 7; Gr 5.62, 5.63A-B, 5.64A-B, Table 5.10 [p. 414]; Ne 506, 510, 529). It takes origin from the inferior 2/3 of the posterior surface of the fibula and adjacent interosseous membrane. The tendon passes behind the medial malleolus in the most posterior position deep to the flexor retinaculum (Ne 517). The flexor hallucis longus tendon crosses deep to the flexor digitorum tendon in the sole of the foot and inserts into the base of the distal phalanx of the great toe (Gr 5.64A; Ne 522). The flexor hallucis longus flexes the great toe and can help plantar flex the foot. It is sometimes asserted to have a special role in toe-off of the gait cycle, but this has been disputed.
The nerve of the posterior compartment is the tibial nerve (Fig. 7; Gr 5.61B-C, 5.62A & C, 5.63A; Table 5.1 [pp. 348-349]; Ne 505, 506, 529). The tibial nerve (L4-S3) is the larger of the two terminal branches of the sciatic nerve. It descends through the popliteal fossa superficial to the popliteal vein and artery and leaves the fossa between the heads of the gastrocnemius. The nerve passes deep to the tendinous arch of the soleus to enter the deep posterior compartment of the leg. The tibial nerve supplies all of the muscles in the posterior compartment of the leg. It divides just distal to the medial malleolus into the medial and lateral plantar nerves.
The posterior tibial artery is the larger terminal branch of the popliteal artery, which divides at the inferior border of the popliteus (Fig. 7; Gr 5.62A & C, 5.63A, 5.65A; Table 5.11 [p. 423]; Ne 500, 506). The artery passes deep to the tendinous arch of the soleus and descends through the deep posterior compartment with the tibial nerve. It gives off medial calcaneal and posterior medial malleolar branches before dividing into the medial and lateral plantar arteries just distal to the medial malleolus. The medial calcaneal artery supplies the medial side of the heel (Ne 522, 523). The posterior medial malleolar artery passes anteriorly across the medial malleolus to help form an arterial anastomosis around the ankle joint.
The structures traversing the tarsal tunnel deep to the flexor retinaculum have a relatively constant relationship (Fig. 7; Gr 5.63A-B; Ne 506, 517). From anterior to posterior, passing behind the medial malleolus, are the tibialis posterior (Tom), flexor digitorum longus (Dick), posterior tibial artery (a), tibial nerve (n), and the flexor hallucis longus (Harry). These relationships are easily remembered as “Tom, Dick, an’ Harry.” The pulse of the posterior tibial artery can be taken at the tarsal tunnel to help assess the peripheral circulation. To do this the patient is asked to invert the foot to relax the flexor retinaculum. A space-occupying lesion (e.g., edema due to inflammation or pregnancy) compresses the tibial nerve, resulting in pain and paresthesia over the medial heel and the sole of the foot (tarsal tunnel syndrome). The symptoms are typically precipitated by extended standing and walking. Motor deficits are less common.
The largest branch of the posterior tibial artery is the fibular (peroneal) artery (Fig. 7; Gr 5.62A & C; Ne 500, 506). Occasionally the posterior tibial artery is absent and the fibular artery enlarges to take its place (Gr 5.65C). The fibular artery descends through the lateral part of the posterior compartment deep to the flexor hallucis longus. It supplies the lateral part of the deep posterior compartment and sends branches through the posterior intermuscular septum to supply most of the blood to the lateral compartment of the leg. Its perforating branch pierces the lower part of the interosseous membrane to enter the anterior compartment of the leg (Gr 5.54A, 5.55A; Ne 506, 508). The perforating branch of the fibular artery may give rise to the dorsalis pedis artery if the anterior tibial artery is small and ends at the ankle (Gr 5.65B). In this instance, a dorsalis pedis pulse is not palpable.
A communicating branch, occasionally large, usually joins the fibular and posterior tibial arteries just above the ankle (Ne 506). Other smaller branches of the fibular artery are the posterior lateral malleolar artery and the lateral calcaneal artery. The posterior lateral malleolar artery passes forward across the lateral malleolus to participate in the anastomosis around the ankle joint. The lateral calcaneal artery supplies the lateral side of the heel.
22. Turn the cadaver to the prone position. Remove any remaining skin from the back of the leg. Once again identify the small saphenous vein and follow it toward its union with the popliteal vein. Trace the small saphenous vein distally to where it passes posterior to the lateral malleolus. Find the medial sural cutaneous nerve piercing the deep fascia of the leg (crural fascia) several centimeters below the popliteal fossa (Gr 5.3; N472). Clean the medial sural cutaneous nerve and find where it is joined by the communicating branch from the lateral sural cutaneous nerve to form the sural nerve. The level at which the sural nerve is formed is variable.
23. Clean the flexor retinaculum spanning the depression between the medial malleolus and the tuberosity of the calcaneus. Try to preserve the retinaculum on one lower extremity. Now remove the crural fascia over the posterior compartment.
24. Cut the medial and lateral heads of the gastrocnemius 2-3 cm below their origins from the femur and reflect the muscle downward to its junction with the calcaneal tendon. You will have to cut muscular branches of the tibial nerve and posterior tibial artery to do this. Briefly look for remnants of two small bursae, one between the medial head of the gastrocnemius and the semimembranosus (semimembranosus bursa) and one deep to the proximal part of the medial head of the gastrocnemius (gastrocnemius bursa) (Gr 5.38, 5.47C; N499). These bursae may be continuous.
25. Identify and clean the small plantaris muscle belly and its long, slender tendon descending medially between the gastrocnemius and soleus muscles. Note whether its tendon fuses with the calcaneal tendon or travels separately to the calcaneus. Divide the plantaris muscle near its origin and reflect it downward.
26. Study the tibial nerve, popliteal vein, and popliteal artery passing deep to the fibrous tendinous arch of the soleus muscle to enter the deep posterior compartment (Gr 5.62A & C; N505). Now detach the soleus entirely from its origin and reflect the gastroc-soleus (triceps surae) down to the attachment of the calcaneal tendon into the tuberosity of the calcaneus. This will expose the tibial nerve and posterior tibial artery. Clean the nerve as far inferiorly as the flexor retinaculum.
27. Identify the popliteus muscle emerging through a gap in the articular capsule of the knee joint (Gr 5.38, 5.47C; N499, 506). The muscle is covered by dense popliteus fascia deep to the tibial nerve and popliteal vessels. Find where the popliteal artery branches into the posterior and anterior tibial arteries near the inferior border of the popliteus. Clean the short proximal part of the anterior tibial artery that is visible from this view before it disappears through a gap in the interosseous membrane to enter the anterior compartment.
28. Clean the posterior tibial artery as it descends through the compartment in the shallow groove between the flexor digitorum longus and flexor hallucis longus. Be aware of, but don’t attempt to clean, the small medial calcaneal and posterior medial malleolar branches. Find the fibular artery branching from the lateral side of the posterior tibial artery near its origin to descend deep to the flexor hallucis longus muscle (Gr 5.62A & C; N506).
29. Identify the flexor digitorum longus, tibialis posterior, and flexor hallucis longus muscles. The flexor digitorum longus is the most medial of these three deep posterior crural muscles. The flexor hallucis longus is the most lateral. Only a small superior portion of the tibialis posterior is currently visible. To expose the rest of the tibialis posterior, bluntly separate the bellies of the flexor digitorum longus and flexor hallucis longus. Detach the flexor hallucis longus from its origin and reflect it distally. Clean the tibialis posterior muscle belly and follow its tendon inferiorly to where it crosses anterior (deep) to the tendon of the flexor digitorum longus.
30. Trace the tendons of the three deep flexor muscles distally until they pass posterior to the medial malleolus and deep to the flexor retinaculum. Verify the relationships of the structures passing behind the medial malleolus: from anterior to posterior are the tibialis posterior tendon, flexor digitorum longus tendon, posterior tibial artery, tibial nerve, and flexor hallucis longus tendon (Gr 5.63A-B; N517). When your hands are clean, attempt to find the posterior tibial artery pulse on yourself or a lab partner. It is easier with the foot inverted.
31. Trace the fibular artery downward through the posterior compartment (Gr 5.62A & C; N506). Look for branches that penetrate the posterior intermuscular septum to supply the lateral compartment of the leg. Find the perforating branch leaving the fibular artery anteriorly to pierce the lower part of the interosseous membrane. Confirm that the perforating branch is the same artery seen earlier during dissection of the anterior compartment. Look for a communicating branch between the fibular and posterior tibial arteries in the inferior part of the compartment. Be aware of, but don’t attempt to find, lateral calcaneal and posterior lateral malleolar branches of the fibular artery.
ANKLE JOINT
32. On a few selected cadavers, faculty will perform demonstration dissections of the ligaments of the ankle joint. Study the strong deltoid ligament on the medial side of the joint. Don't attempt to identify the individual parts of the deltoid ligament, but note its proximal attachment to the medial malleolus. On the lateral side of the ankle joint, identify the anterior talofibular, calcaneofibular, and posterior talofibular ligaments. Be aware that the anterior talofibular ligament is the most frequently sprained ligament at the ankle. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.