Anterior Mediastinum & Heart
During this period the pericardium and heart will be studied. The lower part of the thymus may overlap the upper part of the pericardium from its position in the superior mediastinum. After puberty this lymphoid organ undergoes degenerative changes (involution) and usually appears as a body of fat, although its original bi-lobed structure may still be apparent (Gr 1.58; Ne 205).
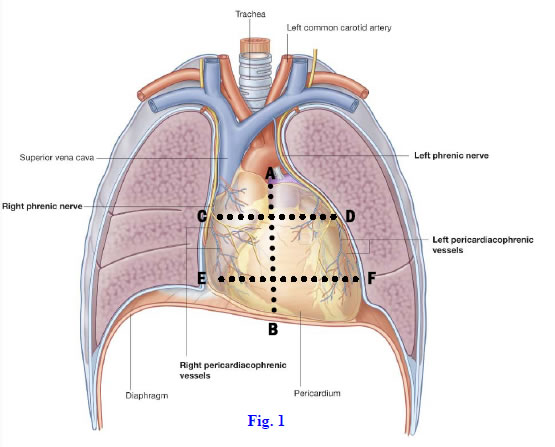
The middle mediastinum contains the pericardial sac, heart, origins of the great vessels entering and leaving the heart, phrenic nerves, and pericardiacophrenic vessels. The pericardium is a closed serous sac, which the embryonic heart invaginates in the same way that the lungs invaginate the pleurae (Gr 1.24B; Ne 205, 209, 210 [no image]). The visceral layer of serous pericardium (epicardium) covers the surface of the heart, including the fat that is usually present. The parietal layer of serous pericardium is separated from the visceral layer by a potential space, the pericardial cavity, which contains a small amount of serous fluid. The external surface of the serous parietal pericardium is covered by the tough fibrous pericardium, which is inseparable from it (Gr 1.21, 1.44, 1.46C, 1.57; Ne 205, 209).
The unyielding fibrous pericardium is the reason that a rapid accumulation of blood or other fluid within the pericardial cavity from injury (e.g., a stab wound) or disease (e.g., perforation of the weakened heart wall following myocardial infarction) can stop the heart from beating (cardiac tamponade). This can be relieved clinically if the pericardium is punctured and the fluid is drained (pericardiocentesis). The pericardium receives innervation from the phrenic nerves (C3,4,5). Therefore, pain originating in the pericardium may be “felt” by the patient in dermatomes C3,4 at the shoulder (referred pain).
Two subdivisions of the pericardial cavity arise during development due to folding of the primitive heart tube. The transverse pericardial sinus is basically the narrow space separating the ascending aorta and pulmonary trunk anteriorly from the superior vena cava posteriorly (Gr 1.43, 1.44; Ne 209). This sinus is a remnant of the passage separating the original arterial and venous ends of the embryonic heart tube and is important in cardiac surgery.
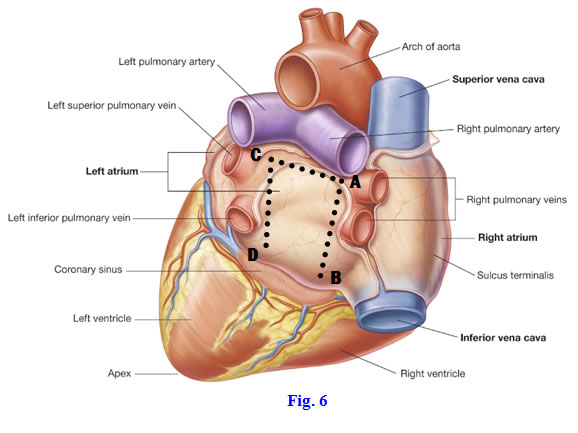
The oblique pericardial sinus is a recess behind the left atrium and is bounded by reflections of the pericardium around the four pulmonary veins and the superior and inferior vena cavae (Gr 1.44; Ne 209). At these pericardial reflections visceral serous pericardium is continuous with parietal serous pericardium. The oblique pericardial sinus is a remnant of the portion of the pericardial cavity at the original venous end of the embryonic pericardial cavity.
1. Displace the thymus superiorly if it is in the way. To open the pericardial cavity, make a vertical incision through the length of the fibrous pericardium (Fig. 8-1, A-B). Now make transverse incisions laterally from the superior and inferior ends of the vertical incision and reflect the flaps of pericardium laterally (Fig. 8-1, C-D, C-E).
2. Examine the pericardial cavity. Identify two subdivisions of the pericardial cavity, the transverse and oblique pericardial sinuses. Insert your index finger into the transverse pericardial sinus, which is located between the ascending aorta and pulmonary trunk anteriorly and the superior vena cava posteriorly. Place your hand into the oblique pericardial sinus behind the heart and explore its extent.
OVERVIEW AND REMOVAL OF THE HEART
3. ![]() Now carefully remove the heart by cutting the great vessels that enter and leave the heart. Cut the ascending aortaand pulmonary trunk about 2.5 cm above where they leave the left and right ventricles, respectively. Next cut the superior and inferior venae cavae close to the heart without damaging the right atrium. Put gentle traction on the heart and cut the four pulmonary veins just before they enter the left atrium. Finally cut the reflections of serous pericardium between the transverse and oblique pericardial sinuses and remove the heart. XXX
Now carefully remove the heart by cutting the great vessels that enter and leave the heart. Cut the ascending aortaand pulmonary trunk about 2.5 cm above where they leave the left and right ventricles, respectively. Next cut the superior and inferior venae cavae close to the heart without damaging the right atrium. Put gentle traction on the heart and cut the four pulmonary veins just before they enter the left atrium. Finally cut the reflections of serous pericardium between the transverse and oblique pericardial sinuses and remove the heart. XXX
The heart is the muscular pump that propels blood through the circulatory system by its rhythmic contractions. It consists of four chambers. Following blood as it flows through the heart, in sequence, it flows through the right atrium, right ventricle, left atrium, and left ventricle.
Venous blood enters the right atrium from the superior and inferior venae cavae, passes through the tricuspid (right atrioventricular) valve into the right ventricle, and is pumped into the pulmonary trunk for transport to the lungs (pulmonary circulation). Oxygenated blood returns from the lungs to the left atrium through the pulmonary veins and passes through the mitral (bicuspid) valve into the left ventricle. Contraction of the left ventricle pumps the blood into the aorta for distribution to the rest of the body (systemic circulation).
To achieve this pattern of blood flow, the two atria contract together followed by the two ventricles contracting together, with the ventricles contracting in sequence from the apex toward the base of the heart to more efficiently expel blood. Most of the blood flow from the atria into the ventricles is passive, but contraction of the atria accounts for the final 25%. The walls of the ventricles relax to allow for maximal filling of blood. When the ventricles contract, the tricuspid and mitral valves close, forcing blood to exit the heart through the pulmonary trunk and aorta. While the ventricles contract, the walls of the atria relax and the atria fill with venous blood. (Note: while blood entering the right atrium is deoxygenated blood from the periphery, blood entering the left atrium is highly oxygenated blood from the lungs.)
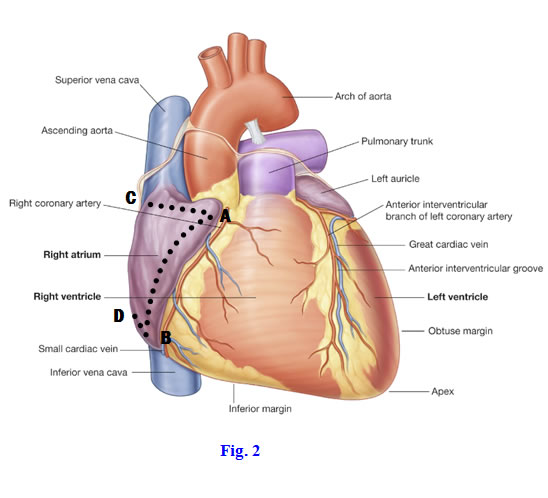
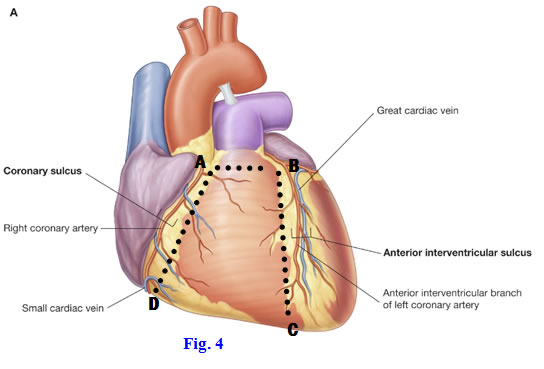
On the surface of the heart the separation of the atria from the ventricles is marked by the coronary (atrioventricular) sulcus, and the separation of the right and left ventricles is indicated by anterior and posterior interventricular sulci. The sulci are usually obscured by fat.
The base of the heart is the proximal end formed mainly by the left atrium, where the pulmonary veins enter, but with a small contribution from the right atrium, where the venae cavae enter. The base is located posteriorly in the body.
The blunt apex is formed by the inferolateral extremity of the left ventricle, which lies in the left fifth intercostal space 8-9 cm from the median plane. Thus, the apex of the typical heart is directed to the left and is the most inferior part of the heart.
The sternocostal (anterior) surface is formed mainly by the right ventricle, with smaller contributions from the right atrium and left ventricle. This is the part of the heart most likely to be injured in blunt trauma or a penetrating wound to the anterior chest wall.
The diaphragmatic surface is formed mainly by the left ventricle with a contribution from the right ventricle. This is the surface that rests on the diaphragm.
The slightly convex right margin of the heart is formed by the right atrium and is continuous superiorly and inferiorly, respectively, with the superior vena cava and inferior vena cava. It can be seen and examined in posteroanterior (PA) chest radiographs (Gr 1.23, 1.43; Ne 207). The right margin is responsible for the cardiac impression on the mediastinal surface of the embalmed right lung.
The left (obtuse) margin is formed mainly by the left ventricle with a small superior contribution from the left auricle. The left margin is responsible for the cardiac notch and deep cardiac impression on the embalmed left lung. In a PA chest x-ray, the arch of the aorta and pulmonary trunk are apparent above the left auricle and left ventricle (Gr 1.23; Ne 207).
The relatively sharp inferior (acute) border of the heart, which is obscured by the liver on an x-ray, is the junction of the sternocostal and diaphragmatic surfaces.
The tissues of the heart are supplied by right and left coronary arteries, which are embedded in a variable amount of fat on the heart’s surface. The right coronary artery branches from the right aortic sinus of the ascending aorta (Gr 1.55 A, B; Ne 211, 212) to enter the coronary sulcusbetween the right atrium and right ventricle (Gr 1.41A, 1.43, 1.45A; Ne 211, 212). Near its origin the right coronary artery gives off the small, but important, sinuatrial nodal artery (Gr 1.45; Ne 212). This artery supplies the sinuatrial (SA) node, the “pacemaker” of the heart (Gr 1.56; Ne 219). Near the inferior border of the heart, the right coronary gives off the right marginal artery, which passes to the left along the inferior border.
The right coronary artery continues in the coronary sulcus onto the posterior aspect of the heart and to the posterior interventricular sulcus, where it usually supplies the posterior interventricular artery (Gr 1.44A, 1.45B; Ne 208, 211, 212). The posterior interventricular artery may be referred to clinically as the “posterior descending artery.” Just proximal to the posterior interventricular sulcus, the right coronary usually gives off the small atrioventricular nodal artery, which supplies the atrioventricular (AV) node of the heart’s conduction system (Gr 1.56; Ne 219). The AV node is the part of the heart’s conduction system that sends impulses through the atrioventricular (AV) bundle in the interventricular septum to coordinate the contractions of the ventricles. The AV bundle bridges the fibrous skeleton of the heart, dense collagenous rings (anuli fibrosi) that both anchor valve cusps (e.g., of the tricuspid valve) and electrically insulate the atria from the ventricles. The conduction system of the heart is discussed in more detail later.
The left coronary artery branches from the left aortic sinus of the ascending aorta and courses to the left between the pulmonary trunk and left auricle (Gr 1.45, 1.48A; Ne 211, 213). As it enters the coronary sulcus the left coronary artery divides into anterior interventricular and circumflex branches. The anterior interventricular artery (clinically termed the “left anterior descending [LAD] artery”) descends in the anterior interventricular sulcus to the apex of the heart, where it typically turns around the inferior border and anastomoses with the posterior interventricular artery. As it descends, the anterior interventricular artery usually gives off a lateral diagonal branch to the anterior wall of the left ventricle (Gr 1.45A; Ne 211, 213)). The anterior interventricular artery supplies the anterior 2/3 of the interventricular septum, which contains the atrioventricular (AV) bundle.
The circumflex branch of the left coronary artery follows the coronary sulcus around the left margin of the heart (Gr 1.45; Ne 211, 213). Its left marginal branch descends along the left (obtuse) margin of the heart. The circumflex branch continues onto the posterior surface of the heart, giving off a posterior artery of the left ventricle before terminating, usually in the coronary sulcus short of its junction with the posterior interventricular sulcus.
4. Reposition the heart in its normal orientation (Gr 1.42, 1.43; Ne 206) and identify its surfaces and borders.
5. Begin the dissection of the heart by identifying and cleaning the coronary arteries and their branches. Clean the right coronary artery. Find the small sinuatrial nodal artery branching near its origin from the right aortic sinus. Dissect the right marginal artery near the inferior border of the heart. Turn the heart over and follow the right coronary artery until it turns downward into the posterior interventricular sulcus as the posterior interventricular(posterior descending) artery. The posterior interventricular artery supplies the posterior 1/3 of the interventricular septum, which separates the right and left ventricles. Just proximal to where the right coronary artery turns downward as the posterior interventricular artery, look for the small atrioventricular nodal arteryto the atrioventricular (AV) node. The AV nodal arterypierces the lower part of the interatrial septum.
6. Clean the left coronary artery and its branches. The left coronary artery branches from the left aortic sinus and passes between the left auricle and the pulmonary trunk (Gr 1.45, 1.48A; Ne 211, 213)). It then divides into anterior interventricular and circumflex branches. The anterior interventricular(left anterior descending [LAD]) artery descends in the anterior part of the interventricular sulcus (Gr 1.41, 1.43, 1.45; Ne 206, 211, 213)). It supplies the anterior 2/3 of the interventricular septum, which contains the AV bundle. The circumflex branch of the left coronary artery passes to the posterior aspect of the heart in the coronary sulcus. The circumflex branch gives off the left marginal branch, which descends along the left border of the heart, and usually gives off a posterior artery of the left ventricle on the back of the heart. XXX
A heart is said to be right dominant if the posterior interventricular artery is a branch of the right coronary artery. This occurs in about 2/3 of all hearts. The heart is left dominant in the minority of individuals in whom the posterior interventricular artery arises from the circumflex branch of the left coronary artery. If both the right and left coronary arteries send branches into or parallel to the posterior interventricular sulcus, the heart is said to be codominant (balanced). The branches of coronary arteries are said to be functional end arteries, which usually lack sufficient anastomoses to maintain tissue viability if occlusion should occur.
Most of the larger cardiac veins accompany branches of the coronary arteries (Gr 1.41, 1.43, 1.44A; Ne 211). The coronary sinus receives the larger cardiac veins as tributaries and is responsible for draining most of the venous blood from tissues of the heart into the right atrium.
The great cardiac vein ascends beside the anterior interventricular artery and becomes the coronary sinus when it reaches the posterior part of the coronary sulcus (Gr 1.46; Ne 211). The small cardiac vein accompanies the right marginal artery to enter the coronary sulcus and follows it onto the posterior surface of the heart to become a tributary of the coronary sinus. An occasional variation is that the small cardiac vein crosses the coronary sulcus to drain directly through the anterior wall of the right atrium. Small anterior cardiac veins also pass directly from the anterior wall of the right ventricle across the coronary sulcus into the right atrium. The middle cardiac vein ascends beside the posterior interventricular artery to reach the coronary sinus.
The small oblique vein of the left atrium descends along the posterior wall of the left atrium to enter the coronary sinus.
Finally, the smallest cardiac veins (venae cordis minimae, Thebesian veins) drain directly from myocardium into chambers of the heart and cannot be demonstrated by dissection (Gr 1.46C).
CHAMBERS OF THE HEART
7. Identify and clean the coronary sinus, great cardiac vein, small cardiac vein, and middle cardiac vein. Try to identify and clean the small anterior cardiac veins and the oblique vein of the left atrium.
INTERNAL FEATURES OF THE CHAMBERS OF THE HEART
8. The heart will now be opened and the major features of each chamber studied, starting with the right atrium. Note the right auricle, a small “ear-like” appendage of the right atrium that overlies part of the ascending aorta.
9. Again, find the coronary sulcus. Make a downward incision through the anterior wall of the right atrium parallel to and about 0.5-1 cm to the right of the coronary sulcus (Fig. 8-2, A-B, Gr 1.49). From each end of this cut, make a transverse incision to the right border of the heart ending next to the superior vena cava superiorly and the inferior vena cava inferiorly (Fig. 8-1, A-C, B-D). Reflect the atrial flap toward the right margin of the heart (Fig. 8-3).
10. To remove clotted blood from the right atrium, first extract as much of it as possible using forceps. Next, put the heart on a tray and take it to the tissue wash sink. Wash out the chamber using running water while the tissue disposer is operating. XXX
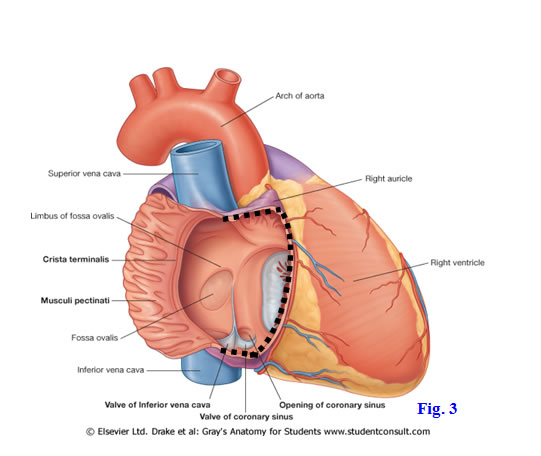
The internal surface of the right atrium is divided into an anterior rough-walled portion and a posterior smooth-walled portion by a vertical ridge of muscle, the crista terminalis (Gr 1.49; Ne 214). The small muscular ridges in the anterior portion of the wall are the pectinate muscles. This rough-walled part of the atrium is a remnant of the original embryonic atrium. The smooth-walled portion of the atrium is the sinus venarum, which developed from the embryo’s right horn of the sinus venosus.
The orifice of the superior vena cava is directed downward and forward toward the right atrioventricular (tricuspid) valve. The orifice of the inferior vena cava has a small semilunar endocardial fold, the valve of the inferior vena cava, which directs blood flow toward the interatrial septum. In the fetus, the interatrial septum was the site of the foramen ovale. Its location is marked after birth by a shallow oval depression, the fossa ovalis. During prenatal life the foramen ovale allowed most of the oxygenated blood returning from the umbilical vein through the inferior vena cava to be shunted into the left atrium, bypassing the pulmonary circulation of the nonfunctional lungs. In 25% of the population, a small opening just sufficient to admit a probe remains after birth (probe patency of the foramen ovale). The prominent margin of the fossa ovalis is the limbus fossa ovalis.
The opening of the coronary sinus is located between the valve of the inferior vena cava and the right atrioventricular orifice. The opening is guarded by the small valve of the coronary sinus. Near the opening of the coronary sinus, between it and the septal cusp of the tricuspid valve, look for a small, lighter colored area of the interatrial wall that is sometimes apparent. This is the location of the AV node (Gr 1.56; Ne 219).
11. Examine the interior of the right atrium. Find the crista terminalis separating the rough-walled anterior portion of the chamber from the smooth-walled sinus venarum. The muscular ridges of the anterior part are the pectinate muscles. Note the superior and inferior venae cavae opening into the sinus venarum. Identify the opening of the coronary sinus between the valve of the inferior vena cava and the right atrioventricular orifice. Find a shallow oval depression on the interatrial septum, the fossa ovalis. It is a remnant of the fetal opening between the two atria, the foramen ovale. Note the prominent margin of the fossa ovalis, the limbus fossa ovalis. Does this heart have a small remnant of the foramen ovale large enough to pass a probe, a probe patency of the foramen ovale?
12. Next cut open the right ventricle as follows: Insert two fingers into the pulmonary trunk to find where the pulmonary valve cusps are located. Make a short transverse incision in the anterior wall of the right ventricle parallel to and just below the pulmonary valve cusps (Fig. 8-4, A-B). From the left end of the first incision make a downward cut parallel to, and 1.5 cm to the right of, the anterior interventricular sulcus (and the anterior interventricular artery that it contains) and continuing downward to the inferior border of the heart (Fig. 8-4, B-C; Gr 1.50; Ne 214). From the right end of the first incision make a downward incision parallel to, and 1 cm to the left of, the coronary sulcus to the inferior border of the heart (Fig. 8-4, A-D). Reflect the anterior wall of the right ventricle downward (the wall has been removed in Fig. 8-5) and take out any clotted blood. XXX
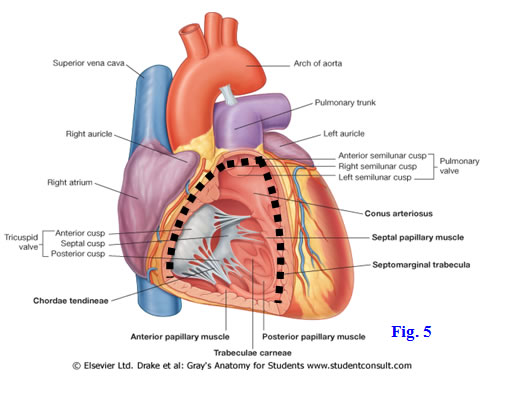
The right ventricle forms most of the sternocostal surface of the heart. Superiorly it tapers into a funnel-shaped outflow tract, the conus arteriosus or infundibulum, which opens into the pulmonary trunk (Gr 1.50; Ne 214). The conus arteriosus has smooth walls and is separated from the main ventricular cavity by a thick muscular ridge, the supraventricular crest. The internal surface of the rest of the ventricle exhibits irregular muscular ridges, the trabeculae carneae. Fingerlike projections of muscle from the ventricular wall, the papillary muscles, are attached to cusps of the tricuspid valve by slender fibrous strands, the chordeae tendineae. Typically the right ventricle contains anterior, posterior, and septal papillary muscles, but these may be replaced by multiple smaller ones in some hearts. Each cusp of the tricuspid (right atrioventricular) valve is attached by chordae tendineae to two papillary muscles (Ne 217). For example, the posterior cusp receives chordeae tendineae from the anterior and posterior papillary muscles. Tension on the chordae tendinae by contraction of the papillary muscles prevents the valve cusps from being pushed back into the right atrium with a regurgitation of blood when the ventricle contracts.
The septomarginal trabecula (moderator band) is a band of muscle that bridges the lower part of the right ventricular chamber from the interventricular septum to the base of the anterior papillary muscle (Gr 1.50, 1.56; Ne 214, 219). The septomarginal trabecula is significant because it carries fibers of the right branch of the atrioventricular bundle (right bundle branch), part of the heart’s conduction system.
The interventricular septum separating the right and left ventricles bulges into the cavity of the right ventricle because of the higher pressure in the left ventricle; therefore, the cavity of the right ventricle is crescent-shaped in cross-section. A small upper part of the interventricular septum consists of a thin membranous part, while the majority of the septum is the thick muscular part (Gr 1.52A; Ne 210 [no image], 218). After traversing the fibrous skeleton of the heart, the AV bundle descends along the margin of the membranous interventricular septum. The AV bundle divides into right and left bundle branches at the junction of the muscular and membranous parts and each descends along its respective side of the muscular interventricular septum. (Gr 1.56; Ne 219).13. Notice the smooth, funnel-shaped outflow tract of the right ventricle just below the pulmonary valve cusps (Gr 1.50; Ne 214). This is the conus arteriosus, or infundibulum. The rest of the ventricular wall is covered by prominent crisscrossing muscular ridges, the trabeculae carneae. The valve cusps of the tricuspid valve are attached to conical projections of muscle from the ventricular wall, the three papillary muscles, by slender chordae tendinae. The papillary muscles are designated as anterior, posterior, and septal, although there may be multiple smaller papillary muscles instead of three larger ones. The anterior, posterior, and septal cusps of the tricuspid valve each receives chordae tendinae from two of the papillary muscles (e.g., the anterior cusp from septal and anterior papillary muscles).
14. Look for a bundle of muscle extending from the lower part of the interventricular septum to the base of the anterior papillary muscle. This septomarginal trabecula (moderator band) contains part of the right branch of the atrioventricular bundle, which regulates contraction of the right ventricle. XXX
The left atrium forms most of the base of the heart. It receives two right pulmonary veins and two left pulmonary veins returning oxygenated blood from the right and left lungs, respectively. The wall of the left atrium is smooth except in the vaguely ear-shaped left auricle, which is a remnant of the embryonic primitive atrium and contains pectinate muscles (Gr 1.51A; Ne 215). Remember that the left auricle forms the part of the left margin of the cardiovascular shadow between the pulmonary trunk and the left ventricle on a PA chest radiograph (Gr 1.23; Ne 207). The interatrial septum features a shallow semilunar depression that indicates the location of the foramen ovale of the embryo.
15. Turn your attention to the left atrium. Two right pulmonary veins and two left pulmonary veins return oxygenated blood from the lungs to the left atrium. Open the left atrium by making parallel vertical incisions through the thin wall of the atrium just medial to the entrances of the right and left pulmonary veins (Fig. 8-6, A-B and C-D). Make a third, transverse incision connecting the superior end of the other two incisions (Fig. 8-6, A-C) and turn the flap downward. After removing clotted blood, observe the smooth wall of the atrium (Gr 1.51; Ne 215). Only the small ear-like appendage of the atrium, the left auricle, and perhaps a small area surrounding its opening, are ridged with pectinate muscles. On the interatrial septum look for a shallow semilunar depression that corresponds to the fossa ovalis in the right atrium. XXX
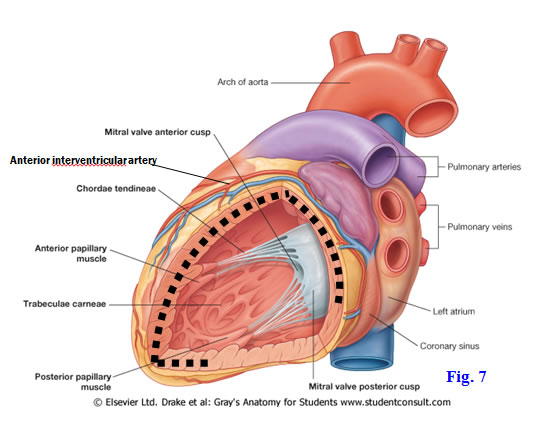
The left ventricle forms the apex of the heart and most of its left (obtuse) margin. The left ventricle must pump harder to overcome resistance in the systemic circulation than the right ventricle does to overcome resistance in the pulmonary circulation and, therefore, has walls two to three times as thick as the right ventricle’s (Gr 1.52; Ne 215, 218). Superiorly its chamber tapers into a smooth-walled outflow tract into the ascending aorta, the aortic vestibule, just below the three cusps of the semilunar aortic valve. As in the right ventricle, the internal surface of the rest of the wall is covered by irregular muscular ridges, the trabeculae carneae. The left ventricle has only two papillary muscles—anterior and posterior—attached by chordae tendineae to cusps of the left atrioventricular (mitral, bicuspid) valve. The mitral valve has only two cusps, anterior and posterior, and each valve cusp receives chordae tendineae from both papillary muscles (Gr 1.55D; Ne 215, 217).
16. Before opening the left ventricle, insert two fingers into the ascending aorta to determine the level of the aortic valve cusps. Make a downward incision parallel to, and 1.5 cm to the left of, the anterior interventricular sulcus and continuing around the apex of the heart 2 cm up the posterior wall of the left ventricle. Make a second transverse incision from the top of the first incision around the left border of the heart parallel and inferior to the coronary sulcus, ending near the middle of the posterior wall of the left ventricle. Reflect the ventricular wall flap to the left (Fig. 8-7). Remove the clotted blood. The wall of the left ventricle is normally two to three times as thick as that of the right ventricle. Verify this.
17. The smooth-walled outflow tract of the left ventricle just below the cusps of the aortic valve is the aortic vestibule (Gr 1.52; Ne 215). The remainder of the internal surface of the left ventricle is covered by trabeculae carneae. Note that from this view the interventricular septum lies not only to the right of, but also anterior to, most of the left ventricle. The muscular part of the interventricular septum normally bulges toward the right because of the higher pressure in the left ventricle. A smaller upper, posterior part is the membranous interventricular septum, which is the usual location of congenital ventricular septal defects when they are present.
18. Identify the two papillary muscles attached by chordae tendinae to the anterior and posterior cusps of the mitral (bicuspid, left atrioventricular) valve, which controls blood flow between the left atrium and ventricle. Look for thin strands of endocardium bridging the lowest part of the chamber of the left ventricle from the interventricular septum toward the apex. When present, these false chordae tendinae enclose individual strands of the left bundle branch, the part of the heart’s conduction system that regulates contraction of the left ventricle. XXX
The conduction system of the heart controls its inherent rhythmic contractions. The conduction system is difficult to demonstrate in dissection but is extremely important to understand. It consists of specialized cardiac muscle cells arranged as two nodes for initiating electrochemical impulses (action potentials) and as pathways that conduct the impulses to other areas of the heart (Gr 1.56; Ne 219).
The sinuatrial (SA) node lies in the upper part of the crista terminalis, near the superior vena cava. The SA node is the “pacemaker” of the heart but is itself influenced by the autonomic nervous system—sympathetic stimulation increases the rate and force of contractions, whereas parasympathetic stimulation decreases the rate and force of contractions. Internodal atrial pathways conduct impulses originating in the SA node to the atrioventricular (AV) node, which is located in the interatrial septum near the opening of the coronary sinus. The AV node sends impulses through the atrioventricular (AV) bundle (of His) to the distal portion of the ventricles. The ventricles are electrically insulated from the atria by the fibrous skeleton of the heart, which surrounds and gives attachment to the atrioventricular valves (Ne 216). The AV bundle divides into right and left bundle branches to their respective ventricles at the junction of the membranous and muscular parts of the interventricular septum. Specialized subendocardial fascicles of the AV bundle are known as Purkinje fibers. Part of the right bundle branch traverses the septomarginal trabecula (moderator band) to reach the anterior papillary muscle.
The blood supply of the heart’s conduction system is clinically important. Typically the SA node is supplied by the SA nodal artery, which can be a direct branch of the right coronary artery or may arise from a right atrial branch of the right coronary. The AV node is supplied by the AV nodal artery, which also usually branches from the right coronary artery. Note that as variations the SA nodal artery and/or AV nodal artery may arise from the left coronary artery. Most of the AV bundle and the bundle branches are located in the anterior 2/3 of the interventricular septum, which is supplied by theanterior interventricular(left anterior descending) arteryoff the left coronary artery. Coronary artery disease that compromises blood flow in the AV nodal artery results in heart block, with the ventricles contracting at their own rate independently of the atria. Occlusion of the blood supply to one AV bundle branch results in bundle branch block. In this condition the unaffected ventricle contracts normally, but the denervated ventricle contracts slightly later, asynchronously, when the impulse spreads to it from the normal ventricle by myogenic conduction.
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.