Posterior Mediastinum
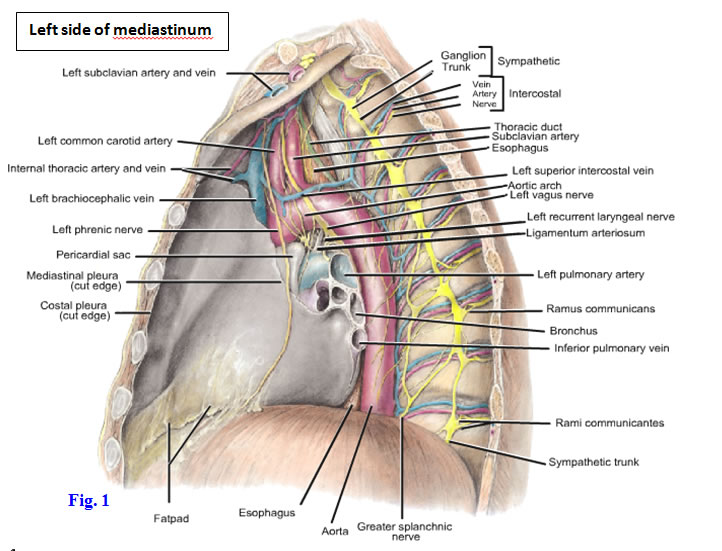
The mediastinum is the central partition of tissue in the thoracic cavity separating the lungs and their enclosing pleurae in the right and left pulmonary cavities (Fig. 1; Gr 1.25; Ne 210 [no image]). The mediastinum consists both of organs intrinsic to the thorax (e.g., the heart) and structures that traverse the thorax between other body regions (e.g., the esophagus and thoracic duct). It is subdivided into the superior mediastinum and inferior mediastinum by a horizontal plane connecting the sternal angle with the intervertebral disc joining vertebrae Tv4/Tv5. The inferior mediastinum is further subdivided with reference to the heart and pericardium. The heart and its enclosing pericardium comprise the middle mediastinum. The anterior mediastinum lies between the pericardium and the sternum, and the posterior mediastinum is posterior to the pericardium and the downwardly sloping posterior portion of the diaphragm, in front of thoracic vertebrae Tv5-Tv12. During this period we will be studying structures of the posterior mediastinum and the superior mediastinum.
1. Be careful to preserve the phrenic nerves during the following dissection. Note again that they pass anterior to the roots of the lungs. In order to gain access to the posterior mediastinum, it is necessary to carefully remove the posterior part of the pericardial sac (Gr 1.57; Ne 209). To preserve the esophageal plexus of nerves while removing the pericardial sac, first clean the right and left vagus nerves where they pass posterior to the roots of the lungs (Gr 1.57, 1.72, 1.75; Ne 203, 224, 225, 226). Follow each vagus nerve distally and clean the branches it contributes to the esophageal plexus, removing the pericardium piecemeal as you do so. Observe that the esophagus lies directly posterior to the left atrium, the pathological enlargement of which can be demonstrated on a chest x-ray by having the patient swallow barium. Carefully clean and preserve the esophageal plexus of nerves on the surface of the esophagus.
2. Before leaving the esophagus, identify short esophageal arteries that branch from the descending thoracic aorta to enter the middle third of the esophagus (Gr 1.57, 1.70; Ne 231). Although it is not apparent at this time, the cervical third of the esophagus is supplied by the inferior thyroid artery and the lower third is supplied mainly by the left gastric artery. XXX
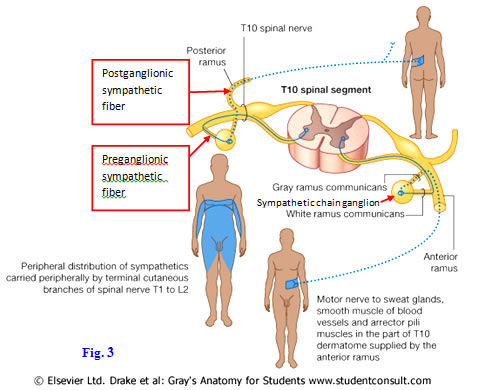
The azygos system of veins receives blood from the posterior thoracic wall via posterior intercostal veins and from the posterior abdominal wall via ascending lumbar veins (Gr 1.73, 1.74, 1.75; Ne 186 [no image], 224, 232). The vertically oriented azygos vein is formed by the union of the right ascending lumbar vein and the right subcostal vein, which is located below the 12th rib. The azygos ascends along the right side of thoracic vertebral bodies, receiving multiple tributaries, including the lower 7 right posterior intercostal veins and right superior intercostal vein. The right superior intercostal vein is formed by the union of the 2nd, 3rd, and 4th posterior intercostal veins. The azygos vein terminates as the arch of the azygos vein, which passes above the root of the right lung to empty into the superior vena cava (Gr 1.75; Ne 224).
On the left side, the left ascending lumbar vein and left subcostal vein unite to form the vertically oriented hemiazygos vein (Gr 1.73, 1.74; Ne 186 [no image], 232), which ascends along the left side of thoracic vertebral bodies. The hemiazygos vein receives left posterior intercostal veins 9-11 as tributaries before turning to the right and crossing over the vertebral column at approximately Tv9 to drain into the azygos vein.
Superior to the hemiazygos vein and in line with it may be an accessory hemiazygos vein, which receives left posterior intercostal veins 5-8 (Gr 1.73, 1.74; Ne 186 [no image], 225, 232). The lower end of the accessory hemiazygos may cross to the right side to enter the azygos vein or may empty into the hemiazygos vein. The left superior intercostal vein drains the posterior portion of intercostal spaces 2-4 into the left brachiocephalic vein but may communicate with the accessory hemiazygos vein (Fig. 1).
On both the right and left sides of the body the first intercostal space is drained by a supreme intercostal vein into its respective brachiocephalic vein.
Expect to find variations. For example, the azygos vein may be a large median vein receiving posterior intercostal veins from both sides, and the hemiazygos and/or accessory hemiazygos veins may be absent. Although the connections are difficult to demonstrate, it is important to be aware that the azygos system communicates with the vertebral venous plexus, providing a pathway for the metastasis of cancer cells and the spread of infection from the thorax to the vertebral column, spinal cord, and brain(Gr 4.26, 4.44; Ne 166). The connections of the azygos system are also one alternative route of venous return to the heart from the lower bodyif the inferior vena cava becomes obstructed (e.g., by a tumor) (Gr 1.74; Ne 232).3. Retract the esophagus to the left and expose the azygos vein. Identify its right posterior intercostal and superior intercostal tributaries. Clean the arch of the azygos vein as it crosses above the root of the right lung to end in the superior vena cava. Now attempt to displace the descending thoracic aorta medially (to the right) just enough to find the hemiazygos and accessory hemiazygos veins, if present. This may be difficult.
THORACIC DUCT
4. Carefully probe through the tissue posterior to the esophagus, between the azygos and hemiazygos veins, to find the delicate thoracic duct ascending in the midline (Fig. 2, Gr 1.71, 1.74, 1.77; Ne 200, 210 [no image], 295). At about the Tv5 level it inclines toward the left, but this may be difficult to see. The thoracic duct is usually whitish in color but may contain dried blood and appear blue. Although it is the largest lymphatic channel in the body, the thoracic duct has the diameter of a small vein (3-5 mm). It may have a scalloped outline. XXX
The thoracic duct drains lymph from the entire body below the diaphragm and from the left half of the body above the diaphragm. Thus, it usually receives the lymphatic channels from the left upper extremity (left subclavian lymphatic trunk), left half of the head and neck (left jugular lymphatic trunk), and left lung (left bronchomediastinal lymphatic trunk) before draining into the junction of the left subclavian and internal jugular veins, which is known as the left venous angle (Gr 1.38, 1.71; Ne 202, 259, 295).
The thoracic aorta consists of the ascending aorta leaving the left ventricle in the middle mediastinum, the arch of the aorta in the superior mediastinum, and the descending thoracic aorta in the posterior mediastinum (Fig. 1; Gr 1.43, 1.64; Ne 206, 209, 226, 231). The descending thoracic aorta has visceral and parietal branches. Visceral branches include the esophageal arteries and the bronchial arteries. Parietal branches include the nine lower pairs of posterior intercostal arteries, the subcostal arteries (below the 12th ribs), and the superior phrenic arteries to the diaphragm (Gr 1.57, 1.63, 1.70; Ne 201, 231).
5. Find representative examples of the visceral and parietal branches of the descending thoracic aorta. Now pull the esophagus aside to see the descending thoracic aorta traversing the aortic hiatus of the diaphragm anterior to the body of the 12th thoracic vertebra (Gr 1.69, 1.77, 2.74; Ne 225, 227, 231). XXX
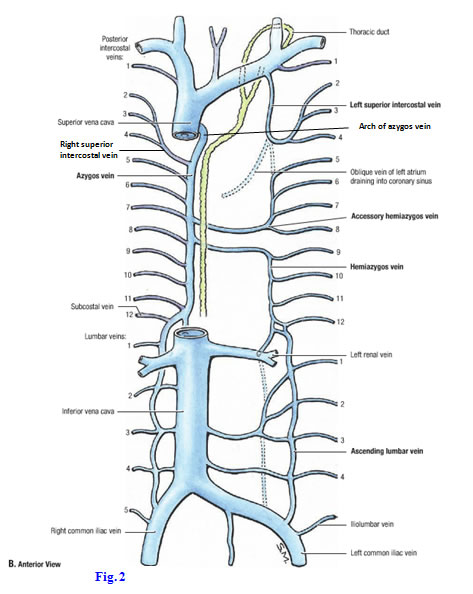
The right and left sympathetic trunks (sympathetic chains) descend from anterior to the necks of the upper ribs anteromedially to lie along the lateral surfaces of lower thoracic vertebral bodies (Gr 1.72, 1.75, 1.76; Ne 203, 224, 225). The thoracic portion of each sympathetic trunk typically features 11-12 swellings, the sympathetic chain (paravertebral) ganglia. Each ganglion is a collection of nerve cell bodies of postganglionic sympathetic neurons, where the axons of preganglionic sympathetic neurons synapse (Fig. 3).
Like the subcostal and first two lumbar chain ganglia, thoracic sympathetic chain ganglia T1-11 are connected to the anterior rami of spinal nerves by both white and gray rami communicantes (Figs. 1, 3). In other words, sympathetic chain ganglia T1-L2 have both white and gray communicating rami, but the sympathetic chain ganglia above and below these levels have only gray communicating rami.
The white ramus communicans carries preganglionic sympathetic fibers (Fig. 3) and general visceral afferent nerve fibers. The preganglionic sympathetic fibers are traveling from the spinal nerve to the sympathetic ganglion, and the general visceral afferent fibers are going the opposite direction, from the sympathetic ganglion to the spinal nerve. (Remember that the cell bodies of the general visceral afferent nerve fibers are located either in posterior root ganglia or in cranial nerve ganglia.) A gray ramus communicans carries postganglionic sympathetic fibers from the ganglion to the spinal nerve for distribution with its anterior and posterior primary rami. Gray rami communicantes do not carry afferent fibers. The white and gray rami communicantes are grossly indistinguishable, but the white ramus communicans usually is located lateral to the gray.
Other visceral nerve branches emerge ventrally from the lower thoracic sympathetic ganglia en route to prevertebral ganglia located in the abdomen. There are three of these thoracic splanchnic nerves on each side in the thorax —greater, lesser, and least. The greater thoracic splanchnic nerve usually receives contributions from the 5th to 9th thoracic chain ganglia (Fig. 1; Gr 1.72, 1.75-1.77; Ne 160, 203, 224, 225, 234). The lesser thoracic splanchnic nerve is formed from the 10th and 11th ganglia. The least thoracic splanchnic nerve comes from the 12th thoracic ganglion. The thoracic splanchnic nerves supply sympathetic innervation for most of the abdominal viscera.6. Clean the thoracic sympathetic trunks. Find examples of sympathetic chain ganglia and the rami communicantes that connect them to intercostal nerves.
7. Clean the greater thoracic splanchnic nerves as they descend toward the diaphragm. The lesser and least splanchnic nerves are difficult to demonstrate; be aware of their functions but don’t spend time searching for them. XXX
The superior mediastinum is located between the manubrium of the sternum anteriorly and the bodies of vertebrae Tv1-Tv4 posteriorly. It extends from the superior thoracic aperture above to a transverse plane connecting the sternal angle with the intervertebral disc joining vertebrae Tv4/Tv5 below. Contents of the superior mediastinum include the remnants of the thymus; right and left brachiocephalic veins and superior vena cava; arch of the aorta and its three branches; vagus, phrenic, and left recurrent laryngeal nerves; trachea and its division into right and left primary bronchi; esophagus; and thoracic duct.
The thymus is a bi-lobed lymphoid organ that begins to undergo fatty degeneration (involution) at puberty (Gr 1.58; Ne 205). In the adult it is represented by a mass of fatty tissue, although it is still functional.
Each brachiocephalic (innominate) vein is formed posterior to the sternoclavicular joint by the union of the subclavian vein and internal jugular vein of its side (Fig. 2; Gr 1.42, 8.5, 8.16E-F; Ne 200, 205, 206). The left brachiocephalic vein crosses to the right side, and the right and left brachiocephalic veins join posterior to the first right costal cartilage to form the superior vena cava. The superior vena cava returns to the right atrium all of the venous blood from structures superior to the diaphragm except that from the lungs and the tissues of the heart itself.8. Carefully remove the remnants of the thymus. Identify the vertically oriented right brachiocephalic vein. Note that the left brachiocephalic vein descends across the superior mediastinum from left to right. The right and left brachiocephalic veins join to form the superior vena cava.
9. Clean the brachiocephalic veins and the remaining portion of the superior vena cava. Look for tributaries of the brachiocephalic veins. Each typically receives an internal thoracic vein and a supreme (first posterior) intercostal vein (Gr 1.74, 1.76; Ne 184, 186 [no image]). The left brachiocephalic vein also receives the left superior intercostal vein draining left intercostal spaces 2-4 and one or more inferior thyroid veins (Gr 8.16 E-F; Ne 74, 225, 232). Identify the entrance of the arch of the azygos vein into the superior vena cava.
10. While performing these dissections, please remain within the thorax and do not to dissect into the neck. The neck will be dissected during the second semester. XXX
Turn your attention to the arch of the aorta (aortic arch).
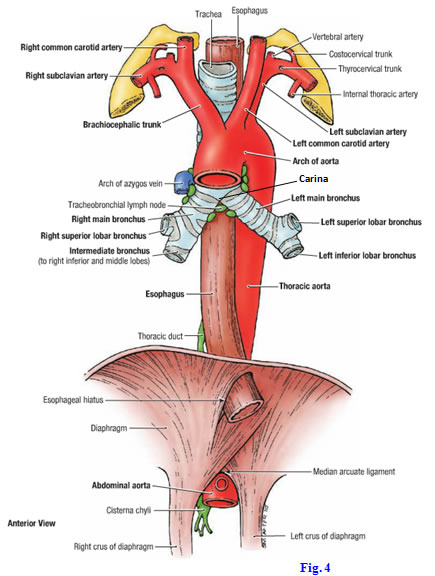
The arch of the aorta passes posterolaterally to the left from the ascending aorta to become continuous with the descending thoracic aorta (Fig. 1; Gr 1.76, 1.80B; Ne 225-227, 231). The first and largest branch of the arch of the aorta is the brachiocephalic trunk (brachiocephalic artery) (Gr 1.64, 1.69, 1.77; Ne 187, 226, 231). It ascends toward the right to divide into the right common carotid artery and right subclavian artery behind the right sternoclavicular joint.
The second branch of the arch of the aorta, located to the left of the brachiocephalic trunk, is the left common carotid artery (Fig. 1; Gr 1.69, 1.76, 1.77; Ne 187, 226, 231). It ascends into the neck.
The third branch is the left subclavian artery, whichalso ascends into the root of the neck (Fig. 1). It passes above the first rib between the anterior and middle scalene muscles to enter the axilla, where it was seen in an earlier dissection.
Variations in the branching pattern from the arch of the aorta may occur, including one or more additional arteries arising from the arch of the aorta (Gr 1.65, 8.16D). These include a thyroid ima artery and a left vertebral artery.
11. It may be necessary to reflect the superior vena cava and left brachiocephalic vein upward to expose the branches arising from the aortic arch. Clean the arch of the aorta and its three large branches, the brachiocephalic trunk, left common carotid artery, and left subclavian artery (Fig. 4).
NERVES OF THE SUPERIOR MEDIASTINUM
12. Find the left vagus nerve descending between the left common carotid and left subclavian arteries to cross the left side of the arch of the aorta (Fig. 1; Gr 1.59, 1.61, 1.72; Ne 206, 220, 225, 226). Clean the left recurrent laryngeal branch that arises near the lower border of the aortic arch. It loops posteriorly under the arch to ascend in the groove between the trachea and esophagus (tracheoesophageal groove) (Gr 1.43, 1.59, 1.61, 1.63; Ne 206, 220, 226).
13. The left recurrent laryngeal nerve courses under the arch of the aorta to the left of a fibrous band, the ligamentum arteriosum, which joins the aortic arch and the left pulmonary artery (Fig. 1; Gr 1.43, 1.59, 1.61, 1.63, 1.76; Ne 200, 206, 225). Clean and preserve the ligamentum arteriosum. It is a remnant of the ductus arteriosus,whichshunted blood in the pulmonary trunk of the fetus away from the nonfunctional lungs and into the aorta.
The origin and course of the left recurrent laryngeal nerve in the thorax—the right recurrent laryngeal nerve arises in the root of the neck—means that the left recurrent laryngeal may be injured by intrathoracic lesions(e.g., metastatic bronchogenic carcinoma, aortic aneurysms). The resulting persistent hoarseness is sometimes the first sign of disease.
14. Follow the left vagus nerve inferiorly until it breaks into branches to form (mainly) the anterior part of the esophageal plexus. Follow the right vagus nerve along the right side of the trachea, medial to the arch of the azygos vein, and then posterior to the root of the right lung (Gr 1.75; Ne 224, 226, 234). Right vagus nerve branches contribute mainly to the posterior portion of the esophageal plexus. Other small branches from the right and left vagus nerves travel to the cardiac plexus of nerves below and behind the arch of the aorta and to the pulmonary plexusesnear the hila of the lungs. Subdivisions of these plexuses are described, but they are often difficult to demonstrate in dissections. XXX
The phrenic nerves descend through the superior mediastinum anterior to the roots of the lungs to enter the middle mediastinum (Fig. 1; Gr 1.21, 1.42, 1.75, 1.76; Ne 187, 206, 224, 225). Each phrenic nerve is derived from the anterior rami of spinal nerves 3-5 (“C3,4,5 keep the diaphragm alive”). Each nerve innervates the musculature in its half of the diaphragm (hemidiaphragm) and provides sensory innervation to all but the periphery of that half.
A lesion of a phrenic nerve results in paradoxical movement of the paralyzed hemidiaphragm during inspiration. For example, if the left half of the diaphragm is paralyzed, then it is pushed upward by abdominal viscera during inspiration while contraction of the intact right half of the diaphragm pulls it downward. This paradoxical movement can be detected on x-rays. Irritation of the diaphragmatic pleura or diaphragmatic peritoneum (i.e., pleura or peritoneum covering the diaphragm) may cause referred pain to the ipsilateral shoulder. That is because the skin of the shoulder receives innervation from the suprascapular nerves, which also contains nerve fibers from C3,4.
The trachea is the portion of the airway that begins in the neck at the inferior border of the cricoid cartilage, which is the lowest of the laryngeal cartilages (Gr 1.24, 1.33, 8.16E, 8.41; Ne 63, 68, 190, 196, 200, 228). The trachea has a wall that is reinforced anteriorly and laterally by C-shaped cartilaginous rings. The trachea descends through the lower neck and superior thoracic aperture and then behind the left brachiocephalic vein, brachiocephalic trunk, and arch of the aorta. The esophagus lies posterior to the trachea, separating it from the bodies of vertebrae (Gr 1.69, 1.75; Ne 226-228).
The trachea bifurcates into two primary (main) bronchi—right and left—at the level of the intervertebral disc between vertebrae Tv4/Tv5 (Gr 1.33, 1.63, 1.69; Ne 196, 226). Note that the right primary bronchus is wider and more vertically oriented than the left, making an inhaled foreign object more likely to enter the right primary bronchus. At the bifurcation of the trachea, the last tracheal cartilage sends a process, the carina, posteriorly between the primary bronchi. On an internal view of the bifurcation through a bronchoscope, the carina forms a ridge between the openings of the primary bronchi.
During the clinical evaluation of the trachea and bronchi, a bronchoscope is passed through the nose, pharynx, and larynx into the trachea. This allows examination of the internal structure of the trachea and bronchi and the extraction of small tissue samples. Distortion or deviation of the carina to one side during a bronchoscopic evaluation suggests the presence of a space-occupying lesion in the thorax (e.g., bronchogenic carcinoma that has metastasized to tracheobronchial lymph nodes [Gr 1.38, 1.69; Ne 202, 233]). The carina is covered by sensitive mucous membrane, and contact with an aspirated foreign object stimulates the cough reflex in an attempt to expel it from the airways. The general visceral afferent fibers of the cough reflex are part of the vagus nerves.
15. Study the bifurcation of the trachea into right and left primary bronchi. Look for small bronchial arteries running along the surface, usually the posterior surface, of the primary bronchi. There usually are two left bronchial arteries and one right bronchial artery to supply tissues of the lungs. Note the tracheobronchial lymph nodes just inferior to the bifurcation of the trachea and understand that their enlargement by metastases in bronchogenic carcinoma may distort and/or invade the carina. Make a square window ≈2 cm x 2 cm in the trachea just superior to its bifurcation and examine the carina. If you are unable to identify the carina, ask an instructor for help. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.