Anterior Abdominal Wall & Inguinal Region
The abdomen is the part of the trunk between the thorax and the pelvis. It consists of the abdominal wall enclosing the abdominal cavity. The anterolateral abdominal wall is formed by skin and subcutaneous tissue (superficial fascia) overlying three flattened layers of muscle—the external abdominal oblique, internal abdominal oblique, and transversus abdominis. These muscles develop from the inferior portion of the same three layers of hypomere as the three layers of intercostal muscles (Fig. 1). As in the thoracic wall neurovascular bundles traverse the fascial interval between the two inner layers of muscle.
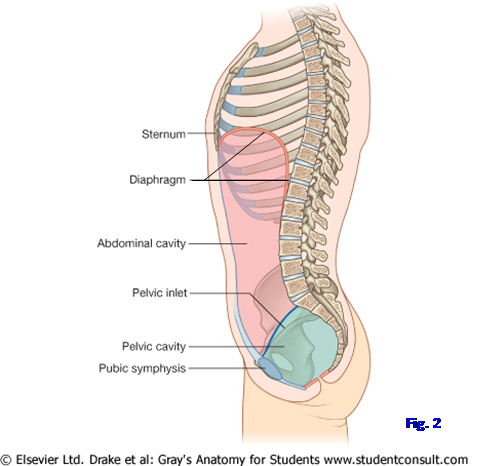
The abdominal cavity is the upper portion of a continuous abdominopelvic cavity bounded above by the respiratory diaphragm and below by the pelvic diaphragm, which separates the pelvic cavity (lesser pelvis, true pelvis) from the perineum (Fig. 2; Gr 2.22, 3.2; Ne 266, 323).
The abdominal cavity includes a serous sac (peritoneum) and the tissues that surround it inside the mostly muscular abdominal wall. The peritoneum is similar to pleurae and the serous pericardium and consists of visceral and parietal layers enclosing a potential space, the peritoneal cavity, which contains a small amount of serous fluid (Gr 2.22, 2.23B; Ne 323).
The largest amount of tissue in the abdominal cavity adjacent to the peritoneum is located posteriorly, the retroperitoneum (e.g., kidneys, aorta, inferior vena cava). The abdominal cavity will be considered in more detail during the next period.
1. On a skeleton identify the jugular (suprasternal) notch and xiphoid process of the sternum; the costal margin formed by the costal cartilages of ribs 7-10; the iliac crest, tubercle of the iliac crest, and anterior superior iliac spine; the pubic tubercle and pubic crest; the pubic symphysis; and the pecten pubis (pectineal line) (Gr 1.9, 3.1, 3.2A; Ne 179, 332, 335, 336).
While studying the rib cage, remember that the right dome of the diaphragm arches as high as the fifth rib and the left dome as high as the fifth intercostal space during expiration (Note: some authors substitute the fourth intercostal space and fifth rib, respectively). The upper abdominal organs (e.g., liver, spleen) are, therefore, protected by the lower ribs and their costal cartilages (Gr 2.1; Ne 190). Conversely, the upper abdominal organs may be injured during fractures of the lower ribs.
Clinically the abdominal cavity is subdivided into regions by one of two methods to describe the location of abdominal organs or a patient’s signs and symptoms. The simpler method is a division into quadrants—right upper quadrant, left upper quadrant, right lower quadrant, and left lower quadrant—by the vertical midsagittal (median) plane and the horizontal transumbilical plane (through the umbilicus).
The other method uses two vertical and two horizontal planes to divide the abdominal cavity into 9 regions. The two vertical planes pass through the midpoints of the clavicles (midclavicular planes). The lower horizontal plane is the intertubercular plane connecting the tubercles of the iliac crests. Clinicians use one of two different upper horizontal planes. Perhaps the more useful upper horizontal plane is the transpyloric plane. It is located midway between the jugular notch and the pubic symphysis at the level of vertebra Lv1. The transpyloric plane is so named because it intersects the pylorus, where the stomach opens into the first part of the small intestine, in the supine patient. The transpyloric plane intersects a number of other important structures, including the fundus of the gallbladder, neck of the pancreas, origins of the superior mesenteric artery and portal vein, etc.
SKIN AND SUPERFICIAL FASCIA
2. Turn the cadaver into the supine position. Make a shallow midline incision through only the skin from the xiphoid process to the symphysis pubis, encircling the umbilicus. The skin should already have been cut from the lower end of the first incision to the anterior superior iliac spine following the lower limb dissection. Reflect the two abdominal skin flaps laterally from the midline without disturbing the superficial fascia. XXX
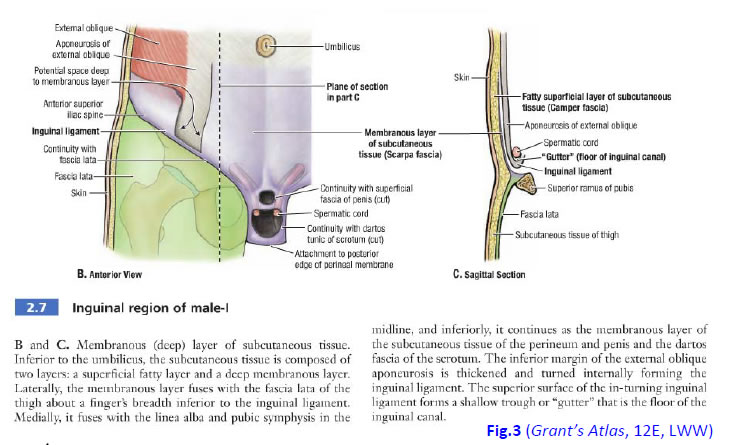
The superficial fascia above the umbilicus forms a single layer containing a variable amount of fat. The superficial fascia below the umbilicus differs from the superficial fascia in most other regions of the body in that it consists of two layers. The superficial fatty layer of superficial fascia is known as Camper’s fascia and is continuous with superficial fascia of the regions above and below it. The deeper membranous layer of superficial fascia is known as Scarpa’s fascia (Gr 2.7B-C, 2.11A; Ne 243, 346).
Surgeons may include Scarpa’s fascia during suturing of lower abdominal skin incisions for added strength. Scarpa’s fascia is continuous below with the superficial penile fascia, the dartos layer of the scrotum, and the membranous layer of superficial perineal fascia (Colles’ fascia) (Fig. 3 [Grant's], Gr 2.7B; Ne 346). The space deep to this continuous membranous layer provides a pathway for blood or extravasated urine from a ruptured penile urethra to ascend from the perineum into the anterior abdominal wall. The fluid doesn’t enter the thigh because the fusion of Scarpa’s fascia with the deep fascia of the thigh (fascia lata) blocks it.
3. Make a transverse incision through both layers of superficial fascia from one anterior superior iliac spine to the other. DO NOT cut into the muscles fibers and tough white aponeurosis of the external oblique muscle. Identify Camper’s and Scarpa’s fasciae. Probe through the fascia of the lower abdominal wall to find examples of cutaneous nerves (Gr 2.4; Ne 251, 252). In a male cadaver, try to insert a finger deep to Scarpa’s fascia over the anterior surface of the pubic bone into the scrotum (Gr 2.7B), verifying that there is continuity of the subcutaneous space from the lower abdominal wall. Note that there is no similar entrance into the thigh because Scarpa’s fascia fuses with the fascia lata. XXX
There are lateral and anterior cutaneous nerve branches in the abdominal wall just as in the thoracic wall. Intercostal nerves 7-11 continue from the thoracic wall into the anterior abdominal wall and, therefore, are called thoracoabdominal nerves (Gr 2.2, 2.4, 2.5; Ne 251, 252). The anterior ramus of T12 is the subcostal nerve. The iliohypogastric nerve, a branch of the anterior ramus of L1, supplies skin of the suprapubic part of the anterior abdominal wall. Notice that the T10 spinal nerve innervates the strip of skin (dermatome) that includes the umbilicus (Gr 2.2, 4.49; Ne 159). This is a useful reference point.
Two superficial arteries ascend from the femoral artery of each side into the lower abdominal wall and one superficial artery passes medially (Gr 2.4, 5.11; Ne 243, 249). The superficial epigastric artery inclines superomedially toward the umbilicus. The superficial circumflex iliac artery courses superolaterally along the inguinal ligament and above the anterior superior iliac spine. The third branch of the femoral artery, the external pudendal artery, passes medially toward the pubic symphysis. (Note: there are actually two external pudendal arteries on each side—superficial and deep—but the deep vessels are usually difficult to demonstrate in dissection).
The superficial epigastric vein descends beside the artery to end in the great saphenous vein of the thigh near its termination in the femoral vein (Gr 2.4; Ne 250). Anastomoses between the superficial epigastric vein and the lateral thoracic vein of the axilla form the thoracoepigastric vein, which is a collateral channel for returning blood to the heart in obstruction of the superior or inferior vena cava. The superficial circumflex iliac vein and external pudendal vein also are tributaries of the great saphenous vein.
4. Clean and identify the named cutaneous nerves, arteries, and veins of the lower abdominal wall. Identify examples of the thoracoabdominal nerves. Clean the iliohypogastric nerve. Find the superficial epiastric and superficial circumflex iliac arteries and veins. Were there identifiable thoracoepigastric veins in this cadaver? Understand their potential clinical significance. XXX
The three layers deep to the superficial fascia in the anterolateral abdominal wall consist of muscle fibers laterally and aponeuroses medially (Gr 2.4, 2.5, 2.6; Ne 243, 244, 245, 246). The aponeuroses fuse medially to form the sheath of the rectus abdominis muscle (rectus sheath), a vertically oriented muscle. At the midline the rectus sheaths of the two sides fuse to form a band of dense connective tissue, the linea alba, which extends from the xiphoid process to the pubic symphysis. The linea alba is sometimes used for surgical incisions because no large nerves or blood vessels cross the anterior midline. At the lateral edge of the rectus sheath is a curved groove extending from the inferior costal margin near the 9th costal cartilage down to the pubic tubercle (Gr 2.3; Ne 240). This linea semilunaris is a clinically useful landmark, and its junction with the 9th costal cartilage is the surface projection of the fundus of the gallbladder. Palpation at this spot is part of the physical examination in suspected acute inflammation of the gallbladder (acute cholecystitis).
External oblique (external abdominal oblique) muscle fibers are oriented inferomedially (in the same direction as external intercostal muscles). The fibers pass from the lower 8 ribs to attach into the iliac crest (the most posterior fibers) or end in the external oblique aponeurosis. Superior fibers of the aponeurosis contribute to the rectus sheath and then interdigitate with fibers of the other side in the linea alba. The external oblique aponeurosis has a rolled-under inferior free edge between the anterior superior iliac spine and pubic tubercle, forming the inguinal ligament (Gr 2.7A & C; Ne 243, 254, 256). Notice an opening in the external oblique aponeurosis above and slightly lateral to the pubic tubercle, the superficial inguinal ring.
Fibers of the internal oblique (internal abdominal oblique) muscle pass from the lateral half of the inguinal ligament, iliac crest, and thoracolumbar fascia superomedially at right angles to those of the external oblique (Gr 2.5, 2.8, 2.9; Ne 244). The internal oblique aponeurosis helps to form the rectus sheath before reaching the linea alba (Ne 244, 246). The lowermost fibers of the internal oblique muscle and aponeurosis arch medially and downward. These lowest muscle fibers in males form the cremaster muscle, which contributes a covering layer to the spermatic cord. The lowest part of the internal oblique aponeurosis joins that of the underlying transversus abdominis to attach into the pubic crest and pecten pubis as the conjoint tendon (falx inguinalis) (Gr 2.8A, 2.9; Ne 244, 254). The conjoint tendon reinforces the abdominal wall posterior to the superficial inguinal ring, resisting the development of a direct inguinal hernia.
The transversus abdominis muscle is the innermost musculoaponeurotic layer of the anterolateral abdominal wall and has transversely oriented muscle fibers (Gr 2.5, 2.6C; Ne 245, 246). The muscle has proximal attachments from the internal surfaces of costal cartilages 7-12, the thoracolumbar fascia, the iliac crest, and the lateral third of the inguinal ligament. Medially the aponeurosis contributes to the rectus sheath before ending in the linea alba. The lowest part of the aponeurosis joins that of the overlying internal oblique to arch downward and attach into the pubic crest and pecten pubis as the conjoint tendon.
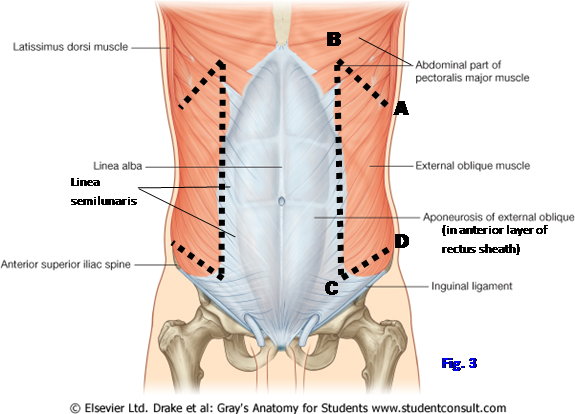
5. The muscle layers of the abdominal wall vary in thickness from individual to individual, so be careful not to cut too deeply when making incisions (Fig. 3). Clean the external oblique muscle and aponeurosis. Make the following incisions in the muscles on both sides:
A to B Cut the external oblique muscle along its attachments to the ribs and costal cartilages.
C to D Cut the external oblique parallel to, and 5 cm above, the inguinal ligament (i.e., above a line joining the anterior superior iliac spine and pubic tubercle).
B to C Make a cut just lateral to the linea semilunaris connecting the medial ends of the first two incisions.
6. Now reflect the external oblique muscle laterally.
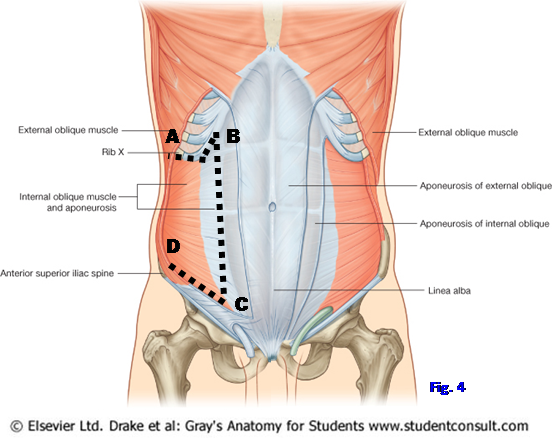
7. Deep to the external oblique is the internal oblique muscle and aponeurosis. The internal oblique may be partially fused with the underlying transversus abdominis, but the two can be distinguished by the different directions of their muscle fibers and by the presence of segmental nerves and blood vessels passing between them. Clean the internal oblique and make the following incisions on both sides (Fig. 4):
A to B Cut the proximal attachment of the internal oblique from the lower ribs and costal cartilages.
C to D Make an incision parallel to and above the inguinal ligament just superior to the incision made through the external oblique.
B to C Make an incision just lateral to the linea semilunaris connecting the medial ends of the first two incisions.
8. Clean the surface of the internal oblique muscle and find the iliohypogastric and ilioinguinal branches of spinal nerve L1 (Gr 2.5, 2.8; Ne 251, 260). XXX
The iliohypogastric nerve supplies motor branches to abdominal muscles and then becomes cutaneous to the pubic (hypogastric) region. The ilioinguinal nerve enters the inguinal canal deep to the external oblique aponeurosis and emerges through the superficial inguinal ring (Gr 2.9A; Ne 251, 260).
Turn your attention to the rectus abdominis muscleand therectus sheath. The rectus abdominis is a long, strap-like, vertically oriented muscle just lateral to the linea alba (Fig. 5; Gr 2.3, 2.4; Ne 240, 243, 244). It attaches inferiorly to the pubic crest. The much wider superior part of the rectus attaches to the xiphoid process and costal cartilages 5-7. The muscle belly is interrupted by 3-4 transverse bands of connective tissue called tendinous intersections, which are anchored to the anterior layer of the rectus sheath. The contraction of the portions of the muscle belly between the tendinous intersections is responsible for Dr. Roy’s washboard abs.
A small triangular muscle may be present anterior to the lower part of the rectus abdominis. This pyramidalis muscle arises from the body of the pubis and inserts into the linea alba between the pubic symphysis and umbilicus. Surgeons may use the attachment of the pyramidalis, when it is present, as a landmark for median abdominal incisions.
The rectus abdominis muscle is enclosed within the rectus sheath, which is formed by the aponeuroses of the three layers of flat abdominal muscles. The upper three-fourths of the rectus sheath consists of both anterior and posterior layers (i.e., layers anterior and posterior to the muscle), but the lower fourth of the sheath has only an anterior layer (Gr 2.5, 2.6C; Ne 245, 246). The inferior edge of the posterior layer of the rectus sheath is indicated by the crescentic arcuate line half way between the umbilicus and pubic symphysis. The arcuate line is more distinct in some cadavers than others but is usually recognizable. If you have difficulty finding it, look for the point at which the inferior epigastric artery and vein (from the external iliac artery and vein) enter the rectus sheath. This occurs at or near the arcuate line.
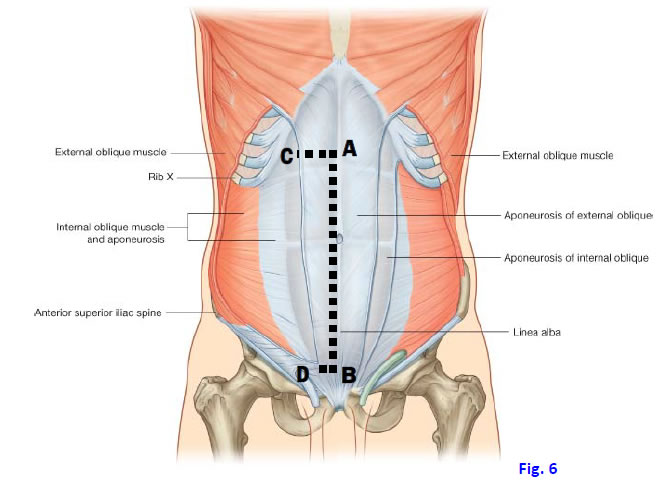
9. Incise the rectus sheath just lateral and parallel to the midline linea alba (Fig. 6, A-B). Carefully detach the anterior layer of the rectus sheath from the rectus abdominis muscle, cutting the attachments of the sheath to the underlying tendinous intersections. Make superior and inferior transverse incisions in the rectus sheath (Fig. 6, A-C and B-D). and retract it laterally.
10. Free the lateral edge of the rectus abdominis muscle from the linea semilunaris (Fig. 7 A-B). Divide the rectus abdominis transversely at the level of the umbilicus and carefully turn the upper and lower parts of the muscle laterally ![]() to expose structures enclosed within the rectus sheath posterior to the muscle. XXX
to expose structures enclosed within the rectus sheath posterior to the muscle. XXX
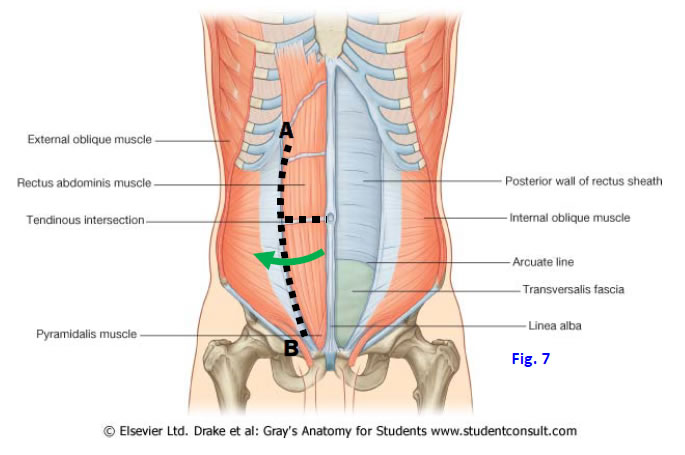
Superior to the arcuate line the internal oblique aponeurosis splits around the rectus abdominis. The anterior lamina of the internal oblique aponeurosis is fused to the aponeurosis of the external oblique to form the anterior layer of the rectus sheath (Gr 2.6C; Ne 246). The posterior lamina of the internal oblique aponeurosis is fused to the aponeurosis of the transversus abdominis to form the posterior layer of the rectus sheath.
Below the arcuate line all three aponeuroses pass anterior to the rectus abdominis; therefore, there is no posterior layer of the rectus sheath below the arcuate line. Instead the posterior surface of the lower quarter of the muscle rests against transversalis fascia, which is the name given to the portion of endoabdominal fascia that lies deep to the transversus abdominis.
11. Find examples of the anterior cutaneous nerves that pierce the rectus abdominis (Gr 2.4, 2.5; Ne 251, 252). Deep to the rectus abdominis try to find the anastomosis between the inferior epigastric artery (a branch of the external iliac artery) and the superior epigastric artery (a branch of the internal thoracic artery) (Gr 2.5; Ne 249). XXX
The anatomosis between the superior and inferior epigastric arteries is an important route for arterial blood to bypass the site of stenosis and reach the lower body in the congenital anomaly known as postductal coarctation of the aorta. A similar anastomosis between the superior and inferior epigastric veins providesan alternative route of venous return to the heart during obstruction of the superior or inferior vena cava.
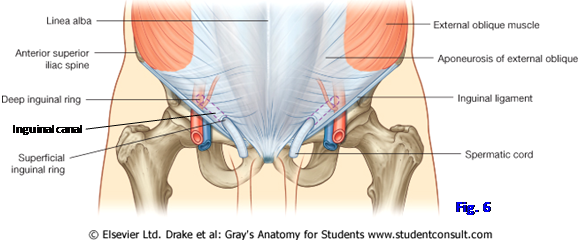
The inguinal region is the lower medial part of the anterior abdominal wall. It is clinically important due to the incidence of inguinal hernias, the most common type of hernia in both males and females.
A hernia is the protrusion of a structure from the space it normally occupies (Gr 2.15B-C). In an abdominal wall hernia, the herniating organ frequently is a loop of small intestine, which may have its lumen obstructed (bowel obstruction) or its blood supply compromised (strangulation), both of which are life-threatening emergencies. For example see http://www.emedicine.com/PED/topic2559.htm
Hernias are common in the inguinal region due to the presence of an oblique passage through the three musculoaponeurotic layers above the medial half of the inguinal ligament, the inguinal canal (Fig. 6; Gr 2.7-2.10, 2.15; Ne 254). The inguinal canal transmits the thick spermatic cord in the male and the thin round ligament of the uterus in the female, making the region inherently weaker and more disposed to the development of hernias in males. The ilioinguinal nerve also traverses the canal to emerge at the superficial inguinal ring in both sexes (Gr 2.4A; Ne 251, 260). It supplies cutaneous innervation over the upper medial thigh and the anterior scrotum or labium majus.
The inguinal canal extends from the deep inguinal ring in an anteromedial direction through the abdominal wall to the superficial inguinal ring (Fig. 6). The deep inguinal ring is an evagination of transversalis fascia above the midpoint of the inguinal ligament lateral to the inferior epigastric artery.
The superficial inguinal ring is an opening in the external oblique aponeurosis superior and slightly lateral to the pubic tubercle but medial to the inferior epigastric artery. The superficial inguinal ring is bounded by a lateral crus that attaches to the pubic tubercle, a medial crus that attaches to the pubic crest, and superolaterally by intercrural fibers that keep the two crura from splitting apart (Gr 2.8A; [in 2.7A note that the lateral and medial crura are incorrectly labeled as “Right and left crus”]; Ne 254). The lateral crus is continuous laterally with the inguinal ligament, the rolled-under inferior free edge of the external oblique aponeurosis between the anterior superior iliac spine and pubic tubercle.
Some deep fibers pass posteriorly and inferiorly from the medial end of the inguinal ligament to attach to the superior pubic ramus lateral to the pubic tubercle as the lacunar ligament. The lacunar ligament is continuous laterally with thickened periosteum over the pecten pubis (pectineal line), the pectineal (Cooper’s) ligament, which is used to anchor sutures in some types of hernia repair (Gr 2.7A, Table 3.2 [p.192]; Ne 245, 255, 256).
The inguinal canal has anterior and posterior walls, a roof, and a floor (Gr 2.7-2.10, 2.13A; Ne 243-245, 254). The anterior wall is formed mainly by the external oblique aponeurosis. Laterally, in front of the deep inguinal ring, the anterior wall is reinforced by the internal oblique muscle.
The posterior wall is formed by transversalis fascia. Medially, behind the superficial inguinal ring, the posterior wall is reinforced by the conjoint tendon.
The roof is formed by the arching inferior fibers of the internal oblique and transversus abdominis muscles (Ne 253, 254). The floor of the inguinal canal is the inguinal ligament, which is reinforced medially by the lacunar ligament (Gr 2.7A & C; Ne 255, 256).
Contraction of the abdominal wall muscles provides some protection against hernia development under normal circumstances. Due to the oblique orientation of the inguinal canal, the increase in intra-abdominal pressure from abdominal muscle contraction pushes the posterior wall of the inguinal canal toward the anterior wall, narrowing the width of the passage. Contraction of the internal oblique and transversus abdominis muscles pulls their arching lower fibers downward and decreases the height of the canal.
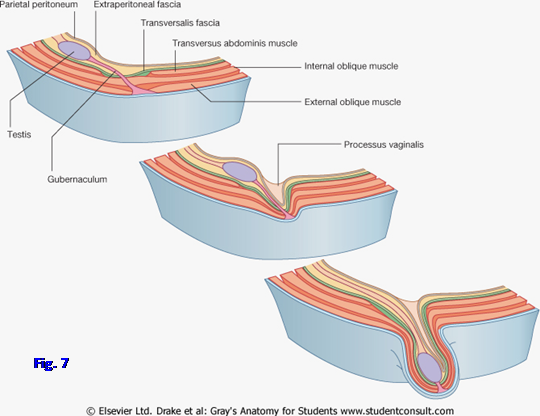
When an inguinal hernia does develop, it can be classified as either indirect or direct. In males an indirect inguinal hernia follows the path of embryonic descent of the testis from the posterior abdominal wall through the deep inguinal ring, inguinal canal, and superficial inguinal ring into the scrotum (Fig. 7). It leaves the abdominal cavity lateral to the inferior epigastric vessels. An indirect inguinal hernia results from a failure of closure of the peritoneal evagination that developed during descent of the testis, the processus vaginalis. (Note: the distal portion of the processus vaginalis normally persists around the testis in the male as the tunica vaginalis.) Consequently, the herniating structure has the same three coverings as the spermatic cord in the male—external spermatic fascia from the external oblique layer, cremasteric muscle and fascia from the internal oblique layer, and internal spermatic fascia from the transversalis fascia (Gr 2.15). An indirect inguinal hernia develops the same way in females as in males despite the fact that the ovary descends only as far as the pelvis. The processus vaginalis is associated with the gubernaculum as in the male. The herniating structure frequently descends into the scrotum or labium majus.
A direct inguinal hernia pushes directly forward through the abdominal wall at the superficial inguinal ring due to weakness, usually acquired rather than congenital, or narrowness of the conjoint tendon. A direct hernia thus leaves the abdominal cavity medial to the inferior epigastric vessels through the region known as the inguinal (Hesselbach’s) triangle. The inguinal triangle is bounded laterally by the inferior epigastric vessels, medially by the rectus abdominis muscle, and inferiorly by the inguinal ligament. Since the herniating structure does not traverse the inguinal canal, it typically does not have all of the three coverings as the spermatic cord; however, it is covered by transversalis fascia and acquires a covering of external spermatic fascia if it pushes through the superficial inguinal ring. In a direct inguinal hernia the herniating structure rarely enters the scrotum.
12. On the cadaver pull the cut edges of the external and internal oblique layers forward to find the deep inguinal ring above the midpoint of the inguinal ligament. Identify the superficial inguinal ring bordered by the lateral crus, medial crus, and intercrural fibers. Find the spermatic cord or round ligament of the uterus emerging through the superficial inguinal ring with the ilioinguinal nerve lateral to it. In the male cadaver pull the external oblique aponeurosis forward to see cremaster muscle fibers leaving the internal oblique layer to accompany the spermatic cord (Gr 2.9; Ne 244, 254).
13. Look for the tiny cremasteric branch of the inferior epigastric artery and the genital branch of the genitofemoral nerve supplying the cremaster muscle. Study the fusion of the internal oblique and transversus abdominis aponeuroses medially to form the conjoint tendon, which attaches to the pubic crest and medial part of the pecten pubis. A weak conjoint tendon posterior to the superficial inguinal ring can result in the development of a direct inguinal hernia. Finally elevate the lower edge of the transversus abdominis just medial to the deep inguinal ring and look for the origin of the inferior epigastric artery from the external iliac artery. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.