The Abdominal Cavity, Gastrointestinal Tract
NOTE: This set of dissection instructions is for two laboratory periods. There is sufficient time to perform a thorough study and review.
The abdominal cavity is the upper portion of a continuous abdominopelvic cavity bounded above by the respiratory diaphragm and below by the pelvic diaphragm, which separates the pelvic cavity from the perineum (Fig. 1; Gr 2.22, 3.2; Ne 323). The abdominopelvic cavity contains a serous sac, the peritoneum, and the tissues around it inside a musculoaponeurotic and skeletal abdominal wall. The peritoneum has visceral and parietal layers enclosing a potential space, the peritoneal cavity, that normally contains only a small amount of serous fluid (Gr 2.22, 2.23B; Ne 323, 327). This is the same basic arrangement that was seen in the pericardial and pleural cavities, with which the peritoneal cavity shares a developmental origin. The accumulation of excess fluid within the peritoneal cavity (ascities) can result from a number of pathological conditions (e.g., cirrhosis, cancer, infection). The peritoneal cavity may be punctured and some of the fluid aspirated for analysis or the excess fluid may be drained (paracentesis), e.g., to relieve respiratory distress.
The visceral layer of peritoneum forms the outer layer (serosa) covering some abdominal organs. The parietal layer of peritoneum lines the inside of the abdominal wall and the inferior surface of the respiratory diaphragm. Immediately outside the parietal peritoneum is a layer of extraperitoneal connective tissue. The largest amount of extraperitoneal connective tissue in the abdominal cavity is located posteriorly, the retroperitoneum, enclosing multiple organs (e.g., the kidneys, pancreas, aorta).
Parts of the peritoneum that connect two organs or connect organs to the abdominal wall are given special names. A mesentery is a double layer of peritoneum that suspends an organ (e.g., small intestine, transverse colon) from the abdominal wall because the organ had invaginated the peritoneal sac from behind during embryonic development (Fig. 1). Nerves and vessels that supply the suspended organ reach it through the mesentery. The more obvious mesenteries are the mesentery (proper) for the jejunum and ileum of the small intestine, the transverse mesocolon for the transverse colon, and the sigmoid mesocolon for the sigmoid colon.
An omentum is a double layer of peritoneum that connects the stomach to adjacent organs. The greater omentum (or more specifically its gastrocolic ligament component) is an apron-like peritoneal fold that usually hangs in front of the small intestine (Gr 2.19, 2.20A; Ne 261, 267). Its anterior layer descends from the greater curvature of the stomach and its posterior layer ascends to fuse with visceral peritoneum on the transverse colon and with the transverse mesocolon (Fig. 1; Gr 2.22; Ne 323). The lesser omentum passes from the lesser curvature of the stomach and the first part of the duodenum below to the liver above. The lesser omentum is correspondingly subdivided into hepatogastric and hepatoduodenal ligaments (Ne 267).
Organs that are suspended by a mesentery have a covering of visceral peritoneum and are classified as intraperitoneal organs. Some intraperitoneal organs have no obvious mesentery but nevertheless are enclosed by visceral peritoneum. These include the liver, gallbladder, and cecum.
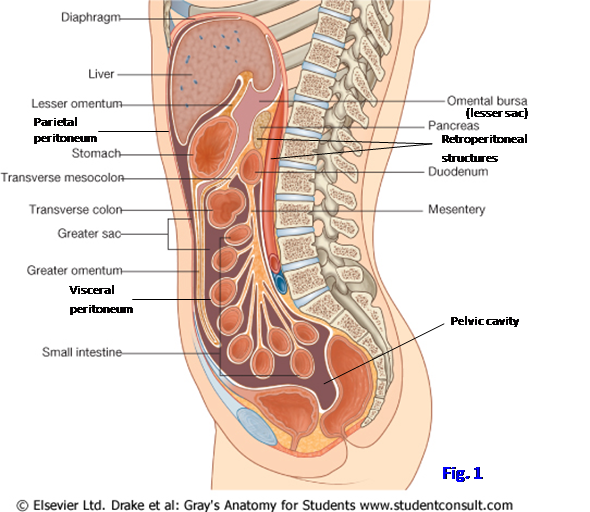
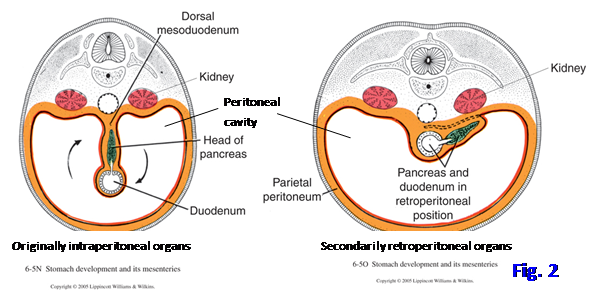
Organs that remain behind the peritoneal sac and lack a mesentery are classified as retroperitoneal organs. They either are not covered at all with peritoneum, or are covered only on their anterior surface. Retroperitoneal organs include most of the duodenum and pancreas, ascending and descending colons, kidneys and ureters, suprarenal glands, abdominal aorta, and inferior vena cava. Of these, the first four mentioned—duodenum, pancreas, ascending colon, and descending colon—were originally intraperitoneal during embryonic development and later became retroperitoneal during rotation of the gut and fusion of various fasciae. The originally intraperitoneal organs that later became retroperitoneal—duodenum, pancreas, ascending colon, and descending colon—are said to be secondarily retroperitoneal (Fig. 2). The organs that were originally retroperitoneal and remained that way are said to be primarily retroperitoneal.
The peritoneal cavity is a closed sac in males. In females the open ends (ostia) of the uterine tubes connect the peritoneal cavity with the outside world via the uterine tubes, cavity of the uterus, and the vagina. This provides a potential pathway for an external infection to enter the peritoneal cavity, resulting in peritonitis. The patency of the uterine tubes can be examined by injection of a radiopaque dye into the uterine cavity, from where it normally flows through the uterine tubes into the peritoneal cavity (hysterosalpingography) (Gr 3.33B).
The peritoneal cavity is a closed sac in males. In females the open ends (ostia) of the uterine tubes connect the peritoneal cavity with the outside world via the uterine tubes, cavity of the uterus, and the vagina. This provides a potential pathway for an external infection to enter the peritoneal cavity, resulting in peritonitis. The patency of the uterine tubes can be examined by injection of a radiopaque dye into the uterine cavity, from where it normally flows through the uterine tubes into the peritoneal cavity (hysterosalpingography) (Gr 3.33B [no image]).
The peritoneal cavity is subdivided into the small lesser peritoneal sac (omental bursa) behind the stomach and lesser omentum and the large greater peritoneal sac, which occupies the rest of the peritoneal cavity (Fig. 1; Gr 2.22, 2.23B; Ne 323, 327). The lesser and greater sacs communicate on the right side through the omental (epiploic) foramen, which is located posterior to the hepatoduodenal ligament above the first part of the duodenum (Gr 2.20, 2.22, 2.23A; Ne 267, 323, 327).
1. The abdominal cavity will be opened in different ways by even-numbered and odd-numbered dissection groups.
2. On EVEN-NUMBERED TABLES, using a Stryker saw, cut through the remaining ribs (most likely 6th to 11th ribs) and intercostal spaces at the anterior axillary line on both sides to extend the vertical cuts used in removing the anterior thoracic wall in previous dissections. Extend the cuts further inferiorly towards the iliac crests using scissors to cut through the
three abdominal muscle layers in the midaxillary line. Be careful to cut only through the abdominal wall muscles and not into the parts of the colon in these areas! Then, extend the cuts anteriorly towards the anterior superior iliac spines (ASIS) using your scalpel, cutting through the attachment of the three flat muscles along the contour of the iliac crest. Be careful not to cut farther anteriorly than the ASIS.
3. From the superior end of one vertical cut, use scissors or a scalpel to cut through the anterior attachments of the diaphragm about 2-3 cm away from the sternum and costal cartilages. Carefully pull the anterior abdominal wall attached to the lower part of the sternum and lower part of the anterior thoracic cage forward until you see a sagittally oriented peritoneal reflection attaching the upper part of the anterior abdominal wall to the liver. This is the falciform ligament (Gr 2.18, 2.19; Ne 247, 277 [Anterior view]), which contains the ligamentum teres hepatis (round ligament of the liver) and paraumbilical veins in its inferior free edge. The ligamentum teres hepatis is the fibrous remnant of the umbilical vein. Cut the falciform ligament as close to the anterior abdominal wall as possible and reflect the abdominal wall forward.
4. If there is difficulty reflecting the anterior abdominal wall forward, it is probably due to adhesions. These basically are fibrous bands of scar tissue where the visceral peritoneum covering abdominal organs (e.g., small intestine) fuses to the parietal peritoneum lining the inside of the abdominal wall or where the visceral peritoneum covering two abdominal organs fuses. Such adhesions frequently form following abdominal surgery or inflammation of the peritoneum due to infection or other injury (peritonitis) and may cause pain and intestinal obstruction. If adhesions are present in the cadaver, they must be carefully torn by pulling the fused surfaces away from each other. If you have difficulty doing this, seek faculty assistance.
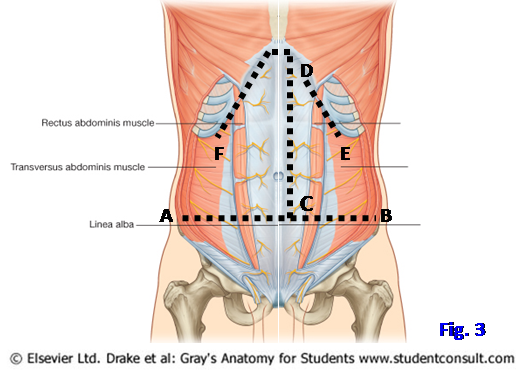
5. On ODD-NUMBERED TABLES, open the abdominal cavity by making the incisions in the abdominal wall indicated in Fig. 3:
6. A to B Pull the anterior abdominal wall forward and carefully make a transverse incision through it from 2 cm above one anterior superior iliac spine to 2 cm above the other. In making this incision, you will be cutting the transversus abdominis muscle of each side and, if they were not previously transected, the rectus abominis muscles. The cut will also include the linea alba and posterior layer of the rectus sheath on each side of it, as well as transversalis fascia, extraperitoneal connective tissue, and parietal peritoneum.
C to D Next make a vertical incision through the abdominal wall above the level of the first incision just to the left side of the linea alba.
D to E Detach the left side flap from the costal arch in order to reflect it laterally.
D to F Before cutting the right side flap from the costal arch, it is necessary to cut the peritoneal ligament that connects the liver to the anterior abdominal wall above the umbilicus, the falciform ligament (Gr 2.18, 2.19; Ne 247, 261, 277). Enclosed within its inferior free border is the fibrous remnant of the umbilical vein, the ligamentum teres hepatis(round ligament of the liver), passing from the umbilicus to the liver. Cut the falciform ligament and ligamentum teres hepatis ≈1 cm behind the anterior abdominal wall. Then make the cut D to F and reflect the right side flap laterally.
7. If there is difficulty reflecting the anterior abdominal wall forward, it is probably due to adhesions. These basically are fibrous bands of scar tissue where the visceral peritoneum covering abdominal organs (e.g., small intestine) fuses to the parietal peritoneum lining the inside of the abdominal wall or where the visceral peritoneum covering two abdominal organs fuses. Such adhesions frequently form following abdominal surgery or inflammation of the peritoneum due to infection or other injury (peritonitis) and may cause pain and intestinal obstruction. If adhesions are present in the cadaver, they must be carefully torn by pulling the fused surfaces away from each other. If you have difficulty doing this, seek faculty assistance. XXX
The internal (posterior) surface of the anterolateral abdominal wall is viewed during some laparoscopic surgeries (e.g, inguinal or femoral henia repair), and a physician needs to be familiar with its basic features. There are five umbilical peritoneal folds and associated depressions, the peritoneal fossae, on the internal surface. The umbilical peritoneal folds are the median, medial, and lateral umbilical folds. The median umbilical fold is parietal peritoneum raised over a fibrous remnant of the embryonic allantois, the urachus. The median fold extends upward from the apex of the urinary bladder to the umbilicus (Gr 2.18, 3.13B; Ne 247, 347). A patent urachus (urachal fistula) in a newborn may result in urine leaking from the umbilicus.
The medial umbilical fold on each side is parietal peritoneum raised over the medial umbilical ligament, which also ascends to the umbilicus. The medial umbilical ligament is the obliterated distal portion of the umbilical artery. Laterally on each side is the lateral umbilical fold. It is parietal peritoneum raised over the inferior epigastric artery and vein, which ascend medially to enter the rectus sheath near the arcuate line.
The supravesical fossa lies above the bladder between the median and medial umbilical folds. The medial inguinal fossa is bounded by the medial and lateral umbilical folds. The lower part of the medial inguinal fossa, lateral to the rectus abdominis and above the iliopubic tract, is the inguinal (Hesselbach’s) triangle. The iliopubic tract is a thickening of transversalis fascia that parallels the internal surface of the inguinal ligament. The inguinal triangle is the site where a direct inguinal hernia leaves the abdominal cavity.
The lateral inguinal fossa is lateral to the lateral umbilical fold. Note the ductus deferens and testicular vessels or the round ligament of the uterus entering the deep inguinal ring in the lower part of the lateral inguinal fossa. The deep inguinal ring is where an indirect inguinal hernia leaves the abdominal cavity.
8. Pull the anterior abdominal wall forward so that you can examine the lower part of its posterior surface (Gr 2.18, 3.13B; Ne 247, 347). This internal view of the anterior abdominal wall is the one seen during laparoscopic surgery. Identify the median, medial, and lateral umbilical folds. Note the slight depressions between the umbilical folds and identify these peritoneal fossae. They are the supravesical fossa, medial inguinal fossa, and lateral inguinal fossa.
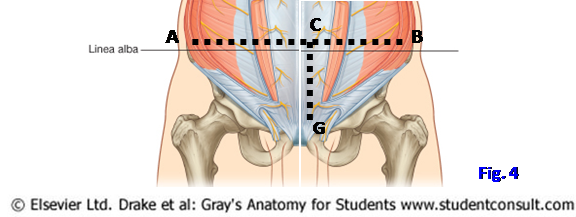
9. For groups on ODD-NUMBERED TABLES, as shown in Fig. 4, C to G open the lower part of the anterior abdominal wall by making an incision just to the left side of the linea alba from the edge of the original transverse cut (A-B) down to the pubic bone. Reflect the flaps laterally and downward toward the inguinal canal.
10. ALL TABLES: The remaining instructions in this dissection apply to ALL TABLES.
11. The abdominal cavity should now be fully exposed (Gr 2.19; Ne 261). Explore the abdominal organs in situ visually and by palpation. It again may be necessary to break adhesions.
LIVER AND ASSOCIATED STRUCTURES
12. Examine the large liver, which is responsible for the right dome of the diaphragm and extends across the midline to near the left midclavicular line (Ne 261, 277). On the right side of the liver, projecting below its sharp inferior border, look for the fundus of the gallbladder, which usually is stained dark green by stored bile in the cadaver. Note that the surface projection of the fundus is at the tip of the 9th costal cartilage near the linea semilunaris. The gallbladder may have been surgically removed (cholecystectomy) in some cadavers.
13. Find the ligamentum teres hepatis enclosed within the inferior free margin of the falciform ligament, which is the vertical peritoneal fold connecting the liver and the anterior body wall. It was cut earlier when the abdominal cavity was opened.
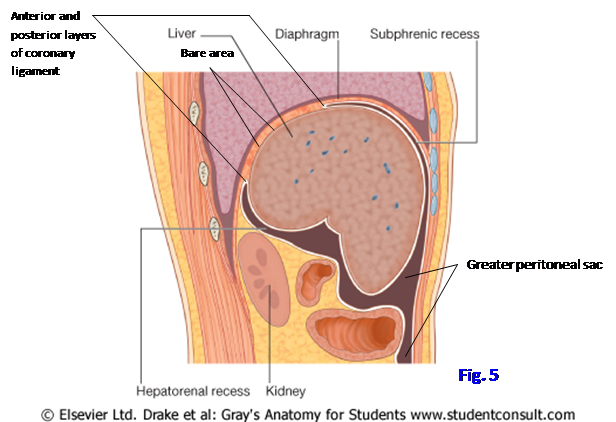
14. Insert your hand into the narrow space between the liver and diaphragm, beside the falciform ligament (Fig. 5). This space is the subphrenic recess, which is a common site for abscess formation within the peritoneal cavity. Now try to push your hand below and behind the right lobe of the liver into the hepatorenal recess or pouch (Morison’s pouch) in front of the right kidney (Gr 2.35; Ne 317 [unlabeled], 327). XXX
In a supine patient the hepatorenal recess is the lowest part of the peritoneal cavity. Therefore, gravity may cause infectious fluids to drain into it from the subphrenic recesses or omental foramen. The subphrenic recesses are frequent sites of abscess formation, which may result in referred pain to the shoulder from irritation of the diaphragmatic peritoneum. For more on abdominal abscesses, see http://emedicine.medscape.com/article/189468-overview.
In Fig. 5, notice that the liver is suspended from the diaphragm by peritoneal reflections, the anterior and posterior layers of the coronary ligament.The liver is covered by visceral peritoneum except for a posterior bare area, which isin direct contact with the diaphragm.
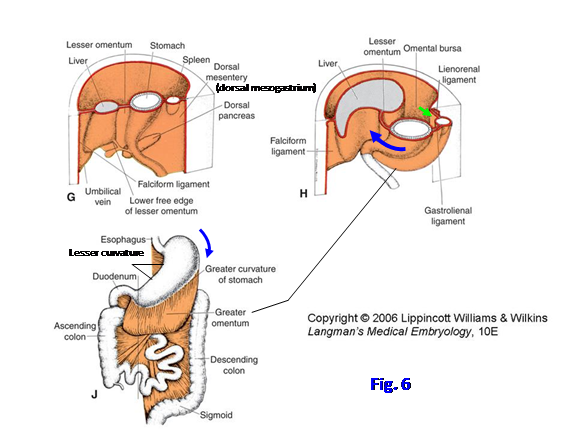
The stomach is saclike dilatation of the digestive tract connecting the abdominal portion of the esophagus and the small intestine(Gr 2.19, 2.20, 2.27A; Ne 261, 267, 268, 269). What was originally the left side of the embryo’s stomach faces anteriorly in the adult due to the stomach’s 90° clockwise rotation around a longitudinal axis (![]() ) during development (Fig. 6). The stomach also rotates 90° around an anteroposterior axis (
) during development (Fig. 6). The stomach also rotates 90° around an anteroposterior axis (![]() ) during development.
) during development.
The stomach has four parts (Gr 2.27, 2.31B, C, D; Ne 267, 268). The cardia (cardiac part) surrounds the cardial orifice, the opening into the stomach at the gastroesophageal junction. The fundus is the dilated superior part of the stomach to the left of the cardia. It is related to the left dome of the diaphragm and often contains gas in x-rays. The body forms the major part of the stomach. The pyloric part is the funnel-shaped outflow region of the stomach. It consists of the pyloric antrum leading into the narrow pyloric canal. The angular incisure on the lesser curvature indicates the junction between the body and pyloric antrum. The pylorus consists of the opening of the stomach into the first part of the duodenum, the pyloric orifice, surrounded by the thick, circular smooth muscle of the pyloric sphincter. Relaxation of the pyloric sphincter under parasympathetic control of the vagus nerves (anterior vagal trunk) allows emptying of the stomach.
The stomach has two curvatures. The lesser curvature of the stomach faces superiorly and to the right. The angular incisure indicates the junction of the body and pyloric part of the stomach. The lesser curvature and the first part of the duodenum are attached to the liver by the hepatogastric and hepatoduodenal ligaments, respectively, which are parts of the lesser omentum.
The spleen is the largest of the lymphatic organs. It lies deep to ribs 9-11 on the left side with its long axis roughly parallel to the 10th rib. Despite this seemingly protected position, the living spleen is relatively fragile and it is the most frequently injured abdominal organ. It rests on the shelf of peritoneum (phrenicocolic ligament) that suspends the angled junction of the transverse and descending colons (splenic, or left colic, flexure) from the diaphragm. The spleen is positioned between the stomach and left kidney by two other peritoneal ligaments, the gastrosplenic (gastrolienal) ligament and the splenorenal (lienorenal) ligament (Fig. 6H; Gr 2.23B; Ne 264, 327).
Pay particular attention to the relationships of the spleen on the left side and of the liver on the right side (Gr 2.20A, 2.21, 2.63; Ne 242, 267, 278, 308). Each organ lies deep to the lower ribs but is separated from them by the diaphragm and the costodiaphragmatic recess of its side. The liver and spleen may be damaged by blunt abdominal trauma with or without fractures the lower ribs. During biopsies of the spleen and liver, care must be taken not to damage a lung or its pleura. During a liver biopsy, a trocar or needle inserted through the right 9th or 10th intercostal space in the midaxillary line would penetrate, in order, the skin and superficial fascia; intercostal muscles; endothoracic (extrapleural) fascia; costal pleura, costodiaphragmatic recess, and diaphragmatic pleura; diaphragm; diaphragmatic peritoneum, subphrenic recess, and visceral peritoneum; and the liver. In patients with ascites or increased risk of bleeding a transjugular approach may be used to perform the liver biopsy: internal jugular vein![]() brachiocephalic vein
brachiocephalic vein![]() superior vena cava
superior vena cava![]() right atrium
right atrium![]() inferior vena cava
inferior vena cava![]() hepatic vein
hepatic vein![]() liver. Thus, any resultant bleeding is back into the venous system.
liver. Thus, any resultant bleeding is back into the venous system.
15. Examine the stomach. Identify the fundus, body, pyloric part, and pylorus. Squeeze the pylorus to appreciate the thickness of the pyloric sphincter. Lift the left lobe of the liver to better see the lesser curvature of the stomach facing superiorly and to the right. Is the angular incisure apparent? Note the hepatogastric and hepatoduodenal ligaments.
16. Put your hand inside the left costal margin and follow the curvature of the ribs posteriorly to near the midaxillary line, where you should feel a hard organ deep to ribs 9-11. This is the spleen. Understand how fractures of the lower ribs on the left side can cause lacerations and hemorrhaging from the spleen. XXX
The stomach opens into the small intestine, which is the primary site for the absorption of nutrients (Gr 2.26). The small intestine consists of the duodenum, jejunum, and ileum. All of the duodenum, except the first couple of centimeters, is retroperitoneal and will be studied later. The junction of the duodenum and jejunum, the duodenojejunal junction, is where the small intestine again becomes an intraperitoneal organ. The jejunum and ileum are intraperitoneal.
The small intestine opens into the large intestine at the ileocecal junction (Gr 2.26; Ne 273, 274). The large intestine is a site for water absorption and the temporary storage of the resulting semisolid feces until its elimination. The large intestine comprises the cecum and appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and upper part of the anal canal.
17. Lift the greater omentum superiorly and drape it over the sternum and costal cartilages, breaking any adhesions that may hamper its reflection (Gr 2.39, 2.40; Ne 261). Note that the portions of the small intestine now visible, the jejunum and ileum, are framed on three sides by large intestine. XXX
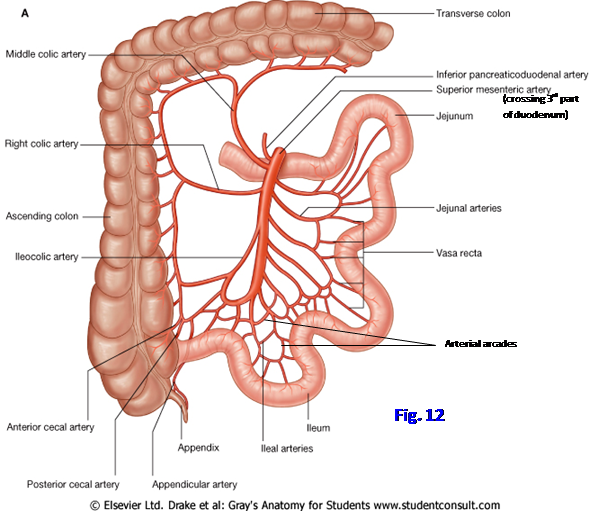
The mesentery that suspends the jejunum and ileum from the posterior abdominal wall has a fan-shaped structure. Its attachment on the abdominal wall, the root of the mesentery, extends from the duodenojejunal junction to the ileocecal junction, a length of about 15 cm (6 inches) (Gr 2.23A; Ne 266, 270). The much longer intestinal side of the mesentery, attached to the jejunum and ileum, averages about 7 m (21 feet). Therefore, the small intestine is highly coiled.
Distinguishing the jejunum from the ileum may be difficult, especially if adhesions are present. The jejunum forms the proximal two-fifths of their combined length and lies mainly in the left upper quadrant. The ileum makes up the distal three-fifths and is mostly in the right lower quadrant.
There is a gradual transition in structure between jejunum and ileum, but the proximal jejunum can be distinguished from the distal ileum by the amount of fat in the mesentery and the arrangement of its arterial supply (Gr 2.43; Ne 272). The mesentery of the proximal jejunum usually contains little fat and may be translucent, while the mesentery of the distal ileum is laden with fat (Gr 2.43, insets). The proximal jejunum also is characterized by only 1-2 arterial arcades (anastomotic loops) and long vasa recta (straight arteries) in its mesentery, while the distal ileum typically has 3-5 arterial arcades and short vasa recta. The jejunum and ileum develop from the embryonic midgut and, therefore, the arterial supply is from the superior mesenteric artery (Gr 2.43, 2.44; Ne 287).
18. Bluntly dissect the arterial arcades and vasa recta in the mesentery along several centimeters of the proximal jejunum and the distal ileum. Notice the relative amounts of fat that you need to remove in each location to expose the vessels. The proximal jejunum characteristically has fewer arterial arcades and longer vasa recta than the distal ileum. The origin of the arterial supply from the superior mesenteric artery will be dissected later. XXX
The jejunum and ileum are framed by the cecum and ascending colon on the right side, the transverse colon above, and the descending colon on the left side (Gr 2.26, 2.39, 2.41; Ne 261, 263). The large intestine is approximately 1.7 m (5 feet) in length and has features, aside from position, that usually make it easy to distinguish from the small intestine.
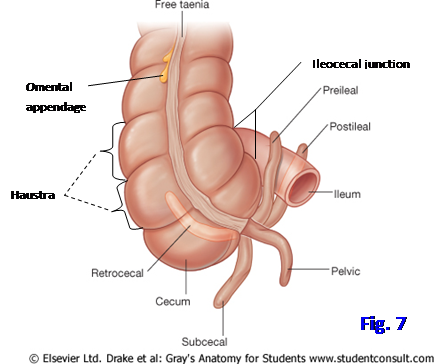
The outer longitudinal layer of smooth muscle in the large intestine is incomplete and arranged in three narrow bands, the teniae coli (Gr 2.42, 2.43, 2.47; Ne 273, 276). The appendix, rectum, and upper portion of the anal canal are exceptions and have a complete longitudinal layer of smooth muscle. This fact may be used to find an elusive appendix by tracing the convergence of the three teniae coli toward its base. The teniae coli are slightly shorter than the rest of the colon, drawing its wall into a series of sacculations, the haustra. Also characteristic of the large intestine is the presence of fat-filled pouches of visceral peritoneum, the omental (epiploic) appendices, suspended from it.
Study the cecum and appendix. The cecum is a blind pouch located in the iliac fossa of the right lower quadrant. It receives the ileum at the ileocecal junction, which is guarded by an ileocecal valve (Fig. 7; Gr 2.1A, 2.26, 2.41-2.43, 2.47; Ne 273, 274, 276). The ileocecal valve prevents the reflux of chyme into the terminal ileum. The valve may be obstructed by a gallstone (gallstone ileus) that has entered the lumen of the intestine (usually the superior part of the duodenum or the transverse colon) via a fistula with the gallbladder (cholecystenteric fistula).The cecum has no distinct mesentery but in most bodies it is enveloped by peritoneum and, therefore, is mobile. It is classified as an intraperitoneal organ.
The appendix (vermiform appendix) is a diverticulum of the posteromedial wall of the cecum below the ileocecal junction (Gr 2.42; Ne 273-275). Usually it is short, 6-10 cm, but occasionally it may be 20 cm or more in length. The appendix has a short mesentery, the mesoappendix, derived from the mesentery of the terminal ileum. Although the base of the appendix occupies a relatively constant position one-third of the distance along a line drawn from the right anterior superior iliac spine to the umbilicus (McBurney’s point), the orientation of the appendix is variable (). The majority of the time (≈65%) the appendix extends superiorly behind the cecum toward the right colic flexure (retrocecal position). The variability in anatomical position is important because it determines the signs and symptoms as an inflamed appendix (appendicitis) irritates contiguous structures. Typically appendicitis presents with vague periumbilical pain that later shifts to become severe right lower quadrant pain. The initial vague pain is due to visceral afferent (GVA) innervation, while the subsequent sharp, localized right lower quadrant pain results from irritation of the parietal peritoneum, which is innervated by somatic afferent (GSA) nerve fibers. Flexing the right thigh without resistance may relieve the patient’s pain by relaxing the psoas major muscle, but flexing the thigh against resistance or extending it may increase pain due to the irritation resulting from inflammation (positive psoas/iliopsoas sign). Vomiting, when it occurs, characteristically follows the onset of appendicitis pain, whereas vomiting that precedes pain suggests another cause, such as intestinal obstruction.
19. Find the ileocecal junction. Study the cecum and appendix. Verify that the cecum occupies the iliac fossa of the right lower quadrant. What is the orientation of the appendix in your cadaver, or has it been surgically removed (appendectomy)? If the appendix is still present, look for the short mesoappendix derived from the mesentery of the terminal ileum. The appendicular artery, a branch of the ileocolic artery or its posterior cecal branch, enters the mesoappendix by passing posterior to the terminal ileum. XXX
The ascending colon passes superiorly from the cecum along the right side of the abdominal cavity toward the right lobe of the liver (Gr 2.26, 2.39, 2.41, 2.47; Ne 261, 263). There it has an angled junction with the transverse colon at the hepatic (right colic) flexure. The ascending colon is secondarily retroperitoneal. A deep vertical groove, the right paracolic gutter, lies between the lateral aspect of the ascending colon and the abdominal wall.
The transverse colon is the longest part of the large intestine and crosses the abdominal cavity from right to left. It has a mesentery, the transverse mesocolon, and hangs down a variable distance toward the pelvis (Gr 2.39, 2.41; Ne 261). The attachment of the transverse mesocolon on the posterior abdominal wall crosses the descending (2nd) part of the duodenum and the inferior border of the pancreas (Gr 2.23A, 2.62A; Ne 266, 270).
The transverse colon is continuous with the descending colon at the splenic (left colic) flexure, which is usually somewhat posterior and superior to the hepatic flexure (Gr 2.26, 2.39, 2.41; Ne 270, 276). The descending colon descends along the left side of the abdominal cavity to become continuous with the sigmoid colon in the left iliac fossa. Like the ascending colon, the descending colon is secondarily retroperitoneal. The left paracolic gutter is located on its lateral aspect.
Located lateral to the ascending and descending colons are vertical grooves lined with parietal peritoneum. These right and left paracolic gutters, respectively, provide pathways for the movement of infectious fluid or cancer cells into the pelvic cavity in the upright patient. In fact, patients with peritonitis may be propped in a seated position to facilitate the flow of infectious fluid into the pelvis, where the absorption of toxins is slower than it is nearer to the diaphragm. Since the ascending and descending colons are secondarily retroperitoneal organs with a mesentery that fused to the posterior abdominal wall on their medial side during development, the paracolic gutters also provide an approach for surgical mobilization of the ascending and descending colons that doesn’t endanger their nerve and blood supplies.
The sigmoid colon is an S-shaped segment of colon of variable length. It is continuous above with the descending colon in the iliac fossa and below with the rectum in the pelvis in front of the third sacral vertebra (Sv3). The sigmoid colon is suspended by the sigmoid mesocolon from its attachment on the posterior abdominal wall, the root of the sigmoid mesocolon (Gr 2.23A; Ne 263, 266). The root is roughly in the form of an inverted V with the apex over the terminal division of the left common iliac artery. The sigmoid colon is the most common site of volvulusresulting from twisting of the colon around its mesentery with intestinal obstruction and possible necrosis due to loss of the blood supply (e.g., see http://www.learningradiology.com/notes/ginotes/sigmoidvolvpage.htm ) . The sigmoid colon is also the most frequent location for the development of outpouchings of the intestinal mucosa (diverticulosis), which commonly occurs in middle-aged and elderly individuals, probably due to a lifetime of insufficient fiber in the diet. Diverticula are prone to infection and inflammation (diverticulitis), hemorrhage, and perforation (producing peritonitis). For example, see http://digestive.niddk.nih.gov/ddiseases/pubs/diverticulosis/ The rectum will be studied with other pelvic organs.
FOLLOWING THE VASCULATURE
During this next section, the study of the abdominal portion of the digestive tract will be approached by following its blood supply. To truly understand the abdomen, one must have an appreciation of its vasculature. Gastrointestinal organs will then be displaced to study other retroperitoneal organs and the posterior body wall.
Once again review the organization of the peritoneal cavity. It consists of a greater peritoneal sac and a lesser peritoneal sac, or omental bursa. The omental bursa (lesser sac) communicates with the greater sac only at the omental (epiploic) foramen (Gr 2.20, 2.22, 2.23B, 2.24; Ne 265, 267, 323, 327).
The omental foramen is bounded anteriorly by the hepatoduodenal ligament, which is the free right edge of the lesser omentum that contains the bile duct, proper hepatic artery, and portal vein (Gr 2.23, 2.35, 2.36; Ne 265, 266, 278, 283, 327). The posterior boundary of the omental foramen is the inferior vena cava behind parietal peritoneum, the superior boundary is the caudate lobe of the liver, and the inferior boundary is the first(superior) part of the duodenum. The omental foramen may be the site of an internal hernia if a loop of small intestine becomes entrapped there. Fluid sometimes accumulates in the omental bursa (e.g., following a perforation through the posterior wall of the stomach). Injury and inflammation of the pancreas (pancreatitis) can result in an encapsulated collection of pancreatic fluid, usually in the posterior wall of the omental bursa (pancreatic pseudocyst) (e.g., see http://www.emedicine.com/radio/topic576.htm ).
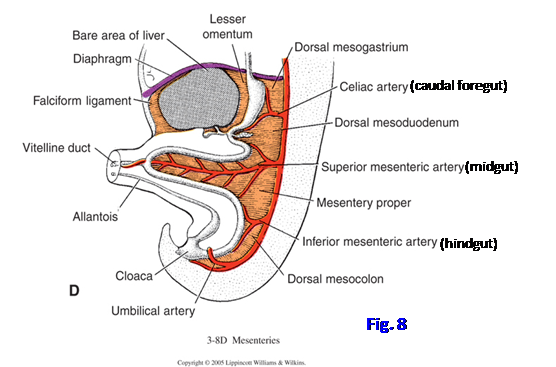
The blood supply to the abdominal portion of the gastrointestinal system from three unpaired ventral branches of the aorta reflects its embryonic origin (Fig. 8). Derivatives of the embryonic caudal foregut, which extends from the distal esophagus to the entrance of the (common) bile duct into the second, or descending, part of the duodenum, are supplied by branches of the celiac trunk (celiac artery). Midgut derivatives extend from just distal to the bile duct entrance to near the splenic (left colic) flexure and are supplied by branches of the superior mesenteric artery. The hindgut extends from just proximal to the splenic flexure to the middle of the anal canal and is supplied by branches of the inferior mesenteric artery.
Note that the abdominal aorta is a retroperitoneal structure, and so the celiac trunk, superior mesenteric artery, and inferior mesenteric artery arise in a retroperitoneal position. Some of their branches, however, enter a mesentery to supply intraperitoneal organs. The celiac trunk arises in front of vertebra Tv12, the superior mesenteric artery at the Lv1 level, and the inferior mesenteric artery at the Lv3 level. Pay particular attention to the fact that the autonomic innervation of the gastrointestinal tract follows the blood vessels that supply it. Since the general visceral afferent nerve fibers that accompany sympathetic fibers carry pain from visceral organs, knowledge of their arrangement provides a basis for understanding pain referred to the body wall (Gr 2.77, Table 2.7 [p. 169]).
The venous drainage of the abdominal portion of the gastrointestinal tract and spleen differs fundamentally from that of the rest of the body. The abdominal digestive tract is drained by the portal system of veins, which carries the nutrient-rich blood to the liver rather than directly to the systemic circulation as represented by the inferior vena cava (Gr 2.60; Ne 292). In the liver nutrients are extracted from the blood and stored, while toxins are extracted and broken down, and bile is produced for transport in the bile duct to the duodenum. The secreted bile both neutralizes acid in the chyme leaving the stomach and emulsifies fat to facilitate its digestion. Only the larger tributaries of the portal vein will be dissected.
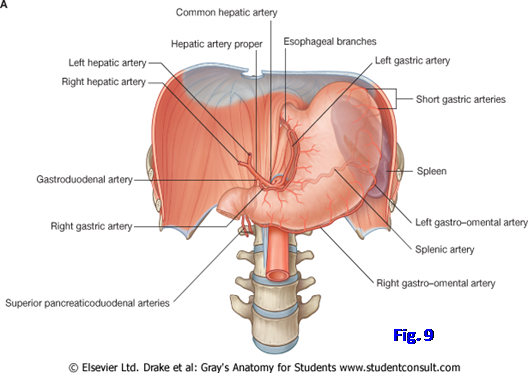
The celiac trunk (celiac artery) is the first branch of the abdominal aorta to be studied. It has three branches—the left gastric, common hepatic, and splenic arteries (Fig. 9; Gr 2.28, 2.30, 2.34; Ne 283, 284).
The left gastric artery ascends briefly toward the esophageal hiatus of the diaphragm, giving off esophageal branches before descending to the right along the lesser curvature of the stomach. It anastomoses with the right gastric artery.
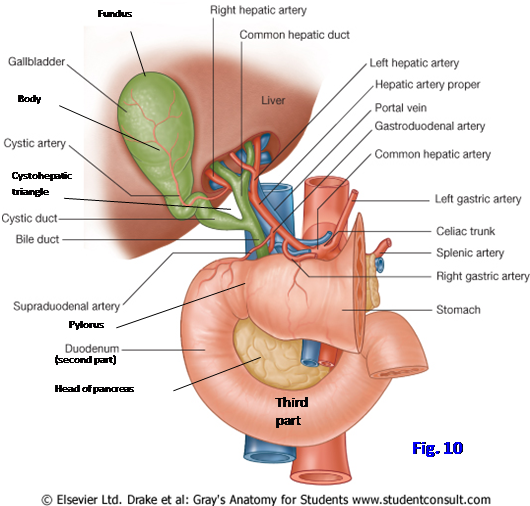
The common hepatic artery courses to the right from its origin to divide into proper hepatic and gastroduodenal arteries near the pylorus. The proper hepatic artery usually gives origin to the right gastric artery, then ascends in the hepatoduodenal ligament. It bifurcates into right and left hepatic arteries to their respective lobes of the liver. The cystic artery to the gallbladder typically arises from the right hepatic artery, but variations are common (Fig. 10; Gr 2.57; Ne 283, 284). The cystic artery crosses a triangle bounded on the left side by the common hepatic duct, on the right side by the cystic duct, and above by the liver (cystohepatic/hepatobiliary triangle). This is an important relationship during the surgical removal of the gallbladder (cholecystectomy). The triangle contains a lymph node (Calot’s node) that is enlarged during inflammation of the gallbladder (cholecystitis) or bile ducts (cholangitis).
The gastroduodenal artery descends behind the first part of the duodenum to divide into the superior pancreaticoduodenal and right gastro-omental arteries (Fig. 9; Gr 2.28, 2.33, 2.34; Ne 283, 284). In this position the gastroduodenal artery may hemorrhage due to a peptic ulcer that erodes through the posterior wall of the first part of the duodenum, the most common location for a peptic ulcer. Alternatively, a duodenal ulcer may erode inferiorly into the pancreas, producing pancreatitis, or anteriorly into the peritoneal cavity, causing peritonitis, both potentially life-threatening conditions.
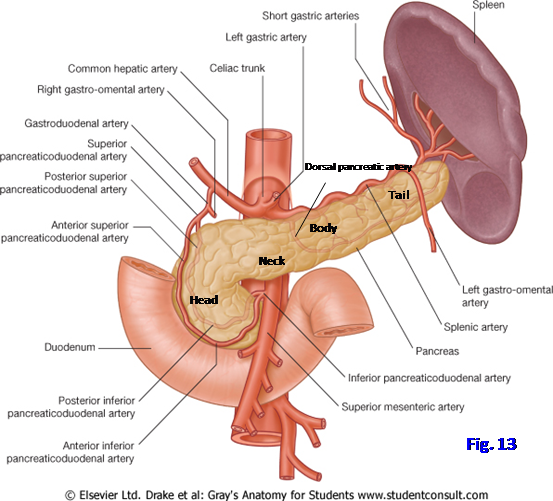
The superior pancreaticoduodenal artery divides into anterior and posterior branches that anastomose with corresponding branches of the inferior pancreaticoduodenal artery from the superior mesenteric. As the name suggests, the pancreaticoduodenal arteries supply the head of the pancreas and adjacent duodenum.
The right gastro-omental artery follows the greater curvature of the stomach within the greater omentum. It anastomoses with the left gastro-omental branch of the splenic artery.
The splenic artery is the third branch of the celiac trunk. It branches from the left side of the celiac trunk and passes posterior to the stomach along the superior border of the pancreas. In this position it may be the cause of fatal hemorrhage following the rare erosion of a peptic ulcer through the posterior wall of the stomach. Fatal hemorrhage also may result from the rupture of a splenic artery aneurysm, while an unruptured aneurysm may cause severe epigastric pain and vomiting (emesis) (e.g., see http://shortreports.rsmjournals.com/content/1/3/24.full)
Along with the tail of the pancreas, the splenic artery enters the splenorenal ligament to reach the hilum of the spleen (Fig. 9; G11 2.28, 2.32, 2.34; G12 2.29, 2.33, 2.34; N 281-284). The splenic artery gives branches to the pancreas, short gastric arteries to the fundus of the stomach, and the left gastro-omental artery to the greater curvature. Pancreatic branches regularly include a dorsal pancreatic artery given off near the origin of the splenic artery and a great pancreatic artery near the middle of the body of the pancreas (N 284, 286).
20. Study the omental foramen. Its anterior boundary is the hepatoduodenal ligament. Place your index finger into the omental foramen and your thumb anterior to the hepatoduodenal ligament and squeeze the hepatoduodenal ligament to palpate the three structures traversing it: the portal triad comprised of the bile duct, proper hepatic artery, and portal vein. Surgeons sometimes use this Pringle maneuver to compress the proper hepatic artery or portal vein to control bleeding (e.g., from a severed cystic artery).
21. Clean the celiac trunk and its branches. The lesser omentum and the parietal peritoneum in the posterior wall of the omental bursa will have to be removed piecemeal to expose the celiac trunk. Start by elevating the liver and pulling the stomach downward. Find the left and right gastric arteries in the lesser omentum along the lesser curvature of the stomach.
22. Follow the left gastric artery proximally to where it branches from the celiac trunk, looking for small esophageal branches of the left gastric artery that ascend on the distal esophagus. Expect the arteries to be enclosed in a dense plexus of autonomic nerve fibers (celiac plexus), which will have to be removed without damaging the vessels.
23. Clean the common hepatic artery, either by following it distally from the exposed celiac trunk or by following the right gastric and proper hepatic arteries proximally toward it. Examine the bifurcation of the common hepatic artery into the proper hepatic and gastroduodenal arteries.
24. Follow the proper hepatic artery through the hepatoduodenal ligament toward the liver. The artery typically lies to the left of the bile duct and anterior to the portal vein in the ligament (Fig. 10).
25. Find the division of the proper hepatic artery into right and left hepatic arteries near the transverse fissure (porta hepatis), where structures enter and leave the liver.
26. Identify the cystic artery supplying the gallbladder. It typically arises from the right hepatic artery within the cystohepatic triangle and courses to the right to reach the gallbladder. Variations are common. A discrete cystic veinmay not be present because sometimes all of the veins of the gallbladder drain directly into the liver (Gr 2.54C). Note that the cystic duct from the gallbladder joins the common hepatic duct from the liver to form the (common) bile duct (Gr 2.37, 2.54B-C; Ne 280, 284). XXX
27. Trace the gastroduodenal artery inferiorly behind the first part of the duodenum. Find its division into superior pancreaticoduodenal and right gastro-omental arteries. Approaching from the right(lateral) side, mobilize the descending (second) part of the duodenum and the head of the pancreas from the right kidney and related structures and retract them anteriorly (Gr 2.36; Ne 286).
28. Clean the anterior and posterior branches of the superior pancreaticoduodenal artery, which anastomose in front of and behind, respectively, the head of the pancreas with the corresponding branches of the inferior pancreaticoduodenal artery. These anastomoses are described as forming arches (arterial arcades). The posterior superior pancreaticoduodenal artery often branches from the gastroduodenal artery proximal to its division into anterior superior pancreaticoduodenal and right gastro-omental arteries.
29. Follow the right gastro-omental artery along the greater curvature of the stomach in the greater omentum to where it anastomoses with the left gastro-omental artery (Gr 2.28; Ne 283).
30. Cut through the greater omentum just inferior to the gastro-omental arteries and elevate the stomach and transverse colon (Gr 2.21, 2.34; Ne 264). Continue removing parietal peritoneum from the posterior wall of the omental bursa to dissect the tortuous splenic artery as it courses along the superior border of the pancreas (Gr 2.21, 2.34; Ne 281, 284). Find the short gastric and left gastro-omental branches of the splenic artery.
31. Clean the splenic vein as it passes medially posterior to the body and tail of the pancreas. It usually receives the inferior mesenteric vein as a tributary. The splenic vein unites with the superior mesenteric vein behind the neck of the pancreas to form the portal vein, which enters the hepatoduodenal ligament en route to the liver. Try to find the beginning of the portal vein. XXX
Study the organs supplied by the blood vessels just dissected. The stomach consists of a cardial portion, fundus, body, and pyloric portion (Gr 2.27; Ne 267, 268). The cardia surrounds the cardial orifice at the gastroesophageal junction. A physiologic lower esophageal sphincter, formed in part by the diaphragmatic musculature of the esophageal hiatus, prevents regurgitation into the esophagus. Chronic reflux of gastric contents into the lower esophagus may cause metaplastic change of the mucosa, ulceration, and stricture formation. This Barrett’s esophaguspredisposes to the development of esophageal adenocarcinoma.
The fundus is the dilated upper portion of the stomach below the left dome of the diaphragm and often contains gas bubbles that are apparent on a radiograph. The body forms the major portion of the stomach. It is continuous at a notch on the lesser curvature (angular incisure) with the pyloric part. The pyloric part consists of the wide pyloric antrum leading into the narrow pyloric canal. The pyloric canal ends at the pyloric orifice connecting the stomach with the duodenum. The pyloric orifice is guarded by a thickened circular layer of smooth muscle under parasympathetic control by the vagus nerves (anterior vagal trunk), the pyloric sphincter.
32. Attempt to find the anterior and posterior vagal trunks continuing from the esophagus onto the stomach (Gr 1.72, 2.76; Ne 298-300). They coalesce from the esophageal plexus of the thorax with most fibers from the left vagus nerve entering the anterior vagal trunk and most fibers from the right vagus nerve entering the posterior trunk. XXX
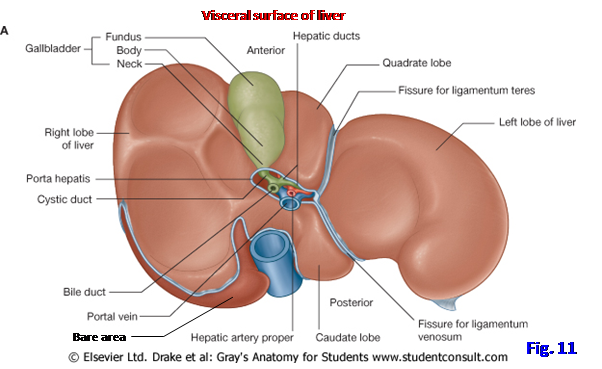
The liver is the largest gland in the body. It has diaphragmatic and visceral surfaces separated anteriorly by a sharp inferior border (Figs. 5, 11; Gr 2.22, 2.24, 2.49, 2.50A; Ne 267, 277, 278).
Posteriorly the diaphragmatic surface has a bare area where the liver isn’t covered by visceral peritoneum and is in direct contact with the diaphragm. The inferior vena cava traverses the groove for the inferior vena cava in the bare area (Fig. 11). The bare area is bordered by peritoneal reflections that suspend the liver from the diaphragm, the anterior and posterior layers of the coronary ligament. These layers meet laterally to form the right and left triangular ligaments on their respective sides of the falciform ligament.
The liver is subdivided into functional right and left lobes by a sagittal line joining the fossa for the gallbladder and the groove for the inferior vena cava. The functional right lobe of the liver is a single large lobe. The functional left lobe includes the smaller caudate and quadrate lobes medially separated from the main portion of the left lobe by the fissure for the ligamentum teres hepatis (round ligament of the liver) and the fissure for the ligamentum venosum. The caudate and quadrate lobes are separated from each other by a transverse fissure, the porta hepatis, where the portal vein, hepatic arteries, hepatic ducts, and associated lymphatic vessels and nerves enter or leave the leave (Gr 2.50, 2.55A; Ne 277, 283, 284). The large portal vein carries 75% of the blood to the liver.
Some authors consider the caudate lobe to be a separate lobe functionally distinct from the right and left lobes. The caudate lobe may have a papillary process projecting toward the porta hepatis. A caudate process extends to the right between the inferior vena cava and the porta hepatis, connecting the caudate and right lobes (Gr 2.50A).
The ligamentum teres hepatis (round ligament of the liver) is a fibrous remnant of the fetal left umbilical vein (usually just referred to as the “umbilical vein”) (Fig. 11; Gr 2.50; Ne 267, 277). The left umbilical vein carried well oxygenated blood from the placenta to the fetus before birth. The ligamentum venosum is a fibrous remnant of the fetal ductus venosus. The ductus venosus shunted much of the oxygenated blood from the left umbilical vein to the inferior vena cava, bypassing the hepatic sinusoids of the liver.
The liver is often divided for descriptive purposes into anatomical right and left lobes as well. The large anatomical right lobe is separated from the anatomical left lobe by the fissures for the ligamentum teres hepatis and ligamentum venosum. Thus, the caudate and quadrate lobes would be considered part of the anatomical right lobe of the liver.
The gallbladder is an elongated thin-walled sac occupying the gallbladder fossa on the visceral surface of the liver. The gallbladder stores and concentrates bile and is usually stained green in the cadaver. Visceral peritoneum envelops the gallbladder and helps bind it to the liver. The gallbladder consists of a fundus, body, and neck (Figs. 10, 11; Gr 2.37, 2.50, 2.58; Ne 277, 280). The fundus is the wide end of the organ that projects slightly below the inferior border of the liver. Its surface projection is near the junction of the tip of the right 9th costal cartilage and the linea semilunaris (i.e., about the midclavicular line). A patient with an inflamed gallbladder (cholecystitis), which often results from gallstones, experiences pain at this site and abruptly stops inspiration with the pressure of palpation (Murphy’s sign). Alternatively, the inflamed gallbladder may irritate diaphragmatic peritoneum, referring pain to the right shoulder. An inflamed gallbladder may adhere to the superior part of the duodenum with development of a cholecystenteric fistula. A gallstone entering the duodenum through such a fistula may pass distally and obstruct the ileocecal junction(gallstone ileus). Instead of the superior part of the duodenum, an inflamed gallbladder may adhere to the transverse colon and develop a cholecysteneric fistula with it. Would this result in gallstone ileus?
The body of the gallbladder occupies the gallbladder fossa of the liver. The neck is the tapered S-shaped portion of the gallbladder that is connected by the cystic duct to the common hepatic duct. The cystic duct is kept open by a spiral fold (spiral valve) of mucosa (Gr 2.37A; Ne 280), facilitating the passage of bile. The cystic duct joins the common hepatic duct to form the bile duct. A pouchlike dilatation of the neck of the gallbladder (Hartmann’s pouch) may develop as a pathological change and be a site of gallstone accumulation.
The gallbladder and cystic duct are supplied by the cystic artery, which usually branches from the right hepatic artery, but variations occur (Gr 2.57; Ne 283, 284). Small cystic veins directly enter the liver from the fundus and body of the gallbladder and sometimes from the neck and cystic duct. A cystic vein from the neck of the gallbladder and cystic duct rarely is a direct extrahepatic tributary of the portal vein.
33. Now carefully remove the liver. Cut any remnants of the lesser omentum and the structures entering or leaving the porta hepatis. Cut the bile duct just distal to the union of the cystic duct and common hepatic duct. Cut the falciform ligament, the anterior and posterior layers of the coronary ligament, and the right and left triangular ligaments. Cut the inferior vena cava superiorly between the liver and diaphragm. Cut the inferior vena cava inferiorly as close to the liver as possible. Lift the liver from the abdominal cavity.
34. Study the isolated liver with the attached gallbladder, identifying each of the features described in the preceding paragraphs. Identify the diaphragmatic and visceral surfaces of the liver separated by its sharp inferior border. Find the bare area of the liver, which isn’t covered by visceral peritoneum. It is outlined by the cut edges of the anterior and posterior layers of the coronary ligament, which continue laterally into the right and left triangular ligaments on those respective sides of the liver (Gr 2.49B; Ne 277). Look in the lumen of the superior part of the hepatic portion of the inferior vena cava and identify the hepatic veins, which drain blood from the liver into the systemic circulation.
35. On the visceral surface of the liver find the fossa for the gallbladder and the groove for the inferior vena cava. An imaginary sagittal line joining the two fossae indicates the division of the liver into functional right and left lobes. Find a second sagittal line formed by the fissure for the ligamentum teres hepatis and the fissure for the ligamentum venosum, which subdivides the functional left lobe. Clean the ligamentum teres hepatis, a remnant of the fetal left umbilical vein. Verify that it is a fibrous cord enclosed within the inferior free margin of the falciform ligament. Bluntly dissect into the fissure for the ligamentum venosum to find the ligamentum venosum, a fibrous cord that is a remnant of the fetal ductus venosus.
36. The transversely oriented porta hepatis connects the two sagittal lines described in the previous paragraph and separates the quadrate and caudate lobes. The quadrate and caudate lobes are part of the functional left lobe, although some authors classify the caudate lobe as a functionally distinct lobe. Identify the right and left branches of the portal vein, right and left hepatic arteries, and right and left hepatic ducts at the porta hepatis.
37. Identify the fundus, body, and neck of the gallbladder if it wasn’t surgically removed. Palpate the gallbladder to check for the presence of gallstones, which may have been asymptomatic. Follow the cystic duct to its union with the common hepatic duct to form the (common) bile duct. Clean the small cystic artery and trace it to its origin, usually from the right hepatic artery. The cystic artery usually arises in the surgically important cystohepatic triangle formed by the cystic duct, common hepatic duct, and the liver (Fig. 10). Check to see if there is a cystic vein draining into the portal vein below the liver. XXX
The large superior mesenteric artery and vein emerge from behind the neck of the pancreas to cross anterior to the uncinate process of the pancreas and the inferior (3rd) part of the duodenum to enter the mesentery (Fig. 13; Gr 2.25, 2.33, 2.34, 2.43, 2.44; Ne 284, 288, 323). In rare patients the superior mesenteric vessels may compress the duodenum, obstructing the passage of intestinal contents (superior mesenteric syndrome). The superior mesenteric artery is also a common site for acute mesenteric ischemia produced by an thromboembolus dislodged from the heart or by sudden occlusion at a focus of long-standing atherosclerosis (e.g., seehttp://emedicine.medscape.com/article/758674-overview )
The superior mesenteric artery gives off the inferior pancreaticoduodenal artery and jejunal and ileal branches to the small intestine (Figs. 12, 13). It supplies the large intestine via middle colic, right colic, and ileocolic branches. The ileocolic artery also contributes to the blood supply of the terminal ileum.
The middle colic artery arises from the right side of the superior mesenteric artery just distal to the pancreas and enters the transverse mesocolon. Near the wall of the transverse colon it divides into right and left branches (Gr 2.43, 2.44A, 2.45; Ne 287, 288).
The next branch of the superior mesenteric artery is the right colic artery, which has a variable origin. It may arise from the superior mesenteric artery or from a common stem with the ileocolic artery. The right colic artery passes to the right side in a retroperitoneal position and divides into ascending and descending branches to supply the ascending colon.
The ileocolic artery descends toward the ileocecal junction (Gr 2.43, 2.44A; Ne 287, 288). It has ascending colic, cecal, and ileal branches. The appendicular artery also commonly branches directly from the ileocolic artery. The appendicular artery is anend artery(i.e., it doesn’t have anastomoses). Consequently, if acute infection and inflammation of the appendix (acute appendicitis) results in edema compressing the artery or in the artery’s thrombosis, then necrosis and perforation of the appendix may result. A potentially fatal generalized peritonitis may be prevented if the greater omentum walls off the site of infection, producing a localized abscess.
38. Clean the superior mesenteric artery and its branches. They are enclosed within a dense superior mesenteric plexus of autonomic nerve fibers (i.e., sympathetic, parasympathetic, and visceral afferent fibers). Find the small inferior pancreaticoduodenal artery that branches from its right side as the superior mesenteric artery emerges from behind the pancreas (Ne 286, 287). The inferior pancreaticoduodenal artery divides into anterior and posterior branches that anastomose, forming arcades, with the corresponding branches of the superior pancreaticoduodenal artery. Continuing into the mesentery, dissect examples of the 12-16 jejunal and ileal arteries that branch from the left side of the superior mesenteric. Their arterial arcades and vasa recta were studied earlier.
39. Clean the middle colic, right colic, and ileocolic arteries and identify their branches. Pay attention to the appendicular artery.
40. Now study the bile passages, the duodenum, and the pancreas. The origin of the (common) bile duct by the union of the cystic duct and common hepatic duct has already been seen. Follow the bile duct inferiorly behind the head of the pancreas, which was mobilized earlier. Usually the bile duct occupies a groove on the posterior surface of the pancreas, but it may be completely embedded within pancreatic tissue.
41. Carefully clean the bile duct down to where it joins the fragile main pancreatic duct to form a dilatation, the hepatopancreatic ampulla, which opens near the middle of the second part of the duodenum at the major duodenal papilla (Gr 2.37). Note that the major duodenal papilla is the only one of these structures visible from the lumen if the duodenum is cut open. Unless it is sectioned, the hepatopancreatic ampulla can only be seen as it is formed by the union of the bile and main pancreatic ducts before it begins to penetrate the wall of the duodenum (Gr 2.37A). XXX
A circular smooth muscle sphincter at the hepatopancreatic ampulla (hepatopancreatic sphincter [of Oddi]) controls the entrance of secretions into the lumen of the duodenum. In addition, the bile duct and main pancreatic duct may have their own smooth muscle sphincters. A gallstone that has traversed the cystic and bile ducts may become impacted in the hepatopancreatic ampulla, causing the reflux of bile into the pancreas with the development of pancreatitis. A tumor in the hepatopancreatic ampulla may have the same result. A second smaller accessory pancreatic duct opens at the minor duodenal papilla above the major papilla (Gr 2.37).
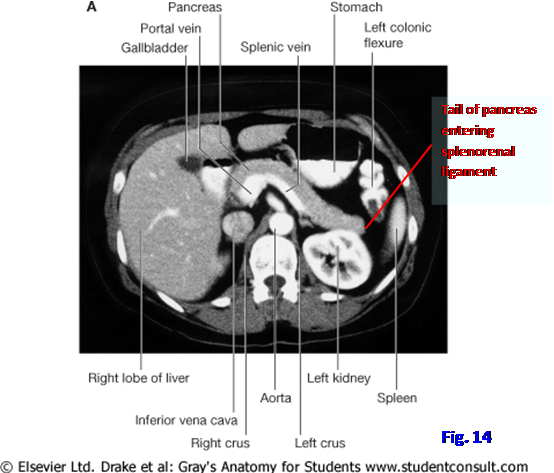
The pancreas is a combination exocrine and endocrine gland. Its exocrine secretions enter the duodenum through the main and accessory pancreatic ducts. Its endocrine secretions enter the blood. The pancreas is divided for descriptive purposes into a head, neck, body, and tail (Figs. 10, 13; Gr 2.32, 2.33; Ne 281). The head of the pancreas occupies the C-shaped curvature of the duodenum. The uncinate process is a projection from the inferior part of the head that passes to the left posterior to the superior mesenteric vessels. The neck of the pancreas lies anterior to the superior mesenteric artery. The superior mesenteric vein joins the splenic vein behind the neck to form the portal vein. The body of the pancreas continues to the left from the neck and ends in the tail. The tail of the pancreas occupies the splenorenal ligament with the splenic vessels (Fig. 14) and is in danger during removal of the spleen (splenectomy).
Pancreatic cancer is the fourth leading cause of cancer deaths with a five-year survival rate of less than 5% (see http://emedicine.medscape.com/article/280605-overview ). Adenocarcinoma of the head of the pancreas may cause extrahepatic obstruction of the bile duct. Excess bile is absorbed into the blood, producing yellowing of mucous membranes, conjunctiva, and skin (obstructivejaundice). Painless jaundice is often the first indication of cancer involving the head of the pancreas. Pancreatic cancer involving the body and tail commonly causes severe abdominal pain that radiates to the back. New-onset diabetes mellitus or hyperglycemia in individuals over the age of 50 without a family history may be the first indication of pancreatic cancer.
The duodenum is the first part of the small intestine (Figs. 10, 13; Gr 2.32, 2.33, 2.37; Ne 270, 271, 281). It begins at the pylorus and ends at the dudodenojejunal junction, where the duodenum is continuous with the jejunum. The duodenum is divided into four parts. The superior (first) part, which is approximately 5 cm long, has an initial short segment (2 cm) that is intraperitoneal. This intraperitoneal part has the greater omentum attached to its lower margin and has its upper margin connected to the liver by the hepatoduodenal ligament. This intraperitoneal part of the duodoenum has a distinct appearance on radiographs using contrast medium and is called the duodenal cap (ampulla) (Gr 2.31B-D). The remainder of the duodenum is secondarily retroperitoneal.
The descending (second) part of the duodenum near its midpoint receives the openings of the bile duct and main pancreatic duct at the major duodenal papilla (Gr 2.37; Ne 271). Usually these ducts unite to form the hepatopancreatic ampulla. The accessory pancreatic duct enters the duodenum a little higher at the minor duodenal papilla. However, there is occasional variation in these ducts (Gr 2.38 D-G).
The inferior (third or horizontal) part of the duodenum runs transversely toward the left over the inferior vena cava and aorta at the level of the 3rd lumbar vertebra. The superior mesenteric artery and vein pass anterior to the third part of the duodenum (Fig. 13; Gr 2.83G, 2.85 B-C).
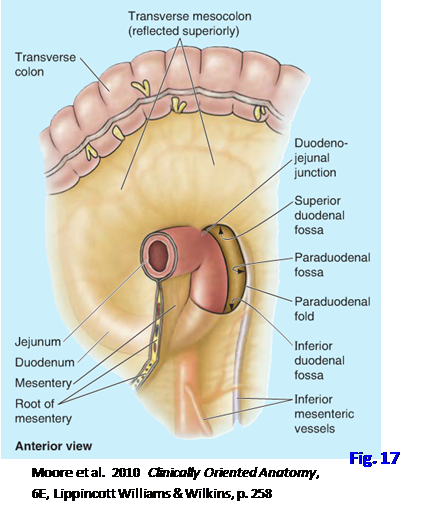
The ascending (fourth) part of the duodenum passes superiorly and to the left to join the jejunum at the duodenojejunal junction (duodenojejunal flexure) (Gr 2.32, 2.47; Ne 262). The duodenojejunal junction is supported by a fibromuscular slip of tissue, the suspensory muscle of the duodenum (ligament of Treitz), which is a surgical landmark. The duodenojejunal junction is where the small intestine again becomes intraperitoneal. It is also the demarcation between upper and lower GI bleeding, which have different clinical characteristics.
42. Study the pancreas and duodenum. Identify the parts of each. Verify that the head of the pancreas occupies the C-shaped curvature of the duodenum. Identify the uncinate process of the pancreas projecting to the left posterior to the superior mesenteric artery and vein. Note the relationship of the neck of the pancreas to the superior mesenteric artery and the origin of the portal vein in the union of the superior mesenteric and splenic veins. Identify the body and tail of the pancreas and note that the latter enters the splenorenal ligament with the splenic blood vessels. Try to dissect the delicate major pancreatic duct via a posterior approach.
43. Identify the four parts of the duodenum. Locate the duodenal cap (Gr 2.31B-D; Ne 271). It is the first 2 cm of the superior part of the duodenum and is the only intraperitoneal part of the duodenum. The hepatopancreatic ampulla was identified earlier entering the middle of the descending part of the duodenum. Verify that the superior mesenteric artery and vein pass anterior to the inferior (horizontal, third) part of the duodenum. Look for the suspensory muscle of the duodenum at the duodenojejunal flexure, where the ascending part of the duodenum joins the jejunum. This is where the small intestine again becomes intraperitoneal. XXX
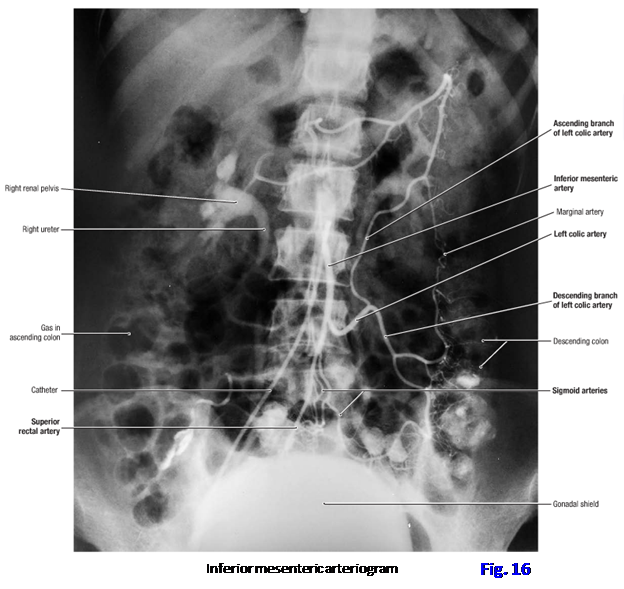
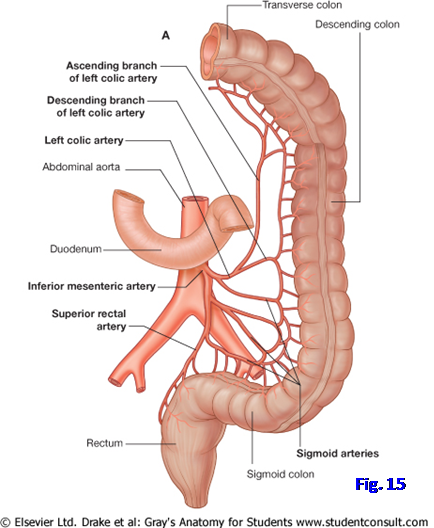
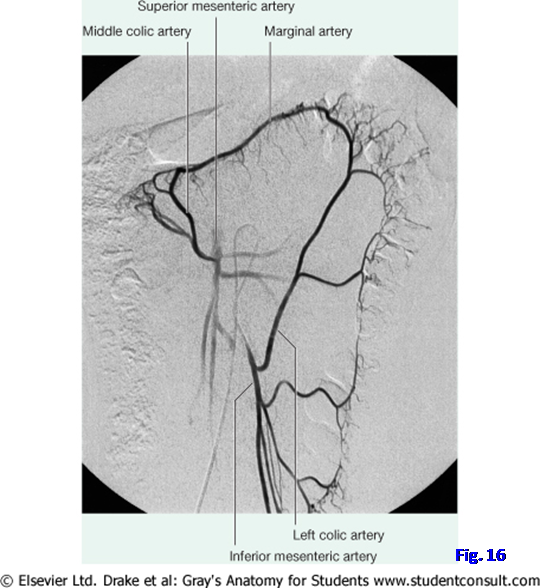
The inferior mesenteric artery sends a left colic branch to the descending colon and sigmoid branches to the sigmoid colon. It terminates as the superior rectal artery to the rectum and upper half of the anal canal (Figs. 15, 16; Gr 2.45, 2.46; Ne 288).
The left colic artery passes to the left behind the peritoneum and divides into ascending and descending branches.The ascending branch anastomoses with the left branch of the middle colic artery from the superior mesenteric, helping to form a marginal arterythat extends from the ileocecal junction to the sigmoid colon. This is important during the atherosclerotic occlusion or surgical ligation of the inferior mesenteric artery.
The descending branch of the left colic artery anastomoses with its sigmoid branches that enter the sigmoid mesocolon to supply the sigmoid colon (Fig. 15; Gr 2.45, 2.46; Ne 288, 378). The direct continuation of the inferior mesenteric artery is the superior rectal artery. It descends into the pelvis and anastomoses with the middle rectal arteries from the right and left internal iliac arteries. These arteries will be studied during dissection of the pelvis.
44. Displace loops of jejunum and ileum to the right and clean the inferior mesenteric artery and its left colic, sigmoid, and superior rectal branches. The inferior mesenteric nerve plexus in which the arteries are enclosed will have to be carefully removed. Clean the inferior mesenteric vein as it ascends retroperitoneally to join the splenic vein (Gr 2.60; Ne 291). In some bodies the inferior mesenteric vein may empty into the superior mesenteric vein instead of the splenic vein. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.