Posterior Abdominal Wall and Kidneys
Please note that for this lab:
- -Only EVEN numbered tables will remove the GI tract.
- -ODD numbered tables will leave the GI tract in the body.
In order to study retroperitoneal organs, the posterior abdominal wall, and the diaphragm, the abdominal portion of the gastrointestinal tract will be removed from all cadavers. Please follow the instructions exactly.
Strings will be tied around the distal esophagus and the distal sigmoid colon to minimize the spillage of their contents when they are cut. Next the three major arteries to the abdominal GI tract—celiac trunk, superior mesenteric artery, inferior mesenteric artery—will be cut close to their origins from the abdominal aorta. The abdominal gastrointestinal tract will then be freed of all attachments to the body wall and removed from the body.
1. Tie a string around the distal esophagus just above the gastroesophageal junction. Cut the esophagus just superior to the string.
2. Mobilize the sigmoid colon. It is continuous with the rectum in front of the third sacral vertebra (G11 2.26, 2.41A, 3.7A, 3.8; G12 2.37A, 3.14A, 3.19). Carefully milk any contents of the distal sigmoid colon proximally by gentle squeezing. Tie two strings 4 cm apart around the sigmoid colon at the level of the sacral promontory (anterior projecting edge on the body of the first sacral vertebra) (G11 3.2A, 3.7A; G12 3.3A, 3.14A), which is part of the pelvic brim at the boundary between the abdominal cavity and the pelvic cavity. The sacral promontory is easily recognizable because the sacrum, which has a concave anterior surface, angles posteriorly on the lumbar vertebral column. Cut the sigmoid colon between the two strings.
3. Review the celiac trunk, superior mesenteric artery, and inferior mesenteric artery and their distributions to abdominal organs. Cut each artery approximately 1 cm from the abdominal aorta, leaving a stump for reference.
4. The gastrointestinal tract between the cut ends must be freed of mesenteries and other attachments. Remove any peritoneal attachments to the posterior abdominal wall from the stomach. If it wasn’t done previously, approach from the right side to mobilize the duodenum and head of the pancreas, inserting your fingers behind the duodenum and pancreas and pulling them forward. Again identify the suspensory muscle of the duodenum (ligament of Treitz) and cut it close to the duodenojejunal flexure. Continue until the entire duodenum and pancreas are free of the posterior body wall.
5. From the left side pull the spleen and tail of the pancreas medially toward the mobilized duodenum. Cut the splenorenal ligament to free the spleen from the posterior body wall.
6. The superior mesenteric artery has already been cut. Now cut the remnants of the root of the mesentery from its line of attachment on the posterior abdominal wall between the duodenojejunal flexure and the ileocecal junction.
7. Using blunt dissection, mobilize the descending colon along its left (lateral) border (i.e., in the left paracolic gutter). Displace the descending colon medially to expose the left kidney and posterior abdominal wall. In order to expose the right kidney, mobilize the ascending colon by bluntly dissecting the peritoneum along its right (lateral) border (i.e., in the right paracolic gutter). Displace the ascending colon medially. If any of the transverse mesocolon is intact, cut it to free the transverse colon. The gastrointestinal tract and spleen should now be free of attachments between the cuts in the esophagus and the sigmoid colon. Carefully remove the mobilized GI tract and spleen and place them in the large plastic bag provided. Wet the removed tissue down before closing the bag. XXX
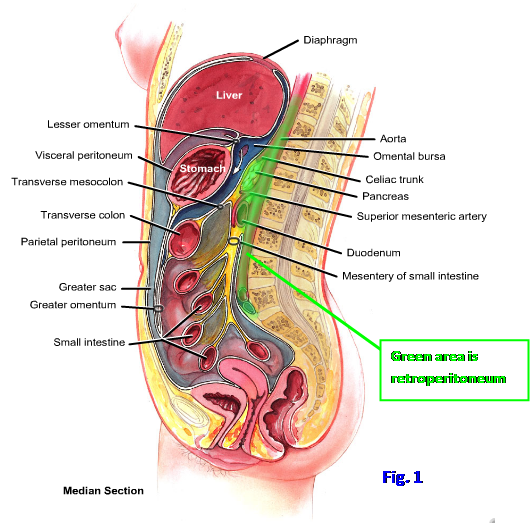
Several organs and the largest amount of connective tissue within the abdominal cavity are located posterior to the peritoneal sac in a region termed the retroperitoneum (Fig. 1). In addition to the secondarily retroperitoneal portions of the gastrointestinal tract previously studied (most of the duodenum and pancreas, ascending colon, and descending colon), the retroperitoneum includes primarily retroperitoneal organs, such as the kidneys and ureters, suprarenal glands, abdominal aorta, and inferior vena cava. These primarily retroperitoneal organs never invaginated the peritoneal sac and were never suspended by a mesentery during embryonic development.
The kidneys and ureters, suprarenal glands, and associated structures will be studied first. The kidneys are paired organs that excrete excess water and metabolic waste products and perform important homeostatic functions for the body. The urine they produce is carried by the ureters to the urinary bladder within the pelvis.
The kidneys are located on the posterior abdominal wall from the T12 to L3 vertebral levels, with the right kidney slightly lower than the left due to the size of the liver (G11 2.62, 2.63; G12 2.62, 2.63; N 308-310, 316). The right kidney is separated from the liver by a clinically important space within the peritoneal cavity, the hepatorenal recess.
The kidneys are retroperitoneal organs and are embedded within fat (G11 2.71; G12 2.71; N 317). The extraperitoneal fat immediately around the kidneys and suprarenal glands is perirenal (perinephric) fat. The kidneys, suprarenal glands, and perirenal fat are enclosed by a membranous layer, the renal fascia, except for an inferior opening around the ureter. External to the renal fascia is pararenal (paranephric) fat. The renal fascia presents a barrier to the spread of infection, except in an inferior direction, where a perinephric infection may spread along the ureter to reach the pelvis. The lack of inferior support by the renal fascia also means that an abnormally mobile kidney may descend more than usual when the body is erect (nephroptosis, or dropped kidney), most commonly in young, thin white females. The resulting intermittent pain from traction on renal vessels and kinking of the proximal ureter is relieved by lying down (see http://emedicine.medscape.com/article/1458935-overview#showall ).
Each kidney is a bean-shaped structure with a medial hilum where structures enter and leave (Fig. 2; G11 2.65-2.67; G12 2.66-2.67; N 311, 312). The renal hilum opens into a depression within the medial side of the kidney, the renal sinus. At the hilum the most anterior structure usually is the renal vein, which drains into the inferior vena cava. The left renal vein differs from the right renal vein in that it receives the left testicular or ovarian vein and the left suprarenal vein as tributaries (G11 2.62B, 2.63A; G12 2.62B, 2.63A; N 308, 310) and also has connections with the ascending lumbar and upper lumbar veins. These connections are clinically significant because they may allow the left renal vein to be ligated near the midline without obstructing venous drainage from the kidney (e.g., venous blood in the ligated left renal vein may drain through the ascending lumbar vein into the azygos system). The left renal vein passes toward the right between the superior mesenteric artery and aorta (G11 2.63; G12 2.63; N 310) and, rarely, may be compressed there (e.g., by an aneurysm of one vessel or the other) in renal vein entrapment syndrome (nutcracker syndrome), resulting in hematuria and left flank pain (e.g., see http://www.actasurologicas.info/v33/n01/ENG/3301NC04.htm ).
Behind the renal vein is the renal artery, which is a branch of the abdominal aorta. One or more accessory renal arteries commonly branch from the aorta, and an extrahilar artery entering the kidney near the inferior pole may compress and obstruct the renal pelvis or ureter. Each of the five segments of the kidney—superior, anterior superior, anterior inferior, inferior, and posterior—typically receives only one segmental artery. That is important because renal segmental arteries are end arterieswith no significant anastomoses(G11 2.66D, 2.67; G12 2.67; N312). On the positive side, each segment of the kidney is surgically resectable, but on the negative side each segment is subject to tissue death and necrosis if its artery is compromised.
The most posterior structure at the hilum is the renal pelvis, which is the funnel-shaped upper end of the ureter.8. Remove any remaining parietal peritoneum overlying the kidneys. Study the pararenal fat around the kidneys and suprarenal glands. Bluntly dissect the fat to demonstrate the membranous renal fascia. It is variably developed and may be difficult to identify in some cadavers. Remove the renal fascia enclosing the perirenal fat adjacent to the kidney and suprarenal gland. Clean away perirenal fat to expose the kidneys and renal vessels.
9. Clean the right and left renal arteries and veins and note whether there are accessory renal arteries present. If so, where do the accessory renal arteries arise? If an accessory renal artery goes to the inferior pole of the kidney in this cadaver, is it in a position to compress the ureter? Verify that the left renal vein passes between the superior mesenteric artery and the aorta en route to the inferior vena cava. Realize that the vein rarely may be compressed there (renal vein entrapment syndrome), just as the inferior part of the duodenum may be compressed between the superior mesenteric artery and the aorta (superior mesenteric artery syndrome) (G11 2.63B; G12 2.63B).
10. ONE KIDNEY is going to be mobilized by cutting its blood vessels, and the kidney and attached ureter on that side will be moved into the pelvis. On EVEN-NUMBERED TABLES mobilize the RIGHT kidney and ureter and reflect them down into the pelvis. On ODD-NUMBERED TABLES mobilize the LEFT kidney and ureter and reflect them down into the pelvis. XXX
Each kidney is enclosed within a fibrous renal capsule and consists of an outer renal cortex and an inner renal medulla (G11 2.65A, 2.66C; G12 2.66A, 2.67B; N 311). The medulla is formed by the renal pyramids. The pyramids are separated by inward penetrations of cortical tissue, the renal columns. Each pyramid ends in a rounded apex known as a renal papilla. Each papilla drains into a tubular minor calyx. Two or three minor calyces join to form a major calyx, and two or three major calyces join to form the renal pelvis. The structures that transport urine are well demonstrated on x-rays when they contain radiopaque material (pyelogram) (G11 2.66B; G12 2.65B).
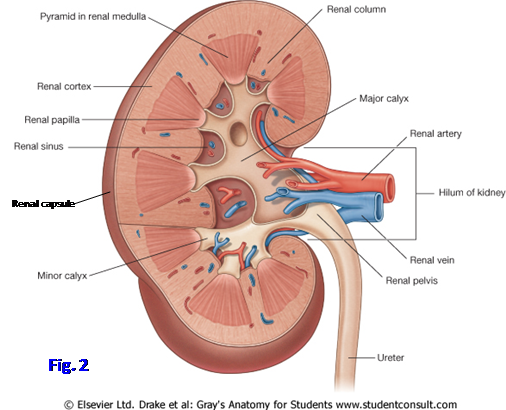
11. On the mobilized kidney, clean and identify the structures at the renal hilum. Bisect the mobilized kidney longitudinally in the coronal plane and study its internal structure (Fig. 2; G11 2.65C, 2.66A; G12 2.66C, 2.66D; N 311).
12. Identify the renal cortex and renal pyramids. Study a renal papilla draining into a minor calyx. Follow two or three minor calyces until they join to form a major calyx. Find the union of the major calyces to form the renal pelvis. XXX
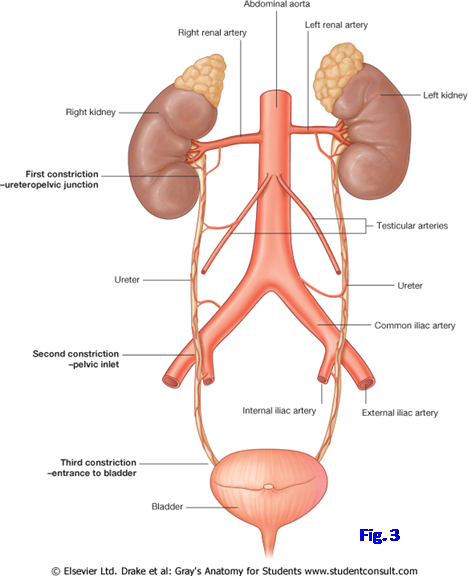
The ureter is a long, narrow, muscular tube that descends retroperitoneally from the renal pelvis to the urinary bladder (G11 2.63; G12 2.63, N 308, 316). The ureter crosses the pelvic brim near the bifurcation of the common iliac arteries. This is one of three normal sites of constriction of the ureter that predispose it to obstruction during the passage of a kidney stone (Fig. 3). The other two sites of constriction are at the junction of the renal pelvis and ureter (ureteropelvic junction) and at the ureter’s passage through the wall of the bladder.
The afferent nerve supply to the ureter is via GVA fibers accompanying sympathetic preganglionic fibers to spinal cord segments T11-L2; therefore, pain is referred to the corresponding dermatomes, usually in a loin-to-groin pattern during passage of a kidney stone.
The blood supply of the abdominal portion of the ureter is from small branches of the renal artery, gonadal artery, abdominal aorta, and common iliac artery (Fig. 3; N316).
The suprarenal (adrenal) glands are endocrine glands that are essential for life. They are located superomedially on the kidneys and are enclosed by perirenal fat and renal fascia (G11 2.63A, 2.64A; G12 2.63A, 2.64A; N 308, 310). The renal fascia forms a thin septum between the gland and the kidney, so that a suprarenal gland can be spared during surgical removal of a kidney (nephrectomy). The embalmed suprarenal gland of the cadaver tends to be friable and may resemble fat.
Each suprarenal gland receives arteries from three sources (G12 2.65C; N 310, 322). The superior suprarenal arteries are several small branches from the inferior phrenic artery. The middle suprarenal artery branches directly from the abdominal aorta. The inferior suprarenal artery (or arteries) arises from the renal artery. In contrast, there typically is a single suprarenal vein on each side. The right suprarenal vein drains into the inferior vena cava, and the left suprarenal vein drains into the left renal vein.13. Clean the ureters and attempt to find some of the small arteries that supply them. Realize that the ureter basically is supplied by nearby arteries as it descends toward the urinary bladder. Pay attention to sites of constriction of the ureters—at the ureteropelvic junction, pelvic brim, and passage through the wall of the urinary bladder. These are potential sites of obstruction by ureteric stones.
14. Find and clean the suprarenal glands. Dissect the superior, middle, and inferior suprarenal arteries and the single suprarenal vein. Verify that the right suprarenal vein drains into the inferior vena cava, but the left suprarenal vein drains into the left renal vein. What are other differences in the tributaries of the left and right renal veins? XXX
Most of the arteries supplying abdominal organs branch from the abdominal aorta (G11 2.63, 2.75, 2.82C; G12 2.63, 2.75; N 308, 316). It begins as the continuation of the thoracic aorta at the aortic hiatus of the diaphragm at the level of vertebra T12 and ends in front of the L4 vertebra by dividing into the right and left common iliac arteries. The aorta descends to the left of the inferior vena cava.
In children and thin adults (but probably not robust 50-year-old anatomy professors) the lower abdominal aorta can be compressed against the body of Lv4 by pressure on the anterior abdominal wall over the umbilicus to control bleeding in the pelvis or lower limbs. The abdominal aorta below the level of the renal arteries is frequently the site of an abdominal aortic aneurysm (e.g., see http://www.emedicine.com/med/topic3443.htm ). Its presence may first be indicated in thin individuals by pulsations of the relaxed anterior abdominal wall when the patient is lying supine. Although surgical repair of an aneurysm with a prosthetic graft—the wall of the aorta is sewn back over the graft to prevent development of an aorticoenteric fistula—is often possible, the inferior mesenteric artery usually arises from the involved area. Therefore, the viability of the hindgut depends on the patency of the marginal artery or replantation of the inferior mesenteric artery into the aortic graft. Endovascular aneurysm repair is a newer approach that doesn’t require the large abdominal incision of conventional surgery.
The branches of the abdominal aorta (G11 2.75A, 2.82C; G12 2.75A; N 257, 308, 316) may be classified as unpaired visceral branches, paired visceral branches, or paired parietal branches. The three large, unpaired visceral branches to the alimentary tract—celiac trunk, superior mesenteric artery, and inferior mesenteric artery—have already been studied arising from the anterior aspect of the aorta.
Paired visceral branches to abdominal (or originally abdominal) organs come off the abdominal aorta laterally—the renal, suprarenal, and testicular or ovarian arteries. Paired parietal branches also come off the aorta laterally to supply the posterior abdominal wall and diaphragm—inferior phrenic, subcostal, and lumbar arteries (G11 2.75A; G12 2.75A; N 257). The lumbar arteries are in series with the posterior intercostal and subcostal arteries. A small unpaired parietal branch, the median sacral artery, branches from the posterior aspect of the aortic bifurcation and descends in the midline over the sacral promontory.
The inferior vena cava returns venous blood from below the diaphragm to the right atrium. It is formed over the right side of the fifth lumbar vertebra by the union of the two common iliac veins (G11 2.63, 2.75B; G12 2.63, 2.75B; N 258, 308). It ascends on the right side of the abdominal aorta and inclines anteriorly to enter the thorax through vena caval foramen at the level of vertebra T8. The tributaries of the inferior vena cava mostly correspond to branches of the abdominal aorta, except for veins from the gastrointestinal tract, which drain into the portal vein. The left testicular or ovarian vein drains into the left renal vein instead of the inferior vena cava, as does the left suprarenal vein. Often the left inferior phrenic vein joins the left suprarenal vein (N 310).
15. Identify the paired visceral and paired parietal branches of the abdominal aorta. The renal and suprarenal arteries have already been studied. Find the small testicular or ovarian arteries branching from the anterior surface of the abdominal aorta just inferior to the renal arteries. Each testicular artery descends retroperitoneally toward the deep inguinal ring, where it becomes a component of the spermatic cord. The ovarian artery descends retroperitoneally with its inferior part raising a peritoneal fold, the suspensory ligament of the ovary, to reach the ovary within the pelvis.
16. The inferior phrenic arteries typically arise from the front of the abdominal aorta between the aortic hiatus of the diaphragm and the celiac trunk, but variations are common. As they ascend to the diaphragm, they give off several small superior suprarenal arteries, as was seen previously. Note four paired segmental lumbar arteries arising posterolaterally from the abdominal aorta (N257). These correspond to posterior intercostal arteries in the thoracic region. Look for the median sacral artery descending from behind the aortic bifurcation across the sacral promontory in the midline.
17. Identify and clean the major tributaries of the inferior vena cava. XXX
The autonomic innervation of the abdominal viscera is by both sympathetic and parasympathetic nerves, which join to form perivascular nerve plexuses on the abdominal aorta and its branches (G11 2.76; G12 2.76; N 297, 301, 302). The sympathetic fibers cause vasoconstriction of blood vessels, inhibit peristalsis, and inhibit glandular secretion in the digestive tract. Parasympathetic fibers increase peristalsis and glandular secretion. The autonomic effects on peristalsis and glandular secretion are mediated through the enteric nervous system, an elaborate network of neurons intrinsic to the wall of the gut.
Details of abdominal autonomic descriptions vary from reference to reference, but in general (Fig. 4) preganglionic sympathetic innervation to adult derivatives of the embryonic foregut is by the greater thoracic splanchnic nerves (T5-9), to the midgut by the greater (T8-9 fibers) and lesser (T10-11) thoracic splanchnic nerves, and to the hindgut by the lumbar splanchnic nerves (L1-L2/3).
The cell bodies of postganglionic sympathetic neurons supplying the abdominal gastrointestinal tract are located within prevertebral ganglia located along the abdominal aorta at the origin of branches to viscera. The main prevertebral ganglia are the celiac, superior mesenteric, aorticorenal, and inferior mesenteric ganglia (Fig. 4). The axons of preganglionic fibers in the greater thoracic splanchnic nerves synapse on cell bodies within the celiac ganglia. From the celiac ganglia the axons of postganglionic neurons follow branches of the celiac trunk to foregut derivatives, including the liver, gallbladder, and pancreas, as part of the celiac plexus. They also supply the spleen.
The axons of preganglionic fibers in the lesser splanchnic nerves and T8-9 fibers of the greater splanchnic nerves synapse on postganglionic sympathetic neurons cell bodies within the superior mesenteric ganglion. The axons of the postganglionic neurons follow branches of the superior mesenteric artery to midgut derivatives (i.e., the segment of the GI tract from the middle of the descending part of the duodenum to near the left colic flexure) as part of the superior mesenteric plexus.
The lumbar splanchnic nerves send preganglionic axons from L1-2 (sometimes L1-3) to the inferior mesenteric ganglion at the base of the inferior mesenteric artery. This ganglion is usually small and may be difficult to identify. Postganglionic fibers follow the branches of the artery to derivatives of the embryonic hindgut as part of the inferior mesenteric plexus.
The other major prevertebral ganglia are the aorticorenal ganglia with one located at the origin of each renal artery. They receive preganglionic sympathetic fibers from the lesser and least splanchnic nerves and send postganglionic axons to the kidneys and suprarenal glands. Direct preganglionic sympathetic nerve fibers also travel to the suprarenal medulla, which functions like a collection of postganglionic sympathetic neurons but secretes catecholamines (mainly epinephrine) into the blood.
The postganglionic sympathetic fibers from prevertebral ganglia join preganglionic parasympathetic fibers to be distributed to viscera in perivascular nerve plexuses (G11 2.76; G12 2.76; N 300, 303). Preganglionic parasympathetic nerves supplying abdominal viscera come from the vagus (CN X) nerves and the pelvic splanchnic nerves. Fibers of the vagus nerves enter the abdomen through the esophageal hiatus of the diaphragm as the anterior and posterior vagal trunks. These preganglionic fibers of the vagus nerves help form the aortic plexus of nerves and are distributed to the abdominal portions of the digestive tract that develop from the embryonic foregut and midgut (i.e., to near the left colic flexure). The cell bodies of postganglionic parasympathetic neurons are located either within the wall of the digestive tube (myenteric and submucosal plexuses) or very close to it.
One important function of the vagal nerve fibers that is often overlooked is relaxation of the pyloric sphincter to allow chyme to enter the duodenum from the stomach. When the vagus nerves are surgically sectioned (vagotomy) to control gastric acid secretion in patients with peptic ulcers that don’t respond to medical therapy, an effort is made to spare the branches to the pylorus (selective vagotomy). Otherwise, a pyloroplasty or bypass surgery may have to be performed (e.g., gastrojejunostomy) (e.g., see http://emedicine.medscape.com/article/197643-treatment ).
The preganglionic parasympathetic fibers in the pelvic splanchnic nerves originate from cell bodies in spinal cord segments S2-4. These preganglionic fibers join the inferior hypogastric plexuses in the pelvis before ascending through hypogastric nerves into the abdomen. They supply derivatives of the embryonic hindgut (i.e., the part of the digestive tract from just proximal to the left colic flexure to the middle of the anal canal).
Sympathetic and parasympathetic (GVE) nerve fibers are accompanied by general visceral afferent (GVA) fibers. The GVA fibers accompanying sympathetic fibers are responsible for pain referred from thoracic and abdominal viscera to the body wall. Therefore, by understanding the source of preganglionic sympathetic nerve fibers supplying an organ, one can predict the dermatomes to which its pathology will refer pain. For example, disease or injury within the distribution of the celiac trunk will refer pain to dermatomes T5-9 because the preganglionic sympathetic fibers to foregut derivatives arise from those spinal cord levels (greater splanchnic nerve). In general pain from the abdominal foregut is referred to the epigastric region, from the midgut to the umbilical region, and from the hindgut to the pubic (hypogastric) region.
The GVA fibers that accompany parasympathetic nerve fibers to thoracic and abdominal viscera are mainly involved in visceral reflex functions.18. Identify the prevertebral ganglia and aortic plexus. Look for the paired celiac ganglia, one on either side of the celiac trunk. Attempt to find the superior mesenteric ganglion (or ganglia) at the root of the superior mesenteric artery. The celiac and superior mesenteric ganglia may be fused. A small inferior mesenteric ganglion may or may not be visible at the root of the inferior mesenteric artery. Appreciate that the celiac, superior mesenteric, and inferior mesenteric plexuses are interconnected and all contain sympathetic, parasympathetic, and general visceral afferent nerve fibers. XXX
The posterior abdominal wall is formed by muscles and fascia behind the kidneys, inferior to the diaphragm. First, the diaphragm will be studied and then the posterior abdominal muscles and associated nerves and blood vessels will be dissected.
The respiratory diaphragm is the chief muscle of inspiration. It is a dome-shaped, relatively thin, musculotendinous sheet that separates the thoracic and abdominal cavities (G11 1.23, 1.81, 2.1, 2.74, Table 1.2 [p. 24]; G12 1.23, 1.82, 2.1, 2.74, Table 1.2; N 187-190, 256, 257, 323). The diaphragm consists of a central tendon with skeletal muscle fibers radiating from it to the margin of the inferior thoracic aperture as sternal, costal, and lumbar portions. The sternal portion attaches to the posterior surface of the xiphoid process. The costal portion attaches to the costal arch and ribs XI and XII.
The lumbar portion of the diaphragm has a more complicated arrangement (G11 2.72, 2.74; G12 2.72, 2.74; N256). The right crus typically arises from the anterior surface of the bodies of the upper three lumbar vertebrae, and the left crus arises from the upper two lumbar vertebrae. The right and left crura are united by the fibrous median arcuate ligament, which arches over the anterior aspect of the aorta to form the aortic hiatus of the diaphragm. The aorta, therefore, doesn’t actually pierce the diaphragm but rather passes posterior to it, where it is unaffected by movements of the diaphragm during respiration (N227).
In addition to the median arcuate ligament, there also are medial and lateral arcuate ligaments in the lumbar portion of the diaphragm (G11 2.72, 2.74; G12 2.72, 2.74; N 256). The medial arcuate ligament is a fascial thickening that extends laterally over the psoas major muscle between the bodies of lumbar vertebrae and the tip of the transverse process of Lv1. The lateral arcuate ligament is a fascial thickening that passes laterally over the quadratus lumborum muscle from the transverse process of Lv1 to the 12th rib.
The vena caval opening is located within the central tendon and transmits the inferior vena cava and terminal branches of the right phrenic nerve (G11 1.68, 2.74; G12 1.7, 2.74; N 189, 256). The vena caval opening is located at the Tv8 level.
The esophageal hiatus of the diaphragm is an opening through muscle of the right crus at the Tv10 level (G11 1.69, 2.74; G12 1.71, 2.74; N 189, 226, 227, 231, 256). The diaphragmatic musculature at the esophageal hiatus is thought to contribute to the physiologic lower esophageal sphincter that helps prevent the reflux of gastric contents into the esophagus. Other structures traversing the esophageal hiatus include the anterior and posterior vagal trunks and esophageal branches of the left gastric vessels.
The aortic hiatus described above is located at the Tv12 level. The aortic hiatus transmits the thoracic duct and a variable number of other structures in addition to the thoracic aorta.
Each half of the diaphragm (hemidiaphragm) receives motor innervation (GSE) from a phrenic nerve carrying fibers from spinal cord segments C3, C4, and C5 (N 187, 189). The phrenic nerves also supply general sensation (e.g., GSA, pain and proprioception) to all but the periphery of the diaphragm. The lower intercostal nerves supply general sensation to the peripheral portion of the diaphragm.
Any process that irritates a phrenic nerve (e.g., inflammation of diaphragmatic parietal pleura or diaphragmatic parietal peritoneum) may result in referred pain to the ipsilateral shoulder via supraclavicular nerves (C3, C4), which are cutaneous nerves of the anterior neck. Thus, an inflamed gallbladder (cholecystitis) may refer pain to the right shoulder, and a ruptured spleen may refer pain to the left shoulder.
Before leaving study of the diaphragm, review the pleural costodiaphragmatic recesses (G11 1.21, 1.24A & C, 1.26, 1.81B; G12 1.21. 1.24A & C, 1.26, 1.82A; N 190-192, 224, 325). Place your hand into them and note the relationship of the right costodiaphragmatic recess to the liver and of the left costodiaphragmatic recess to the spleen. A carelessly performed splenic or liver biopsy may contaminate the pleural cavity and damage the lung.
The psoas major muscle arises from tendinous arches attached to Tv12 and lumbar vertebral bodies and intervertebral discs and to the transverse processes of lumbar vertebrae (Fig. 5B; G11 2.63, 2.72; G12 2.63, 2.72; N 256, 484). It descends inferolaterally and joins the iliacus muscle to pass deep to the inguinal ligament and enter the thigh. Note the psoas fascia covering the psoas major. Infections (e.g., tuberculosis, septic discitis) may spread from the lumbar spine deep to the psoas fascia to enter the upper thigh.
The iliacus muscle arises from the iliac fossa and crest, lateral sacrum, and anterior sacroiliac ligaments (G11 2.72, 5.17; G12 2.72, 5.20A; N 256). Together, the psoas major and iliacus form the iliopsoas muscle, which is the strongest flexor of the thigh at the hip joint. Acting from its distal attachment on the lesser trochanter of a stabilized femur, the iliopsoas flexes the trunk on the thigh (performing sit-ups). The psoas major portion of iliopsoas also can act from its femoral attachment to move the lumbar spine.
A number of visceral organs are closely related to the iliopsoas muscle (e.g., kidneys, ureters, cecum and appendix) (G11 2.63; G12 2.63, N 308). Inflammation of one of these organs usually
results in pain if the patient is asked to flex the thigh against resistance or if it is passively extended (positive iliopsoas/psoas sign; e.g., see http://www.aafp.org/afp/1999/1101/p2027.html ).
A slender psoas minor muscle may be present on the anterior surface of one or both psoas major muscles. It passes from vertebrae Tv12 and Lv1 and the intervening intervertebral disc to the pecten pubis (pectineal line) and iliopubic eminence. The psoas minor weakly flexes the lumbar vertebral column.
The quadratus lumborum muscle attaches to the iliac crest and transverse process of Lv5 inferiorly (G11 2.72; G12 2.72; N 256, 309). As it ascends it has attachments on the transverse processes of the upper lumbar vertebrae, hidden behind the psoas major, before ending superiorly on rib XII. Acting unilaterally the quadratus lumborum bends the vertebral column to the ipsilateral side. The muscles of the two sides fix the 12th ribs in position during inspiration.
The most lateral part of the posterior abdominal wall is formed by the transversus abdominis muscle, which was described with muscles of the anterior abdominal wall.
The posterior abdominal wall muscles are innervated by components of the lumbar plexus of nerves (described below). The psoas major is innervated mainly by direct branches from anterior rami of spinal nerves L1 to L3/4. The iliacus is innervated by the femoral nerve (L2-4). Psoas minor is innervated by the anterior ramus of L1. The quadratus lumborum is innervated by the anterior rami of spinal nerves T12-L4.19. Clean and study the components of the diaphragm and the muscles of the posterior abdominal wall. You may have to rotate the kidneys and suprarenal glands toward the midline and remove extraperitoneal fat. If the diaphragm has been damaged in previous dissections on your cadaver, be sure to look on another body. Identify the right crus and the left crus united over the aortic hiatus by the median arcuate ligament at Tv12. Find the medial arcuate ligament arching over the psoas major and the lateral arcuate ligament over the quadratus lumborum. Identify the central tendon and its vena caval opening at the Tv8 level. Locate the esophageal hiatus, which is an opening through the muscle of the right crus at the Tv10 level.
20. Study the psoas major, psoas minor (if present), quadratus lumborum, and the origin of the transversus abdominis. Pay attention to the fascia covering the muscles. Endoabdominal fascia separates the muscles of the abdominal wall from parietal peritoneum and is named regionally for the structures it covers. Thus, psoas fascia covers the psoas major, quadratus lumborum fascia covers that muscle, and transversalis fascia covers the internal surface of transversus abdominis. (Note: some authors label the quadratus lumborum fascia as the “anterior layer of thoracolumbar fascia.” Both are acceptable terms.) XXX
Nerves of the posterior abdominal wall include somatic nerves (the subcostal nerve and lumbar plexus) and the lumbar sympathetic trunks (G11 2.72, 2.73; G12 2.72, 2.73; N 260, 308, 485). The subcostal nerve is the anterior ramus of T12. It passes behind the lateral arcuate ligament and across the front of the quadratus lumborum to course below the 12th rib and into the anterolateral abdominal wall (Fig. 5B).
The lumbar plexus of nerves is formed within the substance of the psoas major by the anterior rami of spinal nerves L1-4 with a contribution from the anterior ramus of T12 (Figs. 5A-B; G11 2.72, 2.73; G12 2.72, 2.73; N 260, 485, 486). The iliohypogastric and ilioinguinal nerves typically arise as a single trunk from the anterior ramus of L1. The trunk emerges from behind the medial arcuate ligament and passes anterior to the quadratus lumborum muscle. The site of division into a superiorly-located iliohypogastric nerve and an inferiorly-located ilioinguinal nerve is variable.
The iliohypogastric nerve typically runs above and parallel to the iliac crest and reaches the skin of the suprapubic region, which it innervates. The ilioinguinal nerve, however, may run either above or below the level of the iliac crest. It then traverses the inguinal canal to exit through the superficial inguinal ring (G11 2.4, 2.5, 2.8A, 2.11; G12 2.36, 2.46, 2.84A, 2.11). The ilioinguinal nerve innervates skin of the upper medial thigh and the anterior portion of the external genitalia.
The genitofemoral nerve is formed from L1-2. It pierces the upper part of the psoas major and descends on the anterior surface deep to the psoas fascia. The genitofemoral nerve divides into genital and femoral branches. In the male, the genital branch enters the inguinal canal via the deep inguinal ring to provide motor innervation to the cremaster muscle (G11 2.12, 2.72, 5.13A; G12 2.12, 2.72, 5.16A; N 255) and, along with the ilioinguinal nerve, provides the sensory innervation of the anterior scrotum. In the female the genital branch is sensory to the mons pubis and anterior portion of the labium majus along with the ilioinguinal nerve. The femoral branch of genitofemoral nerve descends deep to the inguinal ligament to supply skin of the upper anterior thigh.
The lateral femoral cutaneous nerve (lateral cutaneous nerve of the thigh) is formed by the anterior rami of L2 and L3. It emerges from the lateral border of the psoas major and crosses the iliacus muscle to pass deep to the inguinal ligament just medial to the anterior superior iliac spine (ASIS) (G11 2.72, 2.73, 5.13A; G12 2.72, 2.73, 5.16A; N 260, 486). The lateral femoral cutaneous nerve is sensory to skin of the anterolateral thigh. The nerve may be compressed in obese individuals or people who wear heavy tool belts, producing pain, paresthesia, and sensory loss (meralgia paresthetica).
The femoral nerve, formed by L2-4, is the largest branch of the lumbar plexus. It emerges from behind the lateral border of the psoas major and descends in the groove between it and the iliacus muscle (Fig. 5B). The femoral nerve passes deep to the middle of the inguinal ligament lateral to the external iliac artery. After innervating the iliopsoas muscle, the femoral nerve is the motor nerve to the anterior muscles of the thigh. It should be noted that the external iliac artery changes names to become the femoral artery at the inguinal ligament.
The obturator nerve is formed by the anterior rami of L2-4. The nerve emerges from the medial border of the psoas major and enters the lesser (true) pelvis. It leaves the lesser pelvis below the superior pubic ramus through the obturator canal to enter the medial compartment of the thigh. The obturator nerve is motor to the adductor muscles of the thigh and supplies cutaneous innervation to a small area of the upper medial thigh.
The lumbosacral trunk is formed by the anterior rami of L4-5 and descends over the ala of the sacrum to enter the lesser pelvis. It contributes to formation of the sacral plexus.21. Find and clean the subcostal nerve and the branches of the lumbar plexus. Identify the iliohypogastric and ilioinguinal nerves. Note that they separate from each other in different locations on different bodies. Clean the genitofemoral nerve piercing the psoas major muscle. Be aware of its division into genital and femoral branches, but the division is usually near the inguinal ligament and may be difficult to demonstrate. Verify that the lateral femoral cutaneous nerve passes deep to the lateral portion of the inguinal ligament to enter the thigh. Uncover the thick femoral nerve, which usually is hidden under the lateral border of the psoas major. Look for the obturator nerve descending into the lesser pelvis on the medial side of the psoas major. Expose the lumbosacral trunk descending across the ala of the sacrum into the pelvis. On one side of the body, carefully pick away the psoas major muscle to study formation of the branches of the lumbar plexus. XXX
The lumbar sympathetic trunks descend through the abdominal cavity along the anterolateral surfaces of vertebral bodies (G11 2.72; G12 2.72; N 260). Typically there are four lumbar sympathetic (paravertebral) ganglia on each side with each ganglion connected to a lumbar spinal nerve by a gray communicating ramus (gray ramus communicans). In addition, the first two (or three) lumbar sympathetic ganglia also have white rami communicantes and send preganglionic lumbar splanchnic nerves to the inferior mesenteric ganglion.
22. Clean the lower portions of the lumbar sympathetic trunks on the anterolateral surfaces of the lumbar vertebral bodies, in the grooves formed by the adjacent psoas major muscles. Identify gray rami communicantes passing laterally from lumbar sympathetic ganglia to lumbar spinal nerves. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.