Vertebral Column & Spinal Cord
The skeleton of the back consists of the vertebral column, which is composed of vertebrae and the intervertebral discs that connect the bodies of adjacent vertebrae. There are 33 vertebrae subdivided into five regions (described below). The vertebral column is part of the axial skeleton, which also includes the cranium, hyoid bone, ribs, and sternum.
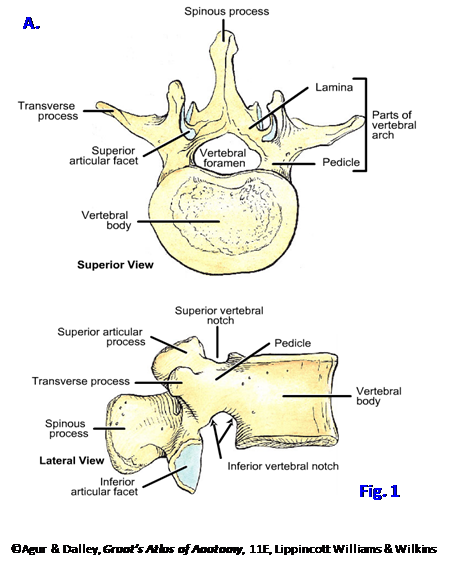 A typical vertebra consists of an anterior vertebral body and a posterior vertebral arch, which enclose a vertebral foramen between them. The combined vertebral foramina in the articulated vertebral column form the vertebral canal, which contains the spinal cord and the membranes that enclose it, the meninges.
A typical vertebra consists of an anterior vertebral body and a posterior vertebral arch, which enclose a vertebral foramen between them. The combined vertebral foramina in the articulated vertebral column form the vertebral canal, which contains the spinal cord and the membranes that enclose it, the meninges.
The vertebral arch is formed by two pedicles and two laminae (Fig. 1A). Each pedicle projects posteriorly from the vertebral body. The pedicle has a shallow superior vertebral notch and a deep inferior vertebral notch. The vertebral notches of adjacent vertebrae form an intervertebral foramen, through which a spinal nerve exits the vertebral canal (Fig. 2; G11 4.4, 4.13D, 4.23A-B, 4.25; G12 4.4, 4.16B, 4.17A; N 151-153, 155).
A spinous process projects posteriorly (and in some cases downward) in the midline from the junction of the two laminae. From the junction of the pedicle and lamina on each side, a transverse process projects laterally, and superior and inferior articular processes project vertically. Each inferior articular process of the vertebra above articulates with a superior articular process of the vertebra below at a synovial zygapophysial (facet) joint (Fig. 2B; G11 4.9B, 4.13D, 4.14, 4.23A; G12 4.10B, 4.16D, 4.21, 4.17A; N 152, 153). The orientation of the zygapophysial joints largely determines the movements permitted in each region of the vertebral column. The zygaphophysial joints are synovial joints and, therefore, may develop osteoarthritis (degenerative joint disease) with age or injury. The resulting osteophytes (bone spurs) can compress the spinal nerve at an intervertebral foramen (note the relationship of the joint and the foramen in Fig. 2B).
1. On a skeleton and individual bones study the basic structure of a typical vertebra (Fig. 1; G11 4.4, 4.6, Table 4.3 [p. 289]; G12 4.4, 4.6, N151, 152). Identify each part. XXX
Although each vertebra is unique, most have characteristic features of the region of the vertebral column from which they come. Thus, there are cervical, thoracic, lumbar, sacral, and coccygeal vertebrae. Of the 7 cervical vertebrae, Cv3-6 are considered typical cervical vertebrae. They are characterized by their small size, a transverse foramen (foramen transversarium) for the vertebral artery and accompanying veins in each transverse process, and a short, often bifid, spinous process (G11 4.9, 4.10; G12 4.10, 4.9 N20, 21). On each side the body of these typical cervical vertebrae has a lip of bone projecting superiorly, the uncus or uncinate process. These articulate with the body of the vertebra above in uncovertebral “joints” (of Luschka), which may become sites of osteophyte formation to produce neck pain. The atypical cervical vertebrae—the atlas (Cv1), axis (Cv2), and vertebra prominens (Cv7)—were studied during the “Deep Back and Suboccipital Triangle” lab and will be revisited during the Head and Neck block.
Thoracic vertebrae are characterized by costal facets on their bodies for articulation with the heads of ribs (G11 4.12; Table 4.2 [p. 286]; G12 4.15; N151). The typical thoracic vertebra has superior and inferior costal facets on each side of the vertebral body; thus, the head of the rib articulates with the bodies of two adjacent vertebrae and an intervertebral disc (G11 1.12A-B, 1.13; G12 1.12A-B, 1.13; N180, 181). There also is a facet on the transverse process of the vertebra for articulation with the tubercle of the rib of the same number. The other distinguishing feature of typical thoracic vertebrae is a long, downwardly sloping spinous process.
Lumbar vertebrae are characterized by their large bodies, which support more weight than cervical and thoracic vertebrae (G11 4.13; Table 4.3 [p. 289]; G12 4.16; N152, 153). They have a short, broad, hatchet-shaped spinous process. They also have a characteristic mammillary process on the posterior surface of each superior articular process for attachment of the multifidus.
The sacrum is a large triangular structure formed by fusion of the five sacral vertebrae in adults (G11 4.16B, 4.17; G12 4.23B, 4.24; N154). The anterior pelvic surface of the sacrum is concave and the posterior surface is convex. The continuation of the vertebral canal in the sacrum is the sacral canal. From it pelvic (anterior) sacral foramina and posterior sacral foramina transmit the anterior rami and posterior rami, respectively, of sacral spinal nerves (G11 4.17A-B, 4.42, 4.43; G12 4.24A-B, 4.43, 4.44; N157, 158).
The sacral canal opens inferiorly at the sacral hiatus on the posterior surface where the laminae and spinous process of Sv5 are missing. Inferior projections of bone on each side of the sacral hiatus, the sacral cornua (G11 4.17B; G12 4.24B; N154), represent the inferior articular processes of Sv5 and are landmarks for caudal epidural anesthesia.
The base of the sacrum articulates above with the fifth lumbar vertebra by an intervertebral disc and articular processes. The sacrum articulates on each side with a hip bone by the sacroiliac joint (G11 4.18B, 4.19; G12 4.26B, 4.27; N332, 333, 335). Note the auricular surfaces of the sacrum and ilium, which form the synovial portion of the sacroiliac joint (G11 4.16, 4.18, 4.19; G12 4.23, 4.26; N154, 474). Inferiorly the apex of the sacrum articulates with the coccyx via the sacral cornua.
The coccyx (tail bone) is a small triangular bone formed by the fusion of four coccygeal vertebrae (G11 4.16B, 4.17A-B; G12 4.23C, 4.24A-B; N154). As anatomical variations three or five coccygeal vertebrae may be present. Frequently, the first coccygeal vertebra (Cov1) is separate with the caudal three vertebrae fused together. The coccygeal cornua articulate with the sacral cornua, but with age the first coccygeal vertebra may fuse with the sacrum.
The vertebral bodies are bound together by intervertebral discs and by anterior and posterior longitudinal ligaments (Fig. 2; G11 4.1, 4.23-4.25; G12 4.1, 4.17-4.19; N 152, 156). Intervertebral discs are located between the bodies of adjacent vertebrae and act as shock absorbers. They consist of a central semifluid nucleus pulposus enclosed by a fibrocartilaginous anulus fibrosus. The anulus consists of concentric lamellae with the collagen fibers of adjacent lamellae running at different angles. The anulus fibrosus is thinner posteriorly, predisposing to protrusion (bulging) or herniation (rupture) of the nucleus pulposus through the anulus in that direction (N158 [upper right figure]); however, the support provided by the midline posterior longitudinal ligament usually directs the protrusion or herniation in a posterolateral direction. For more information, see http://www.aafp.org/afp/990201ap/575.html
The posterior longitudinal ligament is a narrow band ascending along the posterior surfaces of the vertebral bodies and intervertebral discs within the vertebral canal (Fig. 2B; G11 4.24A-B, 4.25; G12 4.18A-B, 4.19; N156). The posterior longitudinal ligament and posterior part of the annuli fibrosi are innervated by recurrent meningeal branches of spinal nerves that pass back (recur) through intervertebral foramina into the vertebral canal (G11 4.23B; G12 4.17B; N163). Only the outer layers of the anulus are innervated.
The broad anterior longitudinal ligament covers the anterior and anterolateral surfaces of the vertebral bodies and intervertebral discs (G11 4.24A, 4.25; G12 4.18A, 4.19; N155, 156). It is a strong, fibrous band that helps to limit extension of the vertebral column and is the only ligament that does so.
The vertebral arches are also joined by ligaments, including the ligamenta flava, interspinous, and supraspinous ligaments (G11 4.24A, 4.25; G12 4.18A, 4.19; N156). The ligamenta flava are yellow elastic ligaments that connect the laminae of adjacent vertebrae. They resist abrupt flexion of the vertebral column, and their elasticity aids extension of the flexed column. Thin interspinous ligaments join the spinous processes of adjacent vertebrae, and the cord-like supraspinous ligament connects the tips of spinous processes as high as Cv7. The supraspinous ligament is expanded in the cervical region as a fibroelastic sheet, the nuchal ligament, to substitute for the short spinous processes in providing muscle attachments (G12 4.10C; N 22).
2. Now turn your attention to the prone cadaver. On ALL BUT 5-6 CADAVERS selected by Dr. Roque or Dr. Roy, the vertebral canal will be opened and the contents studied. The deep back muscles will be preserved only in the 5-6 selected cadavers.
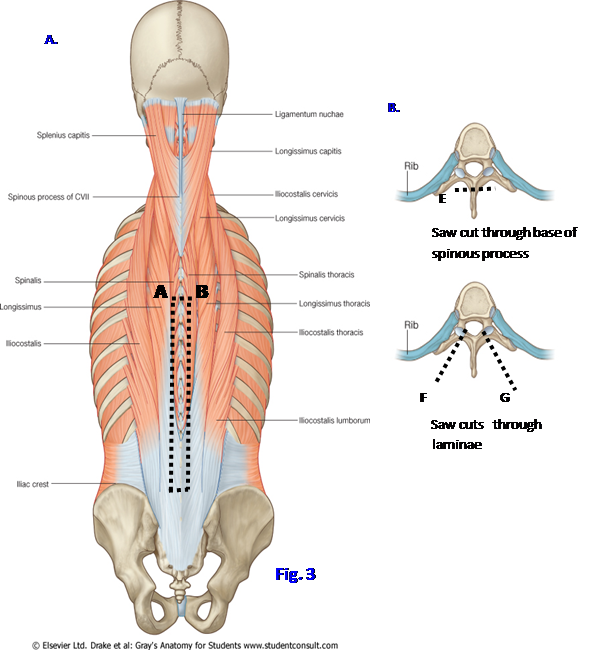
3. Fig. 3A Use a scalpel to make vertical cuts (A⇒C; and B⇒D) through muscle down to the laminae of vertebrae just to the sides of the spinous processes from the midthoracic level (Tv6 or Tv7) above to the supracristal plane at the level of the highest points of the iliac crests (Lv4) below. Remove the mass of muscle near the midline on each side to expose the laminae.
4. Fig. 3B Using a Stryker saw, make a coronal cut through the base of the spinous processes from Tv6 to Lv4 as close to the junction of the laminae as possible (E) and remove the spinous processes and attached interspinous ligaments and muscles en bloc.
5. Fig. 3C, F and G In order to open the vertebral canal (laminectomy), saw through the lateral part of the exposed series of laminae on each side with the saw blade angled slightly inward. Make transverse incisions connecting the superior and inferior ends of the longitudinal cuts (A⇒B, C⇒D) and remove the mobilized posterior parts of the vertebral arches. Examine the deep surface of the removed laminae to identify the intervening ligamenta flava. XXX
The vertebral canal contains the spinal cord enclosed within three layers of membranes, the meninges. Outside the outermost layer of meninges is the epidural space. The epidural space contains epidural fat and the internal vertebral plexus of veins. This venous plexus communicates with an external vertebral venous plexus around the vertebral column and with dural venous sinuses inside the cranial cavity (G11 4.26, 4.44, 4.47A, 7.16A; G12 4.20, 4.46, 4.48B, 7.21A; N102, 166). These communications are clinically significant because the valveless vertebral venous plexus also communicates with veins within the pelvic cavity and the thoracoabdominal region, providing a pathway for the spread of cancer cells or infection to the vertebral column, spinal cord, and brain (e.g., prostate cancer often metastasizes to the vertebral column via this route). For example, see http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=ENE2006056002136 and http://www.medscape.org/viewarticle/522597_4
The spinal cord is enclosed by three meninges (G11 4.40-4.46; G12 4.41-4.44, 4.46-4.47, 4.49; N157, 162, 163). The dura mater is the tough, fibrous outer layer, which forms a tubular sac within the vertebral canal. The spinal dura mater is continuous superiorly with the meningeal layer of the cranial dura mater at the foramen magnum and inferiorly extends to the level of the sacrum. Below Sv2 the dura covers the filum terminale (filum terminale internum) as the filum of dura mater (coccygeal ligament, filum terminale externum) to attach to the coccyx. Note that the dura mater forms sleeves that cover the nerve roots laterally to the intervertebral foramina (G11 4.42; G12 4.43; N162). The spinal dura is innervated by recurrent meningeal (sinuvertebral) branches of the spinal nerves that pass back (recur) through intervertebral foramina into the vertebral canal (G11 4.23; G12 4.17B; N163).
The arachnoid mater is a thin, translucent membrane held against the internal surface of the dura mater by a combination of weak intercellular junctions and cerebrospinal fluid (CSF) pressure (G11 4.43A, 4.44; G12 4.44A, 4.46; N162, 163). Consequently, there is no natural subdural space. The arachnoid mater is separated from the innermost layer of meninges, the pia mater, by the subarachnoid space, which contains the CSF. Delicate strands of connective tissue, the arachnoid trabeculae, cross the subarachnoid space, connecting the arachnoid and pia and helping to suspend the spinal cord. The subarachnoid space is enlarged below the termination of the spinal cord at Lv1 as the lumbar cistern, which is accessed clinically to extract samples of CSF (lumbar puncture) or to inject anesthetic (spinal block). For example, see http://www.emedicine.com/proc/topic80773.htm
6. Make a longitudinal midline incision along the length of the exposed dura mater. Make transverse incisions on each side from the superior and inferior ends of the first incision and retract the flaps of dura laterally. In the cadaver the arachnoid mater is often separated from the inner surface of the dura mater and appears as a separate filmy membrane. This separation between the dura and arachnoid is an artifact of embalming. If the arachnoid mater has separated and is covering the spinal cord, carefully incise and reflect it.
7. Study the specializations of the pia mater. Continuing directly inferiorly from the tapered inferior end of the spinal cord is the filum terminale surrounded by a collection of nerve roots, the cauda equina (G11 4.43A; G12 4.44A; N157). Look for a narrow whitish band, the denticulate ligament, leaving each side of the spinal cord to attach to the inner surface of the arachnoid-lined dural sac by thin, pointed processes (G11 4.45A; G12 4.42A; N162). XXX
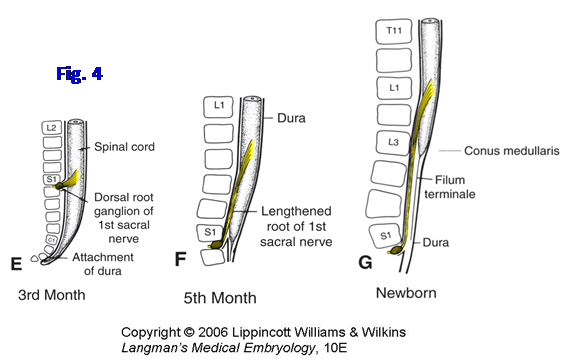
The spinal cord (spinal medulla) is the elongated inferior portion of the central nervous system (G11 4.40, 4.41; G12 4.41, 4.47; N157). It is continuous above with the brainstem at the foramen magnum. Its tapered lower end, the conus medullaris, usually terminates at the lower border of the first lumbar vertebra (Lv1) (G11 4.43; G12 4.44; N 157, 158). However, the spinal cord may terminate as high as vertebra T12 or as low as L3 in the adult, an anatomical variation that may be clinically important in patients with vertebral fractures. The filum terminale (filum terminale internum) extends inferiorly from the conus medullaris (Fig. 4G).
The spinal cord has two enlargements associated with the innervation of the extremities (G11 4.40; G12 4.41; N158). The cervical enlargement (C5-T1) gives rise to the right and left brachial plexuses to the upper limbs. The lumbosacral enlargement (L1-S3) gives rise to the lumbosacral plexuses, which innervate the lower limbs.
The posterior (dorsal) and anterior (ventral) rootlets of spinal nerves leave the spinal cord and unite into posterior and anterior roots, respectively (G11 4.45A, 4.46; G12 4.42A, 4.49, N162). The posterior root contains a collection of afferent (GSA and GVA) neuron cell bodies within a swelling located within the intervertebral foramen, the posterior root ganglion. The posterior and anterior roots unite just distal to the posterior root ganglion to form a short spinal nerve, which divides into posterior and anterior primary rami.
The posterior rami of spinal nerves divide into medial and lateral branches to innervate intrinsic back muscles and the overlying skin (G12 4.17B; N 163, 174). Small articular nerves from the medial branches of posterior rami supply the zygapophysial joints. Anterior rami of spinal nerves innervate all of the skeletal muscles of the trunk and extremities except intrinsic back muscles. Anterior rami also innervate most of the length of the dermatomes, all except for the narrow segments overlying the intrinsic back muscles.
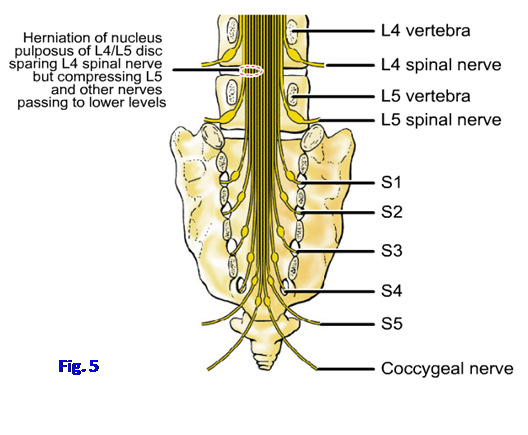
There are 31 pairs of spinal nerves with 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and one coccygeal (G11 4.45B; G12 4.50; N 158). Cervical spinal nerves are numbered according to the vertebra below (e.g., spinal nerve C4 leaves the vertebral canal through the intervertebral foramen above Cv4). All other spinal nerves are numbered according to the vertebra above (e.g., spinal nerve L4 leaves the vertebral canal below Lv4, as shown in Fig. 5 below).
 Small longitudinally-oriented arteries provide the blood supply to the spinal cord (G11 4.47; G12 4.48; N 164, 165). The single anterior spinal artery descends within the anterior median fissure of the spinal cord. The paired posterior spinal arteries descend just medial to the dorsal rootlets entering the posterolateral sulci of the cord.
Small longitudinally-oriented arteries provide the blood supply to the spinal cord (G11 4.47; G12 4.48; N 164, 165). The single anterior spinal artery descends within the anterior median fissure of the spinal cord. The paired posterior spinal arteries descend just medial to the dorsal rootlets entering the posterolateral sulci of the cord.
Segmental arteries (e.g., from posterior intercostal arteries) traverse intervertebral foramina to supply nerve roots or anastomose with the spinal arteries. These small arteries may be difficult to see in gross specimens, but be aware of their importance. Anterior and posterior segmental medullary arteries carry blood to supplement the small amount carried by the spinal arteries. One segmental artery arising from a left (65%) lower intercostal or upper lumbar artery, the great (major) anterior segmental medullary artery (of Adamkiewicz), is especially important for the blood supply of the lower 2/3 of the spinal cord, including the lumbosacral enlargement. Its occlusion or injury may result in the loss of voluntary movements in the lower portion of the trunk and the lower extremities (paraplegia). If segmental medullary arteries reinforcing the posterior spinal arteries are also involved, the paraplegia is accompanied by loss of sensation (anesthesia). A severe drop in systemic blood pressure for several minutes may reduce blood flow within the segmental medullary arteries with similar results.
During the third month of fetal life, the spinal cord occupies the entire length of the vertebral canal. After the third month the vertebral column and dura-arachnoid grow more rapidly than the spinal cord. Due to this differential growth, the spinal cord ends, on average, opposite vertebra Lv3 in the newborn and at the lower border of Lv1 in the adult (Fig. 4; G11 4.43, 4.48A-B; G12 4.44, 4.50A-B; N158). The filum terminale (internum) represents the tract of regression of the spinal cord. The other consequence of this differential growth is that only the cervical spinal nerve roots leave the spinal cord opposite the intervertebral foramen through which they exit the vertebral canal. Spinal nerve roots of other regions descend for increasing distances as one approaches the lower end of the spinal cord. The collection of obliquely descending nerve roots below the conus medullaris, on both sides of the filum terminale, resembles a horse’s tail and is thus called the cauda equina (G11 4.43, 4.48B; G12 4.44, 4.50B; N157, 158).
The lumbar cistern occupied by the cauda equina from Lv2 to Sv2 can be used to withdraw CSF or to inject anesthetic because the slender nerve roots roll away from the tip of the inserted needle. Typically a lumbar spinal puncture (lumbar puncture) is performed between the spinous processes of Lv3 and Lv4 or between Lv4 and Lv5. The supracristal plane transecting the highest points of the right and left iliac crests usually passes through the Lv4 spinous process and is used as a landmark for lumbar punctures.
The other consequence of the obliquity of the descending nerve roots in the lumbar region is that an intervertebral disc that protrudes or herniates in the usual posterolateral direction typically compresses the nerve root descending to exit at the intervertebral foramen below the next vertebra down (traversing root) rather than the nerve root that exits at the level of the disc (exiting root). For example, a herniated L4/5 disc usually compresses the L5 nerve root instead of L4 because L4 exits above the site of herniation (Fig. 5; N158 [upper right]).8. Study the spinal cord and cauda equina. Follow anterior and posterior rootlets from a spinal cord segment as they unite into anterior and posterior roots, which in turn join to form a short spinal nerve. Carefully chip away the articular processes forming the posterior walls of 3-4 intervertebral foramina to expose the posterior root ganglia and spinal nerves. Find the division of each exposed spinal nerve into anterior and posterior primary rami.
9. Cut a 2-3 cm segment from the thoracic spinal cord and remove it. Look for the small anterior and posterior spinal arteries on the removed segment. On the cut end of the spinal cord study the butterfly-shaped gray matter and surrounding white matter (G11 4.41, 4.46; G12 4.47, 4.49; N163 [upper figure]). Identify the posterior and anterior horns of gray matter. In the small area where the section of spinal cord was extracted, remove any remaining meninges, epidural fat, and vertebral veins to expose the anterior wall of the vertebral canal (G11 4.24; G12 4.18; N155, 156). Identify the posterior longitudinal ligament and study its relationship to intervertebral discs. Pay attention to the relationship of the posterior root ganglion and spinal nerve to the intervertebral disc at the intervertebral foramen. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.