Pelvis and Bisect
The pelvis is the part of the trunk inferior to the abdomen and is an area of transition between the trunk and lower limbs. It comprises the pelvic cavity enclosed by the pelvic walls. The pelvic walls are formed by the bony pelvis consisting of two hip (coxal) bones, the sacrum, and the coccyx covered internally and externally by muscles and fasciae (Fig. 1; G11 3.1A, 3.2A; G12 3.4A, 3.3A; N 241, 332, 333).
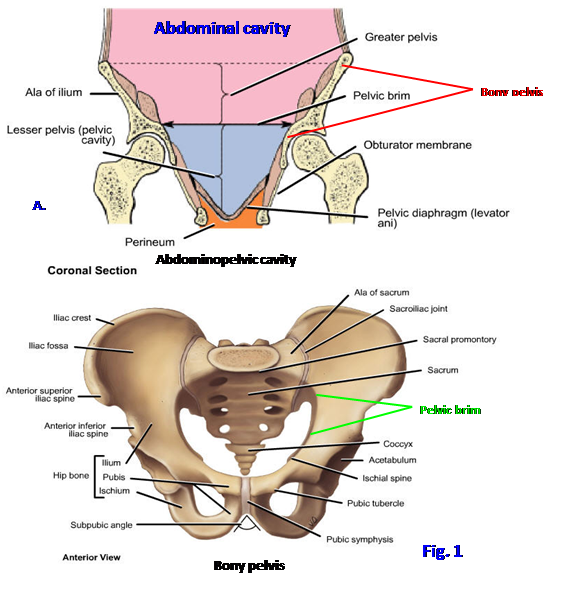
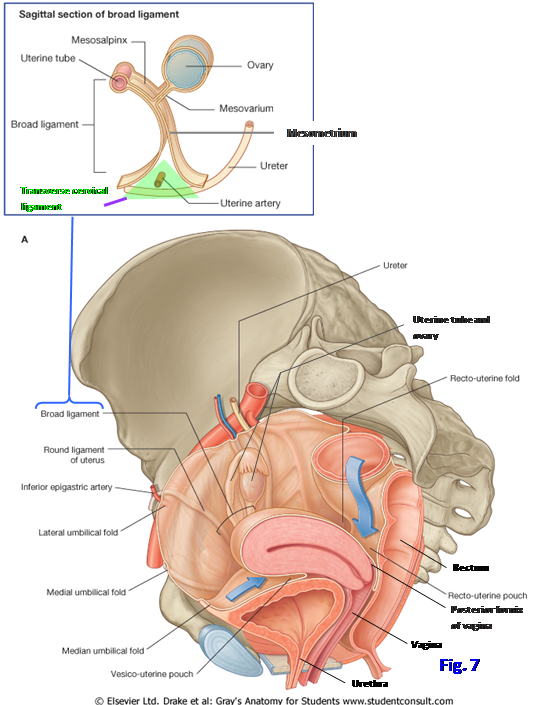
The pelvic cavity is the inferior portion of the continuous abdominopelvic cavity, which extends from the respiratory diaphragm above to the pelvic diaphragm below (Fig. 1A; G11 2.22A, 3.2B; G12 2.19, 3.3A; N 323). The pelvic cavity contains the lowest portion of the serous peritoneum, which encloses part of the greater sac of the peritoneal cavity. As in the abdomen, some organs invaginate the peritoneal sac and are invested by a layer of visceral peritoneum to become intraperitoneal (i.e., the uterine tubes in the female) (N 342, 343). Most organs remain behind or below the parietal peritoneum of the peritoneal sac as extraperitoneal (retroperitoneal, subperitoneal) pelvic organs.
The pelvis is subdivided into the greater (false) and lesser (true) pelves (Fig. 1A; N336 [upper]). The bony walls of the greater pelvis protect the lower abdominal viscera (e.g., loops of ileum, sigmoid colon), while the skeleton of the lesser pelvis protects pelvic organs. The lesser pelvis also provides attachments for structures of the perineum, which is the region inferior to the pelvic diaphragm and between the thighs. The boundary between the greater pelvis and lesser pelvis is a ridge of bone, the pelvic brim (margin of superior pelvic aperture), which is described below.
The bony pelvis is a ring of bone (Fig. 1B; G11 3.1A, 3.2A, 4.15; G12 3.4A, 3.3A, 4.22A; N 241, 332). It bears the weight of the body when sitting, transfers weight from the axial skeleton to the lower extremity skeleton when standing and walking, provides for the attachment of abdominal wall and lower extremity muscles, and encloses and protects lower abdominal and pelvic organs.
The bony pelvis is formed by the two pelvic girdles anteriorly and laterally and by the sacrum and coccyx posteriorly (Fig. 1B; G11 3.1A, 3.2A, 4.15; G12 3.4A, 3.3A, 4.22A; N 332, 336). Each pelvic girdle corresponds to a pectoral girdle formed by the clavicle and scapula in the upper extremity. (Note: Unfortunately, some authors use the terms “pelvic girdle” and “bony pelvis” synonymously, but of course the sacrum and coccyx are parts of the vertebral column.) The two pelvic girdles articulate with each other in the anterior midline at the cartilaginous pubic symphysis and posteriorly with the sacrum at the right and left sacroiliac joints (famed of story and song, as in “oh, my aching sacroiliac”) (G11 4.18, 4.19; G12 4.26, 4.27; N 332, 340).
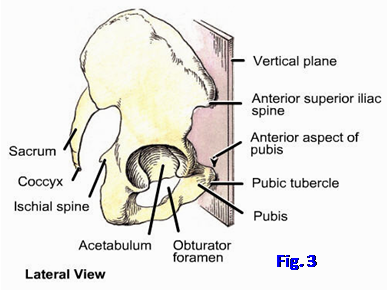
The orientation of the bony pelvis in the anatomical position is tilted anteriorly so that the anterior superior iliac spines and anterior border of the top of the pubic symphysis lie in the same vertical plane (Fig. 3; G11 3.1B; G12 3.4B; N336).
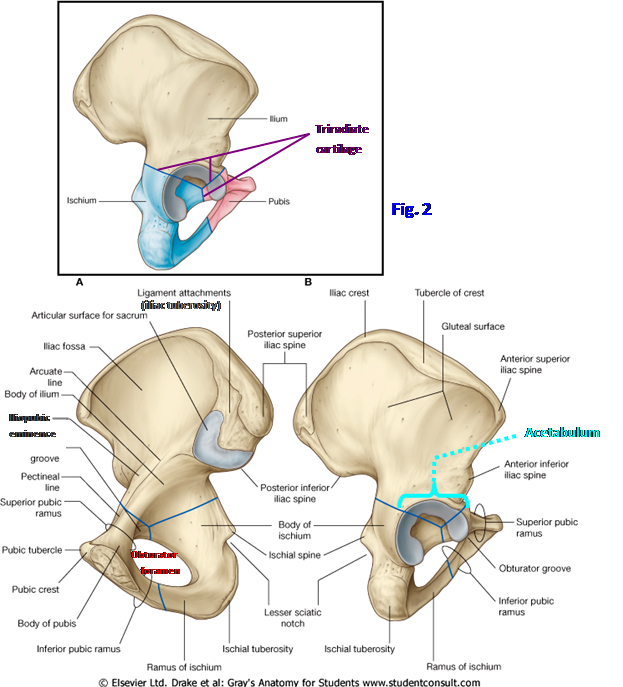
Each pelvic girdle is a hip bone (coxal bone, innominate bone) formed by the fusion of three bones that were originally separate in the fetus. Before skeletal maturity the three bones are joined by the triradiate cartilage at the acetabulum, which is the cup-shaped socket for the head of the femur at the hip joint (Fig. 2B and inset; G11 5.31B; G12 5.31B; N 474). The triradiate cartilage is named for its shape and is a remnant of endochondral ossification. The three bones that fuse to form the pelvic girdle are the ilium, ischium, and pubis. Even though the three bones are fused in the adult, the hip bone is so complex that it is convenient to describe the different parts as though they were still separate bones.
The ilium is the larger, superior part of the hip bone (Figs. 1B, 2; G11 3.1A & C, 3.2, 4.16A, 5.20A & C; G12 3.4A & C, 3.3, 4.23A, 5.22A & C; N 332, 333, 336, 474). It is fan-shaped and consists of a broad upper part, the wing or ala of the ilium, and a narrower inferior part, the body of the ilium. The body of the ilium fuses with the ischium and pubis in formation of the acetabulum. The wing of the ilium has a thickened, convex upper border, the iliac crest, extending between two prominences, the anterior superior iliac spine (ASIS) and the posterior superior iliac spine (PSIS). The iliac crest has a prominence, the tubercle of the iliac crest, about 6 cm behind the anterior superior iliac spine. (Remember that the tubercles of the two iliac crests are landmarks for the transtubercular/intertubercular plane used to help divide the abdomen into 9 regions for localization of abdominal organs.) There is a second prominence inferior to each superior iliac spine, the anterior inferior iliac spine (AIIS) and the posterior inferior iliac spine (PIIS), respectively. The PIIS lies at the upper boundary of a deep concavity on the posterior edge of the hip bone, the greater sciatic notch.
The shallow depression on the inner surface of the wing of the ilium is the iliac fossa (Fig. 2; G11 3.1A & C, 3.2, 4.16A; G12 3.4A & C, 3.3, 4.23A; N 335, 336, 474). Posterior to the iliac fossa on the medial side of the ilium there is an ear-shaped articular facet, the auricular surface, for articulation with the sacrum at the sacroiliac joint. The auricular surface is the site of the synovial portion of the sacroiliac joint. Posterior and superior to the auricular surface is a heavy, roughened area, the iliac tuberosity (tuberosity of the ilium), for attachment of the stout interosseous sacroiliac ligament (G11 3.1C, 4.18; G12 3.4C, 4.26; N 474). This is the syndesmotic (fibrous) portion of the sacroiliac joint. The synovial portion of the joint often also becomes syndesmotic in middle-aged and older individuals, particularly males. Extending anteriorly and inferiorly from the upper half of the auricular surface is a ridge of bone, the arcuate line (Fig. 2A; G11 4.16A; G12 4.23A; N 332, 474). It helps to form the pelvic brim, which is the lateral margin of the pelvic inlet connecting the greater pelvis and the lesser pelvis.
The external (lateral or gluteal) surface of the wing of the ilium has three ridges of variable prominence, the posterior, anterior, and inferior gluteal lines, due to the attachment of powerful muscles of the gluteal region of the lower extremity (G11 5.31A; G12 5.31A; N 336).
The ischium is the posteroinferior component of the hip bone (Fig. 2; G11 3.1C, 4.16A, 5.31; G12 3.4C, 4.23A, 5.31; N 474). The ischium consists of a superior body and an inferior ramus. (Note: some authors describe the boundary between the body and ramus of the ischium as located at the level of the ischial spine, but the account provided here goes back to Henry Gray’s original description.) The body of the ischium fuses anteriorly with the pubis and superiorly with the ilium to form the acetabulum. The ischial spine (spine of the ischium) projects from the posterior border of the body, separating the greater and lesser sciatic notches. Inferiorly the ischium has a thickened, rough prominence on its posterior surface, the ischial tuberosity. We sit on our two ischial tuberosities.
The flattened ramus of the ischium inclines anteriorly, superiorly, and medially from the tuberosity to fuse with the inferior ramus of the pubic bone, forming the ischiopubic ramus (Fig. 2; G11 3.1C, Table 3.1 [p. 191]; G12 3.4C, 3.6; N 336, 474). Thus the ischium and the pubis are the boundaries of the large obturator foramen. In life the obturator foramen is filled by the obturator membrane, except at a small gap anterosuperiorly, the obturator canal (G11 5.30A, 5.35A; G12 5.30A, 5.35A; N 336). The obturator nerve and artery leave the pelvis through the obturator canal to reach the medial compartment of the thigh.
The pubis (pubic bone) is the anteromedial element of the hip bone (Fig. 2; G11 3.1A & C, 4.15, 4.16A, 5.31; G12 3.4A & C, 4.22, 4.23A, 5.31; N 332, 474, 475 [Anterior view]). It consists of a superior ramus that fuses laterally in the acetabulum, an inferior ramus that fuses with the ischial ramus, and a body between the two rami. The superior ramus of the pubis forms the anterior-inferior component of the acetabulum. The pelvic surface of the superior ramus features a ridge that runs posteriorly and superiorly to join the arcuate line of the ilium. This is the pecten pubis (pectineal line), and it is part of the pelvic brim. The junction of the superior ramus and the ilium is marked superiorly by a roughened raised area, the iliopubic eminence.
The body of the pubis is the part that articulates with the contralateral hip bone at the pubic symphysis in the anterior midline. The thickened anterior-superior border of the body is the pubic crest. It ends laterally in a prominence, the pubic tubercle. The pubic tubercle is the medial attachment of the inguinal ligament, which begins laterally at the anterior superior iliac spine.
The flattened inferior ramus of the pubis curves posteriorly, inferiorly, and laterally to fuse with the ischial ramus (G11 3.1C; G12 3.4C). The two together form the ischiopubic ramus. The width of the subpubic angle formed by the two ischiopubic rami meeting at the pubic symphysis is a distinguishing characteristic between male and female pelves (G11 Table 3.1 [pp. 190-191]; G12 3.5; N 334). The female subpubic angle is wider than the male as part of the adaptation for childbirth.
The pubic symphysis is the anterior joint between the two hip bones. It is formed by a fibrocartilaginous interpubic disc and associated ligaments. The medial articular surface of the body of each pubic bone is covered by a thin layer of hyaline cartilage, and this is what actually articulates with the interpubic disc. A small fluid-filled cavity may be present in the upper portion of the interpubic disc in young individuals and often enlarges with age in females.
Ligaments reinforce the pubic symphysis superiorly and inferiorly. The superior pubic ligament runs along the pubic crests from one pubic tubercle to the other, strengthening the anterosuperior aspect of the joint. The arcuate (inferior) pubic ligament arches across the inferior surface of the symphysis between the inferior pubic rami. Tendinous fibers of the rectus abdominis and external abdominal oblique muscles decussate across the anterior surface of the symphysis and provide additional stability.
The sacroiliac joints are combination synovial and fibrous joints (G11 4.18, 4.19; G12 4.26, 4.27). Each joint has an anterior synovial portion formed between the auricular surfaces of the ilium and sacrum. The two auricular surfaces of adults are usually uneven, but congruent, so that they interlock. Behind and above this synovial portion is the syndesmotic portion of the joint between the iliac and sacral tuberosities. The syndesmotic portion is formed mainly by the interosseous sacroiliac ligament. The sacroiliac joint is reinforced by posterior and anterior sacroiliac ligaments (G11 3.3A & D, 4.18B, 4.22A-B; G12 3.7A-B, 4.26B, 4.25A-B; N 335).
Two strong accessory ligaments help to stabilize the sacrum on the hip bone by limiting anteroinferior tilting of the sacral promontory (Fig. 4; G11 3.3A & D, 4.18, 4.22A-B, 5.26, 5.27, Table 3.2 [p. 192]; G12 3.7A-B, 4.26, 4.25A-B, 5.28, 3.8A-B; N155, 335, 336). They are the sacrotuberous and sacrospinous ligaments. The sacrotuberous ligament attaches superiorly to the posterior border of the ilium between the posterior superior and posterior inferior iliac spines and to the back of the sacrum and coccyx. Inferiorly the ligament attaches to the ischial tuberosity. The sacrotuberous ligament’s fibers are closely associated with the tendon of the long head of the biceps femoris muscle. The sacrotuberous ligament forms the lower boundary of the lesser sciatic foramen, which is the inferior and smaller of two openings connecting the pelvic cavity and the gluteal region.
The sacrospinous ligament lies deep to the sacrotuberous ligament (Fig. 4). It passes from the lateral edge of the lower sacrum and upper coccyx to the ischial spine. The sacrospinous ligament separates the greater and lesser sciatic foramina.
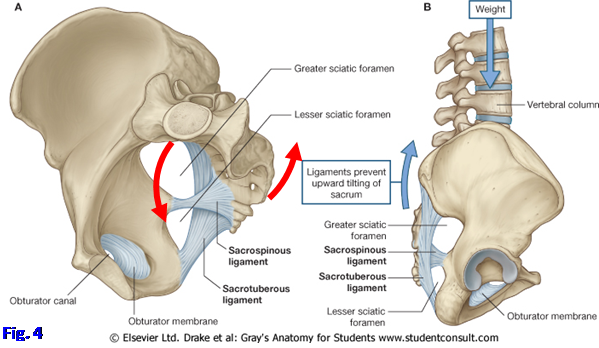
The line of gravity of the body passes anterior to the sacroiliac joints; therefore, there is a tendency for the sacrum to rotate around a horizontal axis so that the sacral promontory moves anteriorly and inferiorly (nutation) into the pelvis while the lower part (apex) of the sacrum and the coccyx tilt posteriorly and superiorly (counternutation) (Fig. 4, red arrows). The sacrotuberous and sacrospinous ligaments hold the apex of the sacrum forward, limiting its posterior and superior rotation.
The sacroiliac joint is further stabilized by the orientation of fibers of the interosseous and posterior sacroiliac ligaments, which pass obliquely upward and laterally from the sacral tuberosity to the iliac tuberosity, so that the weight of the axial skeleton pushing down on the sacrum pulls the ilia medially, compressing the sacrum between them. Adding to stability of the joint is the triangular shape of the sacrum, broader superiorly at its base, which tends to wedge the sacrum between the ilia as weight is transmitted down the vertebral column.
Limited movements at the sacroiliac joints can result from muscle contractions. For example, contractions of the anterior abdominal muscles tend to rotate the anterior portion of a hip bone superiorly at the ipsilateral sacroiliac joint (think ASIS moving upward). The posterior thigh muscles can perform a similar function by pulling downward on the hip bone. The movements produced by muscle contractions are employed clinically to correct malalignments.
Like other joints, the sacroiliac joint is subject to sprain and to inflammation. Inflammation of the sacroiliac joint (sacroiliitis) may occur in association with an injury, infection (e.g., intravenous drug abuse), or as part of a spondyloarthropathy (e.g., ankylosing spondylitis). Pain may be present over the joint with possible referred pain into the buttock, posterior thigh, and groin (e.g., see McGrath, 2004, Journal of Osteopathic Medicine 7(1):16-24).
The pubic symphysis and sacroiliac joints usually allow only limited movements between the two hip bones, but the presence of relaxin and other hormones during pregnancy causes ligaments to relax. This permits increased movement at the pubic symphysis and sacroiliac joints, facilitating childbirth.
1. Study an articulated bony pelvis. Identify the two pelvic girdles, the sacrum, and the coccyx. Note the pubic symphysis, where the two pelvic girdles articulate in the anterior midline, and the right and left sacroiliac joints, where each pelvic girdle articulates with the sacrum. On disarticulated sacrum and hip bones identify the auricular surface for the synovial portion of the sacroiliac joint. Posterior and superior to the auricular surface on each bone find the tuberosity for attachment of the interosseous sacroiliac ligament in the syndesmotic portion of the joint.
2.
Study the orientation of the bony pelvis in the anatomical position. The right and left anterior superior iliac spines and the anterior border of the top of the pubic symphysis occupy the same vertical plane (Fig. 3).
3. Identify the components of each hip bone. The ilium is the superior component, the ischium is the posteroinferior component, and the pubis is the anteroinferior component. They fuse in the acetabulum, the large cup-shaped socket of the hip joint. The location of the triradiate cartilage isn’t evident on skeletal models, but realize that the body of the ilium forms approximately the upper third of the acetabulum, the body of the ischium forms the posterior half of the lower two-thirds of the acetabulum, and the superior ramus of the pubis forms the anterior half of the lower-thirds.
4. Identify the wing (ala) and body of the ilium. Follow the iliac crest along the upper border of the wing from the anterior superior iliac spine (ASIS) to the posterior superior iliac spine (PSIS). Note the tubercle of the iliac crest about 6 cm behind the ASIS. It is the superior attachment of the iliotibial tract. Find the anterior inferior (AIIS) and posterior inferior (PIIS) iliac spines.
5. On the internal surface of the wing study the shallow iliac fossa, where the iliacus muscle attaches. Posterior to this find the roughly ear-shaped auricular surface for articulation with the corresponding surface of the sacrum at the sacroiliac joint. The roughened area posterior and superior to the auricular surface is the iliac tuberosity, where the strong interosseous sacroiliac ligament attaches. Find the arcuate line coursing anteriorly and inferiorly from the upper half of the auricular surface. On the articulated pelvis, verify that the arcuate line is continuous anteriorly with the pecten pubis to help form the pelvic brim. The pelvic brim is the margin of the pelvic inlet connecting the greater and lesser pelves (see below).
6. Study the features of the ischium. It consists of a superior body, which fuses in the acetabulum, and an inferior ramus. The spine of the ischium projects from the posterior border of the body and gives attachment to the sacrospinous ligament. Note that the spine separates the large greater sciatic notch above from the small lesser sciatic notch below. When the hip bone and sacrum are articulated, these are the sites of the greater and lesser sciatic foramina separated by the sacrospinous ligament. The roughened thickening on the inferior part of the ischium is the ischial tuberosity. The ischial tuberosity is the inferior attachment of the sacrotuberous ligament. Several muscles, including the hamstring muscles, also attach there. The ischial tuberosity is also the area on which the weight of the trunk rests in the sitting position.
7. The ramus of the ischium is the thin, flattened part ascending anteriorly and medially from the tuberosity. The ischial ramus fuses with the inferior ramus of the pubis to form the ischiopubic ramus, which is the lower boundary of the large obturator foramen.
8. Identify the body and the superior and inferior rami of the pubis. The body of the pubis is the part that articulates with the contralateral pubic bone at the pubic symphysis. The thickened anterosuperior border of the body forms the pubic crest, which ends laterally in the pubic tubercle. The pubic crest joins the pecten pubis (pectineal line) and arcuate line of the ilium to form the linea terminalis, which meets the ala and promontory of the sacrum to complete the pelvic brim.
9. Follow the superior ramus of the pubis laterally from the body. It fuses with the body of the ilium and the body of the ischium to form the acetabulum. Find the sharp, raised ridge ascending posteriorly on the superior surface of the superior ramus. This is the pecten pubis or pectineal line. Find the thin, flattened inferior ramus of the pubis descending posteriorly and laterally from the body to meet the ischial ramus. In the articulated pelvis note the subpubic angle formed where the two inferior pubic rami meet at the pubic symphysis. Compare this angle in male and female pelves. XXX
The anteroinferior wall of the pelvis is formed by the bodies and rami of the two pubic bones and the pubic symphysis. The lateral walls of the pelvis consist of the two hip bones, the obturator membranes closing the obturator foramina, and covering muscles and fasciae (Figs. 1A, 5; G11 3.2A, 3.3A, Table 3.2 [p. 192]; G12 3.3A, 3.7A, 3.8-3.9; N 336, 337). In the greater pelvis an iliacus muscle takes origin from each iliac fossa. The iliacus joins the psoas major to form the iliopsoas muscle, which passes into the anterior thigh deep to the inguinal ligament to insert into the lesser trochanter (G11 5.17, 5.18; G12 5.20A-B; N 256, 484).
The obturator internus muscle attaches to and covers the lateral wall of the lesser pelvis, inferior to the pelvic brim (G11 3.40A, 5.19, 5.27, 5.33; Table 3.2 [p. 192]; G12 3.44A, 5.21, 5.28C, 5.33, 3.8-3.9; N 337 [Medial view], 340, 372, 398). Its fibers converge toward the lesser sciatic foramen, where it leaves the pelvis to enter the gluteal region. The obturator internus is covered medially by obturator fascia. This fascia is thickened as the tendinous arch of the levator ani (arcus tendineus) along a line extending between the posterior surface of the body of the pubis and the ischial spine (G11 3.4, 3.13C; Table 3.2 [p. 193 upper]; G12 3.10, 3.22C, 3.8-3.9; N 337, 338, 340). The tendinous arch of the levator ani provides attachment for part of the pelvic diaphragm (discussed below).
The posterior wall of the pelvis is formed by the sacrum and coccyx, attached ligaments, and the piriformis muscles (Figs. 4A, 5A-B; G11 3.4, 3.5; Table 3.2 [pp. 192-193]; G12 3.7A, 3.8-3.11; N 335). The ligaments include the anterior sacroiliac, sacrospinous, and sacrotuberous ligaments. Each piriformis muscle arises from the superior portion of the sacrum lateral to the pelvic sacral foramina (G11 3.4, 3.5, 5.25, 5.26; Table 3.2 [pp. 192-193]; G12 3.10, 3.11, 5.27, 5.28, 3.8-3.9; N 337, 338, 340). The piriformis passes laterally and exits the pelvis through the greater sciatic foramen to enter the gluteal region, where it is an important landmark. The anterior rami of nerves that form the sacral plexus run laterally across the surface of the piriformis muscle to reach the greater sciatic foramen (G11 3.5, 3.24, 3.26; G12 3.11, 3.12; N 485, 487). Branches from S1,2 supply the piriformis.
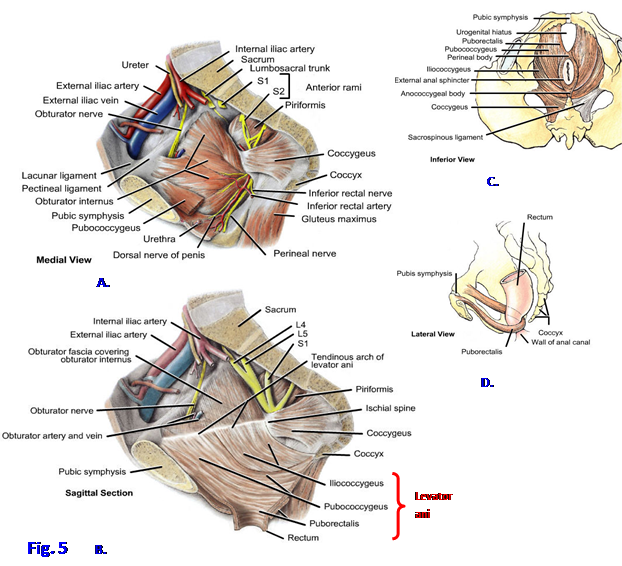
The floor of the pelvis is formed by the funnel-shaped pelvic diaphragm (Figs. 1A, 5B; G11 3.2B, 3.4, 3.5, Table 3.2 [p. 193, upper]; G12 3.8-3.12; N 337-342), which closes the inferior pelvic aperture and separates the pelvic cavity from the perineum. The pelvic diaphragm stretches from one lateral pelvic wall to the other and between the pubis anteriorly and the coccyx posteriorly. It consists of the levator ani and coccygeus muscles and their superior and inferior fasciae.
The levator ani is the larger anterior part of the pelvic diaphragm and is subdivided into three parts—pubococcygeus, puborectalis, and iliococcygeus—named according to their attachments and the direction of their fibers. Part of the levator ani’s origin is from the tendinous arch of the levator ani, which is a thickening of obturator fascia between the posterior surface of the body of the pubis and the ischial spine (Fig. 5B; G11 3.4; Table 3.2 [p. 193, upper]; G12 3.10, 3.8-3.9; N 337, 338, 340). Anteriorly there is a midline gap between the levator ani muscles of the two sides, the urogenital hiatus, which gives passage to the urethra in both sexes and also the vagina in females (Fig. 5C; G11 3.4B, 3.6C; G12 3.9B; N 338, 340).
The pubococcygeus portion of the levator ani arises mainly from the posterior surface of the body of the pubis and passes posteriorly in an almost horizontal plane (G11 3.4, 3.5, 3.6C, Table 3.2 [p. 193, upper]; G12 3.8-3.11; N 338, 340). The pubococcygeus attaches into the coccyx and a median fibrous raphe between the anus and coccyx, the anococcygeal body or ligament. Along its course the most medial fibers insert into midline structures, forming further subdivisions of the muscle. The most important of these attach into the prostate in the male as the puboprostaticus (levator prostatae) (G11 3.4A; G12 3.10; N 341 [labeled “Fibromuscular extensions of levator ani muscle to prostate”]) and the vagina in the female as the pubovaginalis (G11 3.5; G12 3.11; N 339 [labeled “Musculofascial extensions to vagina”]).
The puborectalis muscle is often described as a separate part of the levator ani, but it is better considered as the thickened inferomedial portion of the pubococcygeus, which mostly hides it from view on the pelvic surface (Figs. 5B-D; G11 3.6, 3.7B; G12 3.15; N 337, 339, 341). The puborectalis passes posteriorly from the body of the pubis and meets the contralateral muscle behind the anorectal junction. The right and left puborectalis muscles thus form a muscular sling that is responsible for the anorectal (perineal) flexure. Tonic contraction of the U-shaped puborectalis muscles is important in maintaining fecal continence, and they must relax for defecation to occur.
The iliococcygeus is the posterior part of the levator ani (G11 3.4, Table 3.2 [p. 193, upper]; G12 3.9, 3.10; N 337-341). It arises from the tendinous arch of the levator ani and the ischial spine and inserts into the coccyx and anococcygeal ligament. The iliococcygeus is thin and may be mostly aponeurotic.
Joining the levator ani to form the pelvic diaphragm is the coccygeus muscle (formerly the ischiococcygeus) (G11 3.4; Table 3.2 [pp. 192-193]; G12 3.8-3.11; N 337-341). It is a triangular muscle passing from the ischial spine to the lateral aspect of the lower sacrum and coccyx; however, it may be predominantly tendinous with few skeletal muscle fibers. The coccygeus covers the pelvic surface of the sacrospinous ligament.
The pelvic diaphragm provides dynamic support for the abdominopelvic viscera. The diaphragm is tonically contracted most of the time and helps to maintain urinary and fecal continence. It actively contracts to provide additional support during increases in intra-abdominal pressure (e.g., coughing, sneezing, heavy lifting). The puborectalis portion of levator ani is especially important for fecal continence. The levator ani and coccygeus receive 
innervation on their pelvic surface from the anterior rami of spinal nerves S3 and S4, mostly S4. The puborectalis often receives an additional branch from the pudendal nerve in the ischioanal fossa.
Injury to the pelvic diaphragm during childbirth may result in urinary or fecal incontinence. Alternatively, the pelvic musculature in older women may atrophy as estrogen levels decline or the pelvic floor may be weakened in collagen diseases (e.g., Marfan disease). The uterus or other organs may be pushed downward (prolapse) by increased intra-abdominal pressure due to the pelvic diaphragm’s weakness (e.g., the uterus prolapes into the vagina). It’s no surprise, therefore, that uterine prolapse is most common in multiparous and postmenopausal women. For example, see http://www.emedicine.com/Med/topic3291.htm
Pelvic fascia is connective tissue that fills the space between the parietal peritoneum of the peritoneal sac and the walls and floor of the pelvis. Descriptions of the pelvic fascia are complicated and vary from reference to reference, but basically the fascia is divided into parietal pelvic fascia, visceral pelvic fascia, and subperitoneal fascia (Fig. 6, inset; G11 3.13C; G12 3.22C). Parietal pelvic fascia lines the inner (pelvic) surfaces of muscles forming the walls and floor of the pelvis and is continuous superiorly with transversalis fascia and iliopsoas fascia of the abdomen. Specific regions of the parietal fascia are named for the muscles that they invest (e.g., obturator fascia) (G11 3.4A; G12 3.10).
Thickened bands of parietal pelvic fascia, the tendinous arches of pelvic fascia, run bilaterally from the pubis to the sacrum along the pelvic floor adjacent to the viscera (Fig. 6, pink; G11 3.4A, 3.41; G12 3.10, 3.45; N 345). The most anterior part of the tendinous arch connects the pubis to the prostate in the male (puboprostatic ligament [G11 3.6A, 3.14C, 3.19A; G12 3.15A, 3.14B, 3.28A]) or to the base of the bladder in the female (pubovesical ligament [G11 3.41; G12 3.45; N 345, 348 (Superior view)]). The most posterior part of the tendinous arch passes from the prostate or vagina to the sacrum as the sacrogenital ligament (the uterosacral ligament in the female and the rectoprostatic ligament in the male).
Visceral pelvic fascia is a membranous layer directly covering pelvic organs, forming an adventitial layer for each (Fig. 6, inset; G11 3.13C; G12 3.22C). The visceral and parietal layers become continuous where organs penetrate the pelvic floor.
Subperitoneal fascia is the inferior continuation of the extraperitoneal connective tissue that lines the abdominal cavity outside the peritoneum (e.g., between parietal peritoneum and transversalis fascia). Subperitoneal fascia is described differently by different authors but probably is best considered as extraperitoneal connective tissue that is located between parietal and visceral pelvic fasciae (Fig. 6, inset). The subperitoneal fascia varies substantially in density and content. Some is loose areolar or fatty connective tissue, which creates potential spaces that can be bluntly dissected during surgery (e.g., the potential retropubic space between the pubic symphysis and urinary bladder [G11 3.7A, 3.14C, 3.19A, 3.27; G12 3.14A, 3.14B, 3.20, 3.13A (3.32A); N 346, 348 (midsagittal section)]).
Other areas of subperitoneal fascia are fibrous in consistency and may contain scattered smooth muscle fibers in addition to plentiful collagen and elastic fibers. Nerves and blood vessels
course through these fascial condensations, which are termed “pelvic ligaments.” The ligaments aren’t grossly obvious, but they are palpable. The main fascial condensation extending from the lateral pelvic wall to pelvic viscera is the hypogastric sheath (Fig. 6, green; G11 3.13A; G12 3.22A). It is subdivided into three laminae. The anterior lamina passes to the bladder as the lateral ligament of the bladder, containing superior vesical arteries and veins (Fig. 6; G11 3.15A & C, 3.41A; G12 3.23A & C, 3.45A; N 345). The posterior lamina passes to the rectum as the lateral rectal ligament, carrying the middle rectal artery and vein (Fig. 6).
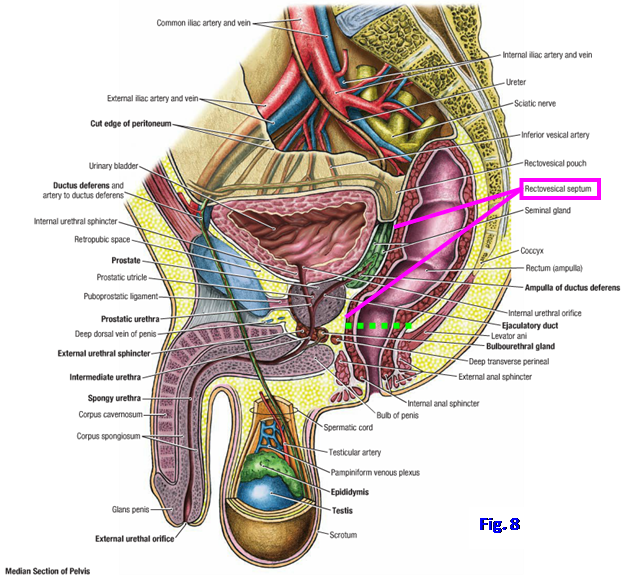
The middle lamina of the hypogastric sheath in males is the relatively thin rectovesical septum (Fig. 8; G11 3.7A, 3.19A; G12 3.14A, 3.20; N 346 [labeled “Rectoprostatic”]). It separates the posterior surface of the bladder and prostate in front from the anterior surface of the rectum behind. In females the middle lamina of the hypogastric sheath is more substantial. It passes medially from the lateral wall of the pelvis to the cervix of the uterus and upper vagina as the transverse cervical ligament or cardinal ligament (Figs. 6 and 7, inset; G11 3.41; G12 3.45; N 345). Clinically it is called the lateral cervical (Mackenrodt’s) ligament. The uppermost portion of the transverse cervical ligament is located within the base of a fold of peritoneum, the broad ligament of the uterus, and carries the uterine artery toward the cervix (Fig. 7, inset; N 352, 354 [upper]).
The ureter passes immediately below the uterine artery en route to the bladder, and this relationship (“water passing under the bridge”) is clinically important during surgical removal of the uterus (hysterectomy). The transverse cervical ligament is the main ligamentous support of the uterus, as will be discussed when the uterus is described.
10. In order to study the pelvic organs and their relationships, it is necessary to bisect the pelvis and perineum and detach one lower extremity. On EVEN-NUMBERED TABLES we will remove the RIGHT lower extremity, and on ODD-NUMBERED TABLES we will remove the LEFT lower extremity. The mobilized kidney, if it was not removed from the body during the last lab period, will be left attached to the half of the pelvis to be removed. Tie a string around the testicular or ovarian vessels on the side where the lower extremity is to be removed. Cut them above the string near the level of the iliac crest. On the same side cut the common iliac artery and vein near the level of the iliac crest.
12. For all tables, use a sharp (new) scalpel blade to make the midsagittal cut through the pelvic and perineal viscera described below.
13. IN THE MALE CADAVER, bisect the penis in the midline posteriorly to the pubic symphysis. Saw through the pubic symphysis and gently separate the two pubic bones. Next use a scalpel to make a cut through all of the pelvic and perineal viscera as close to the midline as possible. Upon reaching the rectum try to cut it and the anal canal in the midsagittal plane and place any contents in the tissue bucket. Be careful not to cut through the ureters, ductus deferentes, or superior or inferior vesical arteries, which are located lateral to the midline.
14. IN THE FEMALE CADAVER, make a midline cut through the soft tissues (mons pubis) superficial to the pubic symphysis and then saw through the symphysis. Gently separate the right and left pubic bones. Use a scalpel to make a midline cut through all of the pelvic and perineal viscera in the midline. Upon reaching the rectum try to cut it and the anal canal in the midsagittal plane and place any contents in the tissue bucket. Be careful not to cut the ureters, uterine arteries and veins, and ovaries, which are located lateral to the midline.
15. In BOTH MALES AND FEMALES retract the aorta and inferior vena cava away from the side of the lower extremity to be removed. Use a handsaw to saw along the midline from inferior to superior through the coccyx, sacrum, vertebra L5, the L4/5 intervertebral disc, and into the body of L4. The lower body of the cadaver may have to be elevated on 4” x 4” wooden blocks to do this. On the side with the extremity to be detached use a scalpel to make a transverse cut just ABOVE the iliac crest through the soft tissues of the abdominal wall and the back medially as far as the vertebral column. Saw horizontally through the body of Lv4 transversely until you meet the preceding vertical cut. Detach the freed lower quadrant. It may be carried to the nearest sink to wash out the rectum at the faucet with the waste disposal.
16. At DR. ROQUE’S TABLES ONLY (i.e., Tables 1-5), the rectum will be completely removed from one half of the bisected pelvis. If the cuts made in bisection of the pelvis deviated to one side of the midline, choose the side with the more intact pelvic organs to remove the rectum. Find where the rectum pierces the pelvic diaphragm (levator ani portion) to become continuous with the anal canal at the anorectal flexure. Cut the rectum horizontally just superior to the pelvic diaphragm (see ![]() in Fig. 8). Cut vessels and nerves to the rectum as close to the lateral side of the rectum as possible. Now remove the freed portion of rectum and set it aside. The pelvic structures exposed by removal of the rectum will be studied during the next period.
in Fig. 8). Cut vessels and nerves to the rectum as close to the lateral side of the rectum as possible. Now remove the freed portion of rectum and set it aside. The pelvic structures exposed by removal of the rectum will be studied during the next period.
SELECTED REFERENCES
McGrath, MC 2004 Clinical considerations of sacroiliac joint anatomy: a review of function, motion, and pain. Journal of Osteopathic Medicine 7(1):16-24.
Prather, H and D Hunt 2004 Sacroiliac joint pain. Disease-a-Month 50:670-683.
Sherman, AL and R Gotlin 2008 Sacroiliac joint injury. http://emedicine.medscape.com/article/96054-overview
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.