Pelvic Organs
The parietal peritoneum of the abdominal cavity continues inferiorly into the pelvic cavity; however, the peritoneum is separated from the floor of the pelvis (pelvic diaphragm) by pelvic organs and the pelvic fascia in which the organs are embedded (G11 2.22A, 3.7A, 3.13, 3.14C, 3.27-3.29; G12 2.19, 3.13, 3.14A-B, 3.22, 3.32, 3.35; N 323, 342, 346). Basically the peritoneum is draped over the tops of pelvic organs as you would drape a sheet over furniture that isn’t to be used for an extended period of time. Of the pelvic organs only the ovaries and uterine tubes of the female are enclosed by peritoneum, and even that description must be qualified. The uterine tubes have openings (ostia) into the peritoneal cavity that are not covered by peritoneum. The epithelial covering of the ovaries, which are suspended by a mesentery, is not the glistening peritoneum seen elsewhere, but those differences are best left for study during histology.
In both males and females, peritoneum is reflected from the anterior abdominal wall onto the superior surface of the bladder. Just superior to the bladder, parietal peritoneum is loosely bound to transversalis fascia by extraperitoneal connective tissue (G11 3.14B; G12 3.21A; N 346). This areolar tissue, which often is laden with fat, allows the bladder to expand between peritoneum and transversalis fascia, separating them as it fills with urine. The loose connective tissue also provides a route of clinical access to the bladder (suprapubic approach) to drain it or to remove a bladder stone or tumor without invading the peritoneal cavity (i.e., an extraperitoneal approach).
In females, peritoneum passes from the superior surface of the bladder a short distance down its posterior surface. In the midline, peritoneum is reflected onto the anterior surface of the body of the uterus and passes upward over the fundus (Fig. 7: G11 3.27, 3.28; G12 3.13, 3.32; N 342, 344). Lateral to the uterus it is draped over the uterine tubes. The peritoneum descends the entire posterior surface of the uterus and onto the posterior vaginal wall before being reflected superiorly onto the middle third of the rectum. Thus peritoneal recesses (pouches or fossae) are formed, one between the bladder and the uterus (vesicouterine pouch) and one between the uterus and rectum (rectouterine pouch) (Fig. 7). The former is shallow and is not related to the anterior vaginal fornix, which is subperitoneal.
The rectouterine pouch (of Douglas) is the most inferior part of the peritoneal cavity in the female (G11 2.22A, 3.27, 3.28; G12 2.19, 3.13, 3.32; N 323, 342, 344). Therefore, blood or infectious fluid in the peritoneal cavity tends to collect there. The rectouterine pouch is closely related to the posterior fornix of the vagina and may be entered through the fornix to drain infectious material (culdocentesis) or for examination of the ovaries or uterine tubes (culdoscopy). Culdoscopy has been largely replaced by laparoscopy.
The double layer of peritoneum that covers the uterus, uterine tubes, and ovaries, extending from one lateral pelvic wall to the other in a roughly coronal plane, is the broad ligament of the uterus (Fig. 7; G11 3.28B, 3.29, 3.30A, 3.32; G12 3.32C, 3.35A-D; N 342-344, 352). The broad ligament is subdivided in relation to these organs (Fig. 7, inset; G11 3.32; G12 3.35B; N 354, 355). The upper part of the broad ligament, which encloses 
the uterine tube within its superior free border, is the mesosalpinx. Extending posteriorly from the broad ligament to enclose the ovary is a roughly horizontal shelf of peritoneum, the mesovarium. Within the medial edge of the mesovarium, connecting the ovary to the body of the uterus near the uterine tube, is a fibrous cord, the ovarian ligament (ligament of the ovary) (G11 3.29, 3.30A; G12 3.32D, 3.35C-D; N355). The coronal part of the broad ligament below the level of the mesovarium and lateral to the body of the uterus is the mesometrium (G11 332; G12 3.35B; N355).
In addition to separating the midline vesicouterine and rectouterine pouches, the broad ligament of the uterus also forms a partition separating two more lateral depressions on each side (G11 3.28B; G12 3.32C; N344). The anterior depression is located lateral to the bladder (paravesical fossa) and the posterior one is located lateral to the rectum (pararectal fossa).
Other peritoneal folds in the female include the rectouterine (sacrogenital, uterosacral) folds raised over the uterosacral ligaments (G11 3.38, 3.39A; G12 3.43A-C; N344, 345). These folds, which may be fairly sharp, arc posteriorly from the uterus (actually the base of the broad ligament) lateral to the rectum to reach the sacrum. They form the lateral boundaries of the pararectal fossae.
In males, the absence of a uterus means that there is only one midline peritoneal recess between the bladder and rectum, the rectovesical pouch. This same relationship exists in females who have had a hysterectomy. In males rectovesical (sacrogenital) folds of peritoneum arc horizontally backward from the posterior surface of the bladder to the sacrum (G11 3.8; G12 3.19; N347). They form the lateral boundaries of the pararectal fossae. As in the female, paravesical fossae are present in the male on each side of the bladder, with their depth varying according to the state of distention of the bladder.
1. Study the arrangement of the peritoneum in the pelvis of male and female cadavers. Basically the peritoneum is draped over the pelvic organs. Remember that in a healthy living body, the peritoneal cavity is a potential space. The large peritoneal cavity of a cadaver is artifact or resulted from a pathological condition (e.g., ascites due to portal hypertension) or starvation during life.
2. In the MALE PELVIS, the peritoneum is reflected from the anterior abdominal wall onto the superior surface of the bladder. Look for the median umbilical fold ascending in the midline from the apex of the bladder toward the umbilicus (G11 3.13B; G12 3.22B; N347). It is formed by peritoneum raised over the urachus. From the superior surface of the bladder peritoneum passes laterally onto the wall of the pelvis. Note the depression in the peritoneal cavity on each side of the bladder, the paravesical fossa. It will be shallow unless the bladder is distended. Follow the short course of the peritoneum downward onto the posterior surface of the bladder and then upward onto the front of the rectum. The peritoneal fossa between the bladder and the middle part of the rectum is the rectovesical pouch. Observe that the middle 1/3 of the rectum is covered by peritoneum only anteriorly. The upper 1/3 of the rectum is covered by peritoneum both anteriorly and laterally, while the sigmoid colon is intraperitoneal and suspended by the sigmoid mesocolon. Attempt to verify this.
3. Identify and palpate the rectovesical folds running posteriorly on each side from the bladder to the sacrum, lateral to the rectum. They form the lateral margins of the pararectal fossae, which are peritoneal fossae located on each side of the rectum.
4. In the FEMALE PELVIS, the peritoneum is reflected downward from the anterior abdominal wall onto the superior surface of the bladder. Find the median umbilical fold ascending in the midline from the apex of the bladder toward the umbilicus (G11 3.28B; G12 3.32C; N343). It is formed by peritoneum raised over the urachus. From the superior surface of the bladder peritoneum is reflected upward on each side onto the lateral wall of the pelvis. Look for a paravesical fossa on each side of the bladder. It will be shallow unless the bladder is distended. The peritoneum continues downward on the posterior surface of the bladder and then upward onto the body of the uterus. The shallow peritoneal recess formed between the bladder and the uterus is the vesicouterine pouch. If the uterus is still present, its body (upper 2/3) probably will be angled forward relative to its cervix (anteflexed) (G12 3.69). The uterus likely will also be tipped anteriorly over the bladder (anteverted) and have to be elevated to view the vesicouterine pouch. In an elderly female the uterus may be so atrophied that this is unnecessary. The orientation of the uterus will be studied in more detail later.
5. Follow the peritoneum upward over the fundus of the uterus and down over the posterior surface of the body and cervix of the uterus. The peritoneum continues inferiorly onto the posterior vaginal wall before being reflected upward onto the anterior surface of the middle third of the rectum. Palpate the extent of the deep peritoneal recess between the uterus and rectum, the rectouterine pouch. It is the most inferior part of the peritoneal cavity in the female. In the bisected pelvis, the rectouterine pouch’s close relationship to the posterior fornix of the vagina is apparent.
6. Study the broad ligament of the uterus. It extends from the uterus to the lateral wall of the pelvis on each side, enclosing the uterine tube within its superior free border. This upper part of the broad ligament is the mesosalpinx (Fig. 7, inset; N354, 355). Identify the ovary suspended from the posterior layer of the broad ligament by a mesentery. Palpate the fibrous ligament of the ovary, which attaches the ovary to the superolateral part of the uterus near its junction with the uterine tube. The roughly horizontal shelf of peritoneum passing posteriorly from the broad ligament on each side of the uterus to enclose the ovary and the ovarian ligament is the mesovarium. The vertical part of the broad ligament inferior to the mesovarium and lateral to the body of the uterus is the mesometrium.
7. Find the rectouterine folds passing backward from the uterus toward the sacrum, lateral to the rectum. Palpate the fibrous uterosacral ligaments that give the rectouterine folds substance. The rectouterine folds form the lateral boundaries of the pararectal fossae. XXX
PELVIC ORGANS (PELVIC VISCERA)
The pelvic viscera include the urinary bladder and terminal parts of the ureters, internal genital organs, and the distal part of the alimentary tract. The urinary bladder is a hollow organ with a muscular wall and is capable of substantial enlargement (distention). It is the temporary reservoir for urine transported from the kidneys by the ureters (G11 2.82D; G12 2.65A; N308 [upper]). The bladder empties through the urethra during micturition.
The ureters and bladder are similar in males and females, but the urethra differs substantially. The ureters are muscular tubes that transport urine from the kidneys to the urinary bladder by peristaltic contractions. They are retroperitoneal with their superior portions within the abdomen and their inferior portions within the pelvis. The ureters cross the pelvic brim near the bifurcation of the common iliac arteries (Fig. 8; G11 2.63A, 3.8, 3.19A-B; G12 2.63A, 3.19, 3.20, 3.28A; N 308, 380, 381), run along the lateral wall of the pelvis, and curve anteromedially to enter the bladder.
The ureters traverse the wall of the bladder obliquely, so that the internal pressure of the filling bladder causes them to close (G11 3.15A, 3.16A; G12 3.23A, 3.24A; N 344, 350, 364). This oblique orientation and contractions of the muscle of the bladder wall during micturition help to prevent reflux of urine into the ureters. This prevents urine from backing up through the ureters to the kidneys, dilating the ureters (hydroureter) and the renal pelves and calyces (hydronephrosis), producing renal atrophy (e.g., see http://emedicine.medscape.com/article/436259-overview and http://www.merckmanuals.com/home/sec11/ch148/ch148b.html ). Urinary obstruction of the bladder or urethra can overcome this protective mechanism to produce hydroureter and hydronephrosis. An obstruction may be due to intrinsic factors (e.g., urinary calculi, prostate cancer) or caused by extrinsic factors (e.g., cancer of the uterine cervix).
The urinary bladder of a child is an abdominal organ (i.e., it is in the abdomen even when empty). The empty bladder of an adult is a pelvic organ (i.e., it is located in the lesser pelvis). As the adult bladder fills, it rises into the abdomen, where it is vulnerable to rupture in abdominal trauma. An empty bladder can be injured in fractures of the bony pelvis.
The empty bladder has an apex, body, fundus, and neck. The apex of the empty bladder points toward the superior edge of the pubic symphysis (Fig. 9A). The median umbilical fold runs upward from the apex to the umbilicus (G11 2.18, 3.13B, 3.28B; G12 2.17, 3.22B, 3.32C; N247, 266, 343, 346 [lower], 347). It is a fold of peritoneum raised over the fibrous urachus (median umbilical ligament), which is a remnant of the embryonic allantois. If the lumen persists (urachal fistula), urine leaks from the umbilicus of the newborn.
The base (fundus) of the bladder is the slightly convex posterior wall located opposite the apex (Fig. 9; N346 [lower], 348 [upper]). The body of the bladder is the major portion located between the apex and base. The body of an empty bladder has a superior surface and two inferolateral surfaces. The neck of the bladder is the inferior part surrounding the origin of the urethra, where the base and inferolateral surfaces meet. The neck is firmly anchored in position by fibrous thickenings of parietal pelvic fascia, the puboprostatic ligaments (from pubic bone to prostate) in males (Fig. 8; G11 3.6A, 3.14C; G12 3.14, 3.15A; N 348 {lower]) and the pubovesical ligaments (from pubic bone to neck of bladder) in females (G11 3.27 and 3.28A [unlabeled], 3.41B; G12 3.13A-B [unlabeled], 3.45A; N 345, 348 [lower]).
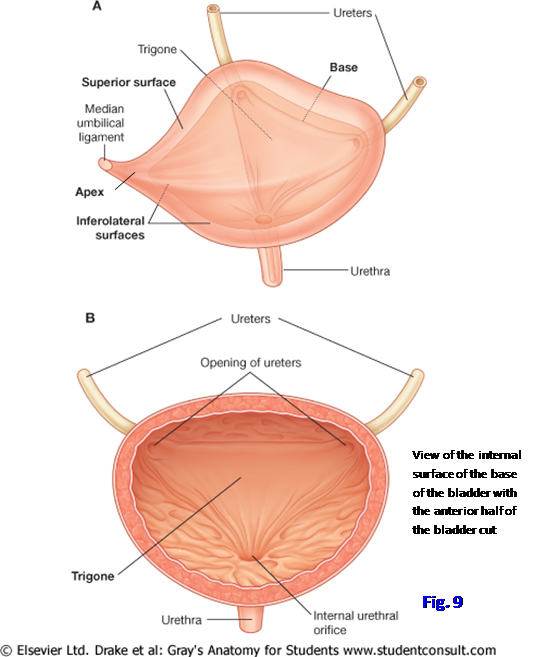
The walls of the bladder are composed mainly of the detrusor muscle (Fig. 9B; G11 3.16; G12 3.24; N350). Near the neck of the bladder in males, the smooth muscle fibers are organized into an involuntary internal urethral sphincter, which is continuous with the fibromuscular tissue of the prostate. This sphincter prevents retrograde ejaculation of semen into the bladder during ejaculation. The presence of an organized internal urethral sphincter in females is controversial; detrusor muscle fibers are continuous with those of the urethra, but some experts advocate the existence of an organized sphincter (N349).
The mucosal lining of the empty bladder is wrinkled except for an area at the base, the trigone, which is always smooth (Fig. 9B; G11 3.16A; G12 3.24A; N346, 348, 350). The trigone has the shape of an inverted triangle and is bounded superolaterally by the openings of the ureters and inferiorly by the internal urethral orifice.
The bladder receives parasympathetic and sympathetic innervation via the inferior hypogastric plexuses (G11 3.25; G12 3.31; N390, 392, 397). The parasympathetic nervous stimulation of the detrusor muscle and inhibition of the internal urethral sphincter cause urine to flow into the urethra when general visceral afferent fibers are stimulated by stretching due to filling of the bladder. Voluntary control of micturition is provided by the pudendal nerves’ innervation of the skeletal muscle external urethral sphincter, which is located mainly within the urogenital diaphragm (deep perineal pouch) of the perineum and will be studied later. Sympathetic nervous stimulation of the internal urethral sphincter prevents retrograde ejaculation and also can inhibit micturition in a nervous male.
Medications that inhibit the sympathetic control of the internal urethral sphincter (e.g., tamsulosin [Flomax] for benign prostatic hyperplasia) allow retrograde ejaculation and may adversely affect a male’s fertility. Retrograde ejaculation also may occur due to peripheral neuropathy in diabetes or following transurethral resection of the prostate.
The urethra carries urine from the internal urethral orifice to the external urethral orifice. The urethra of males and females differs substantially. In males, the urethra is divided into four parts: intramural, prostatic, membranous, and spongy (Fig. 10A; G11 3.7A, 3.14B, 3.19A, 3.51D; G12 3.14A, 3.20, 3.21A, 3.58A; N 346, 365). The short intramural (preprostatic) urethra extends almost vertically through the neck of the bladder, where it is surrounded by the circular smooth muscle of the internal urethral sphincter.
The prostatic urethra descends through the prostate gland (Fig. 10B; G11 3.14B, 3.16; G12 3.21A, 3.24; N 350, 364, 365). It is 3-4 cm long. The posterior wall of the prostatic urethra has a prominent median ridge, the urethral crest, between two grooves, the prostatic sinuses. The middle of the urethral crest has a rounded elevation, the seminal colliculus, which is used as a landmark during transurethral procedures. A shallow pouch in the middle of the seminal colliculus is the prostatic utricle, which is the homologue of the uterus in females. Minute openings on each side of the prostatic utricle are the openings of the ejaculatory ducts. Therefore, the urinary and reproductive tracts in males come together in the prostatic urethra. Secretory ducts of the prostate glands open into the prostatic sinuses. The prostate gland will be considered in more detail with male internal genital organs.
The membranous and spongy urethrae are located in the perineum and will be studied in detail later. For now let it suffice to say that the short membranous urethra traverses the urogenital diaphragm (deep perineal pouch) (Fig. 10B; G11 3.7A; G12 3.14A; N364, 365 [level of “Sphincter urethrae muscle”]). The membranous urethra is surrounded by the external urethral sphincter (sphincter urethrae), which provides voluntary control over micturition. The long spongy (penile) urethra courses through the corpus spongiosum of the penis to open at the external urethral orifice (G11 3.49, 3.51D; G12 3.56, 3.57B; N362, 365).
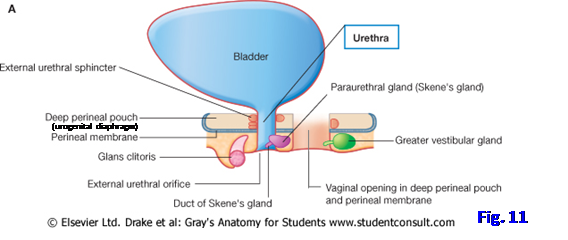
The female urethra is relatively short (Figs. 7, 11; G11 3.27; G12 3.13A; N348, 350). It extends about 4 cm from the internal urethral orifice to the external urethral orifice, which is located within the vestibule of the vagina in the perineum. The urethra descends anterior and parallel to the vagina, which opens into the vestibule immediately behind it. Both the urethra and vagina traverse the urogenital hiatus of the pelvic diaphragm and the urogenital diaphragm (deep perineal pouch). The female external urethral sphincter (sphincter urethrae), which forms part of the urogenital diaphragm and also extends superiorly around the urethra, provides voluntary control of micturition. The urogenital diaphragm will be studied in more detail with the perineum.
The short course of the female urethra and its external opening through the vestibule of the vagina make women more susceptible to bladder infections than men (e.g., see http://www.emedicine.com/EMERG/topic626.htm ). The female urethra’s short, straight course and greater distensibility (due to abundant elastic tissue) can make the passage of catheters or cystoscopes easier in females than males.
The male internal genital organs are the ductus deferentes, seminal vesicles, ejaculatory ducts, and prostate (G11 3.13A-B, 3.14A-B; G12 3.21A-B, 3.22A-B; N346, 364). Each ductus deferens (vas deferens) is a long muscular tube that transports spermatozoa from their storage site in the epididymis to the ejaculatory duct (Fig. 8; G11 3.14A; G12 3.21B; N346, 369, 370). Therefore, the ductus deferens begins at the tail of the epididymis near the inferior pole of the testis and ascends as part of the spermatic cord through the superficial inguinal ring, inguinal canal, and deep inguinal ring. It descends posteromedially from the deep inguinal ring, crossing the external iliac vessels and pelvic brim. The ductus deferens lies just external to, and in contact with, parietal peritoneum as it crosses above the superior vesical arteries, obturator nerve and vessels, and the ureter (G11 3.19A-B; G12 3.20, 3.28A; N347). After crossing the ureter at the posterolateral angle of the bladder, it descends medial to the seminal vesicle. This terminal part of the ductus is enlarged as the ampulla of the ductus deferens, which ends by joining the duct of the seminal vesicle to form the ejaculatory duct (Fig. 12; G11 3.15A & C; G12 3.23; N364).
The seminal vesicles (seminal glands) are accessory reproductive glands. They are located posterior to the base of the bladder, between it and the rectum (Fig. 8; G11 3.14A-C, 3.61D; G12 3.20, 3.21A-B, 3.69; N364) and are palpable in a digital rectal examination. They lie lateral to the ampullae of the ductus deferentes (Fig. 12C). Each seminal vesicle is a highly coiled tube with numerous dilatations and is encapsulated by connective tissue (Fig. 12B; G11 3.15A-B; G12 3.23A-B). The duct of the seminal vesicle joins the ampulla of the ductus deferens to form the ejaculatory duct. The thick alkaline secretions of the seminal vesicles contribute to semen during ejaculation.
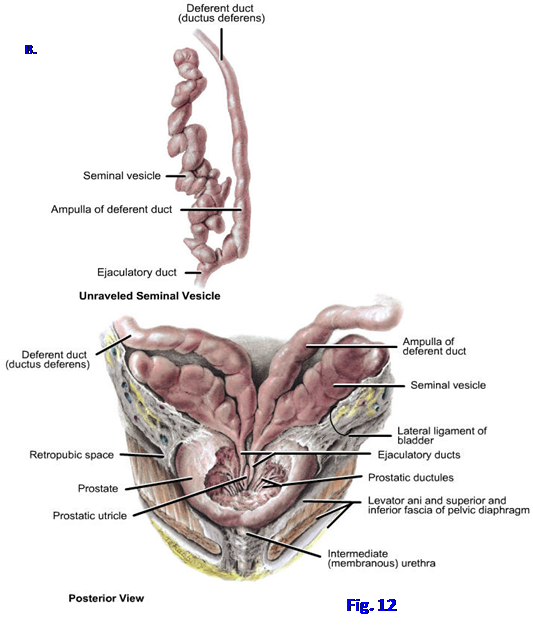 The ejaculatory duct is a slender tube formed by the union of the ampulla of the ductus deferens and the duct of the seminal vesicle (Figs. 8, 11; G11 3.14A-B, 3.15, 3.19A; G12 3.21A-B, 3.23, 3.20; N364, 369). The two ejaculatory ducts pass anteroinferiorly through the posterior part of the prostate gland to open into the prostatic urethra on the seminal colliculus (Fig. 10C; G11 3.16; G12 3.24; N364).
The ejaculatory duct is a slender tube formed by the union of the ampulla of the ductus deferens and the duct of the seminal vesicle (Figs. 8, 11; G11 3.14A-B, 3.15, 3.19A; G12 3.21A-B, 3.23, 3.20; N364, 369). The two ejaculatory ducts pass anteroinferiorly through the posterior part of the prostate gland to open into the prostatic urethra on the seminal colliculus (Fig. 10C; G11 3.16; G12 3.24; N364).
The prostate is an unpaired accessory gland of the male reproductive system that surrounds the part of the urethra immediately below the bladder (prostatic urethra) (Figs. 8, 12C; G11 3.7, 3.14, 3.15C, 3.16, 3.18A; G12 3.14A, 3.21, 3.23C, 3.24, 3.26A; N364, 365). It contains both glandular and fibromuscular components. The prostate has a dense fibrous capsule and outside the capsule is a prostatic sheath formed by the visceral layer of pelvic fascia. The prostatic sheath is continuous anterolaterally with the puboprostatic ligaments, which connect the prostate to the pubis to anchor the neck of the bladder in position (Fig. 8). Between the capsule and the prostatic sheath is the prostatic venous plexus (G11 3.16; G12 3.24; N383), which can be a troublesome source of bleeding during surgical removal of the prostate (prostatectomy).
The prostate traditionally has been divided into lobes, although these aren’t grossly distinct. Although a different system is used clinically to describe the prostate, the traditional anatomical lobes are referred to in articles and monographs, and a physician needs a basic familiarity with them. The anterior lobe of the prostate lies anterior to the urethra and is mostly fibromuscular (i.e., fibrous connective tissue and smooth muscle). The remaining 2/3 of the prostate is glandular. The right and left lateral lobes lie on either side of the urethra and form the major part of the prostate. The posterior lobe lies posterior to the urethra and inferior to the ejaculatory ducts (Fig. 8). The middle (median) lobe is located posterior to the urethra and superior to the ejaculatory ducts. Therefore, it is closely related to the neck of the bladder.
Non-cancerous enlargement of the prostate (benign prostatic hyperplasia, BPH) is common in middle-aged and older males (e.g., see http://www.emedicine.com/MED/topic1919.htm ). The middle lobe (clinically the central or transition zone) usually enlarges the most and compresses the urethra. It may obstruct the internal urethral orifice, producing difficulty initiating urination (hesitancy), sudden urge to void (urgency), difficulty and/or pain during urination (dysuria), and need to void during the night (nocturia). Obstruction of urinary outflow may produce hypertrophy of the detrusor muscle of the bladder and cause an irritable bladder.
Prostate cancer is common in elderly males (60-80% incidence after age 80, depending on the reference). It typically involves the posterior lobe (clinically the peripheral zone; e.g., see http://emedicine.medscape.com/article/1967731-overview#showall ) and, therefore, doesn’t produce symptoms of urinary obstruction until late in the course of the disease. It is diagnosed by digital rectal examination and serum prostate-specific antigen (PSA) tests. Treatment may include partial or total surgical resection of the prostate (prostatectomy). Sometimes this is done transurethrally. An attempt is made to preserve the cavernous nerves so that the patient may retain sexual function.
The prostatic venous plexus deserves additional consideration. It is continuous superiorly with the vesicle venous plexus and drains into the internal iliac veins. Communications posteriorly with the vertebral venous plexus provide a pathway for prostate cancer cells to metastasize to the vertebral column, spinal cord, and brain (e.g., see http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowFulltext&ArtikelNr=95706&ProduktNr=223840 ). The lumbar spine is frequently involved.
The internal genital organs in females include the ovaries, uterine tubes, uterus, and vagina. The ovaries are the sites of oocyte production (oogenesis) and release (ovulation). They are almond-shaped organs, one located on each side of the pelvis near the lateral pelvic wall (Fig. 7; G11 3.27, 3.28B, 3.29, 3.30, 3.35; G12 3.13A, 3.32C, 3.34, 3.35C-D; N342-344, 354, 355). Each ovary is suspended by two peritoneal folds, by the mesovarium from the posterior aspect of the broad ligament and by the suspensory ligament of the ovary from the lateral pelvic wall (G11 3.30A, 3.32; G12 3.35B-D; N354, 355). The surface of the prepubertal ovary is covered by smooth, grayish, dull ovarian surface epithelium, giving it a different appearance than the surrounding glistening peritoneum. In middle-aged and older women, the surface is irregular and scarred from the monthly rupture and discharge of oocytes that occurred during the child-bearing years.
The major ovarian blood vessels, the lymphatics, and the nerves reach the superolateral aspect of the ovary via the suspensory ligament of the ovary (G11 3.27, 3.28B, 3.30A; G12 3.13A, 3.32C, 3.35D; N342-344, 355, 380). The ovarian artery is a branch of the abdominal aorta, reflecting the original embryonic location of the ovary. The ovary’s blood supply from the ovarian artery is supplemented by the ovarian branch of the uterine artery (N384), which will be described with the pelvic blood supply. The right ovarian vein is a tributary of the inferior vena cava, but the left ovarian vein drains into the left renal vein (G11 2.75B; G12 2.75B; N380, 381). The lymphatic vessels follow the arteries back to the lateral aortic (lumbar) lymph nodes (G11 3.37A; G12 3.40B, Table 3.8 [p.245]; N386).
The uterine tubes (oviducts, fallopian tubes) transport the discharged oocyte to the cavity of the uterus. They arise in the superolateral body of the uterus and pass laterally toward the pelvic walls near the ovaries (Fig. 7; G11 3.27, 3.28B, 3.29, 3.30A, 3.32; G12 3.13A, 3.32C, 3.35B-D; N342-344, 354, 355). The uterine tubes occupy the free superior edge of the broad ligament, the mesosalpinx.
Each uterine tube is divisible into four parts: infundibulum, ampulla, isthmus, and uterine part (Fig. 13; G11 3.29, 3.30A; G12 3.35C-D; N 355). The infundibulum is the funnel-shaped distal part near the ovary. It opens into the peritoneal cavity via the abdominal ostium, which is surrounded by finger-like processes, the fimbriae. Thus, the peritoneal cavity is not a closed sac in females (see hysterosalpingograms in G11 3.33B; G12 3.73B; N354). The ampulla is the part of the uterine tube medial to the infundibulum. The ampulla is the longest and widest part of the uterine tube and is the site where fertilization of the oocyte usually occurs. The isthmus is the narrow, relatively thick-walled part of the uterine tube adjacent to the uterus. The uterine (intramural) part of the uterine tube traverses the wall of the uterus to open into the uterine cavity via the uterine ostium (Fig. 13B; G11 3.33B; G12 3.73A; N355).
Ovulation discharges the oocyte from the ovary into the peritoneal cavity, where it is quickly swept by fimbriae and fluid currents into the abdominal ostium of the infundibulum. If the oocyte is fertilized but not collected into the uterine tube, the conceptus may implant within the peritoneal cavity as an ectopic abdominal pregnancy (e.g., see http://www.medscape.com/viewarticle/557082_5 ). Only a few ectopic abdominal pregnancies have been reported to come to term and been delivered by caesarian section. If fertilization occurs within the ampulla of the uterine tube, as it usually does, passage of the zygote down the uterine tube may be blocked by scarring that occurred secondary to pelvic inflammatory disease or other factors. The conceptus then implants in the wall of the uterine tube (ectopic tubal pregnancy). These ectopic tubal pregnancies account for 95% of ectopic pregnancies. They usually end in the second month with a ruptured uterine tube, life-threatening abdominal hemorrhage into the peritoneal cavity, and severe pain. Since the appendix often lies close to the right ovary and uterine tube, a ruptured tubal pregnancy and the resulting peritonitis may be misdiagnosed as acute appendicitis.
The uterus is a thick-walled, hollow muscular organ located in the midline between the bladder and the rectum (Fig. 7; G11 3.27, 3.28, 3.30A, 3.33B; G12 3.13A-B, 3.32A, 3.34A; N 342-344, 352, 355). It consists of a body and a cervix, which meet at a constricted region, the isthmus (Fig. 13; G11 3.33B; G12 3.34A, 3.35D; N355). The uterine tubes join the body of the uterus superolaterally, and inferiorly the cervix joins the vagina.
The body of the uterus forms the upper 2/3 of the organ and includes the rounded fundus superiorly. The body consists of three layers: perimetrium, myometrium, and endometrium. The outer layer is the perimetrium, which consists of peritoneum and a thin layer of connective tissue. The myometrium is the thick middle layer of smooth muscle (G11 3.33A, 3.63C; G12 3.34A, 3.69; N355). The myometrium becomes greatly distended and thinned during pregnancy but then contracts to expel the fetus and placenta during childbirth. The endometrium is the inner layer of the body of the uterus, where the blastocyst implants 5½ - 6 days after conception. The endometrium is actively involved in the menstrual cycle, being mostly sloughed off if conception doesn’t occur.
The cervix of the uterus is the cylindrical lower 1/3 that joins the vagina inferiorly (Fig. 13; G11 3.30A, 3.33B; G12 3.34A, 3.35D; N342, 355). The cervix consists mostly of fibrous connective tissue with small amounts of smooth muscle and elastin. The convex inferior part of the cervix protrudes downward into the vagina, creating a circular recess around the cervix, the fornix of the vagina (Figs. 7, 13B; G11 3.27, 3.33B, 3.35A; G12 3.13A, 3.32A, 3.34A; N342, 355).
The uterus is a hollow organ. The cavity of the body of the uterus is the uterine cavity (Fig. 13B; G11 3.33B, 3.35A; G12 3.34A, 3.73A-B; N355). It is continuous superolaterally on each side with the lumen of a uterine tube. Inferiorly the uterine cavity is continuous at the internal os (internal ostium) with the canal of the cervix, the cervical canal. The cervical canal opens into the lumen of the vagina at the external os (external ostium). The uterine cavity, cervical canal, and lumen of the vagina form the birth canal, through which the fetus passes at childbirth.
The adult uterus in most women maintains a particular posture that contributes to its support. The uterus usually is tilted anteriorly relative to the axis of the vagina (anteversion) and the body of the uterus is also angled anteriorly relative to the cervix of the uterus (anteflexion). The bladder passively supports the anteverted, anteflexed uterus (Fig. 7; G11 3.27, 3.63C; G12 3.13, 3.69; N342, 348).
The other main passive supports of the uterus in the pelvis are the transverse cervical (cardinal) ligaments, but the uterosacral ligaments also contribute (Fig. 6; G11 3.41; G12 3.45; N345, 355). A fibromuscular mass in the perineum, the perineal body, lends important support to the uterus and other pelvic organs by providing for muscle attachments, including the levator ani (G11 3.55; G12 3.36, 3.63A; N 348 [midsagittal section], 357, 358). The perineal body will be studied with the perineum. Dynamic support of the uterus is provided by the pelvic diaphragm, which actively contracts during periods of increased intra-abdominal pressure (e.g., coughing). These passive and dynamic supports resist a tendency for the uterus to fall or be pushed downward through the vagina (uterine prolapse). A uterus that is more vertically oriented than usual (e.g., retroverted and retroflexed) lacks the support of the bladder and is more prone to prolapse.
Ligaments of the uterus that do not provide significant support include the ligament of the ovary and the round ligament of the uterus (Figs. 7, 13A; G11 3.29, 3.30A, 3.32; G12 3.35A-D; N342-344, 352, 355). The ligament of the ovary (ovarian ligament) passes posteriorly, inferiorly, and laterally to the ovary from near the uterotubal junction. The round ligament of the uterus runs anterolaterally from the uterotubal junction. The ligament of the ovary and the round ligament of the uterus are remnants of the gubernaculum, which attached the ovary to the genital swelling in the embryo. The gubernaculum is involved in descent of the ovary into the pelvis from its original position on the posterior abdominal wall of the embryo.
The vagina is a distensible fibromuscular tube that runs inferiorly from the cervix to the vestibule of the vagina, which is a cleft between the labia minora (Fig. 7; G11 3.27, 3.35; G12 3.32A, 3.34A; N342, 352). The vagina traverses the urogenital hiatus of the pelvic diaphragm and pierces the urogenital diaphragm (deep perineal pouch) (Fig. 11), which fills the urogenital hiatus and will be studied in the perineum dissection. The vagina is usually collapsed with an “H” shape in cross section, except superiorly near the cervix at the vaginal vault.
The lumen of the vagina communicates above with the cervical canal through the external os. The upper recess of the vagina that surrounds the convex vaginal part of the cervix is the vaginal fornix (Figs. 7, 13B; G11 3.33B; G12 3.32A, 3.34A; N342, 355). It is subdivided by position into anterior, posterior, and lateral fornices. The posterior fornix of the vagina is potentially important clinically because of its close relationship to the rectouterine pouch (Fig. 7; G11 3.27; G12 3.13; N 342), as discussed previously.
The vagina is related anteriorly to the base of the bladder and the urethra (Fig. 7; G11 3.27, 3.28A; G12 3.13A, 3.13B; N342, 348, 349). Posteriorly it is related mainly to the rectum. Traumatic tears in the anterior vaginal wall (e.g., iatrogenic tears) or disease processes that cause tissue breakdown may result in the formation of open communications (fistulas) between the lumen of the vagina and the bladder (vesicovaginal fistula) or the urethra (urethrovaginal fistula). Urine then escapes from the vagina. If a fistula forms between the vagina and the rectum (rectovaginal fistula), fecal matter may be discharged from the vagina. A weakening of the walls of the vagina without an open communication may result in prolapse of the bladder (cystocele), urethra (urethrocele), or rectum (rectocele) into the vagina.
The rectum is the part of the alimentary tract distal to the sigmoid colon (G11 2.26, 2.41A, 3.7, 3.8, 3.10, 3.19; G12 2.37A, 3.14A, 3.16, 3.19, 3.20; N263, 276, 323, 371-374). Their junction, the rectosigmoid junction, is located anterior to the third sacral vertebra. The rectum follows the curvature of the sacrum inferiorly to the pelvic diaphragm, where it is continuous with the anal canal at the anorectal (perineal) flexure created by the pull of the puborectalis muscle (Fig. 7; G11 3.6B; G12 3.15B; N337, 371). The anal canal is located in the perineum and will be described with it.
In males the rectum is related to the base of the bladder, seminal vesicles, ampullae of the ductus deferentes, and prostate gland (Figs. 8, 12C; G11 3.19A, 3.61D; G12 3.20, 3.69). An upper part of the rectum is related to the rectovesical pouch. This close relationship to other pelvic structures allows palpation of the prostate and seminal vesicles during a digital rectal examination in the male. An annual examination plays a key role in the early detection of prostate cancer. In females, the rectum is related anteriorly to the rectouterine pouch, cervix, and posterior wall of the vagina (G11 3.27, 3.28; G12 3.13, 3.32C; N342). A digital rectal examination may be used to palpate those structures, as well as the ischial spines, and ischial tuberosities.
The rectum has three lateral curvatures during its course (Fig. 14; G11 2.41A, 3.10A; G12 2.37A, 3.16; N373, 374). The superior and inferior curvatures are convex to the right and the middle curvature is convex to the left. Each curvature is formed opposite a semilunar infolding of the rectal wall into the lumen (transverse rectal fold, valve of Houston [G11 3.10C; G12 3.17A; N373]) formed by mucosa, submucosa, and a thickening of the circular smooth muscle layer (e.g., the middle curvature to the left is opposite a transverse rectal fold on the right side of the rectum). The transverse rectal folds are presumed to help support the contents of the rectum. The dilated terminal part of the rectum, supported on the pelvic diaphragm, is the rectal ampulla.
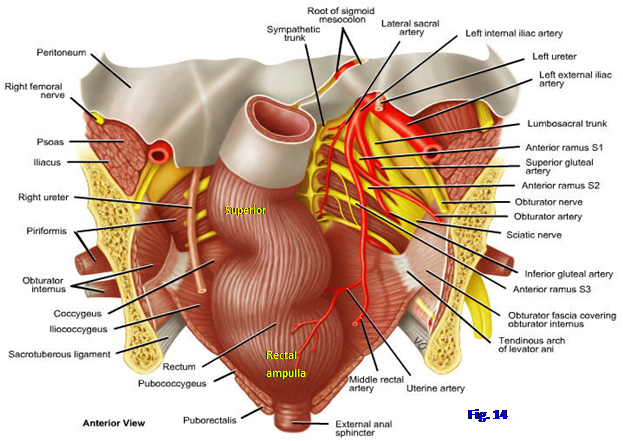
The peritoneal relationship of the rectum changes during its course. The upper third of the rectum, which is continuous with the intraperitoneal sigmoid colon, is covered by peritoneum on its anterior and lateral surfaces (G11 3.10A, 3.14C; G12 3.14B, 3.16; N371). The middle third is covered only anteriorly. The lower third of the rectum is below the peritoneal sac (subperitoneal) and is not in contact with peritoneum.
8. IN THE MALE CADAVER pull the apex of the hemisected urinary bladder backward from the body of the pubis to expose the potential retropubic space. Look for a tough white fascial band running from the body of the pubis to the neck of the bladder. This is the puboprostatic ligament. Clean the interior of the bladder and identify the ureteric orifice. The two ureteric orifices and the internal urethral orifice of the intact bladder outline a triangular smooth area, the trigone. Identify the half of the trigone remaining in the hemisected bladder.
9. Study the prostatic urethra and attempt to identify the features of its posterior wall, including the urethral crest, seminal colliculus, prostatic utricle, and prostatic sinus (G11 3.16; G12 3.24; N364, 365). Look for the pinpoint opening of the ejaculatory duct on the seminal colliculus lateral to the prostatic utricle. If the bisection of pelvic organs was off center, you may need to take scissors and trim away prostate tissue to open the prostatic urethra beginning superiorly at the internal urethral orifice. Is there enlargement of the prostate (benign prostatic hyperplasia) distorting the internal urethral orifice and prostatic urethra? A hard irregular mass may indicate prostate cancer.
10. Examine the rectovesical pouch. Then remove and discard the peritoneum from the pelvic cavity. Clean the ductus deferens and follow its course from the deep inguinal ring across the pelvic brim toward the bladder. It passes superior to the superior vesical artery, obturator nerve and vessels, and the ureter. Note the dilated terminal portion of the ductus deferens, the ampulla of the ductus deferens (Fig. 12C). Just lateral to the ampulla clean the lobulated seminal vesicle. Find the pelvic portion of the ureter and follow it to the bladder.
11. Study the rectum and its relationship to the bladder, prostate, ampulla of the ductus deferens, and seminal vesicle. Identify a transverse rectal fold. Can you identify the perineal flexure? the cut edge of the puborectalis muscle? If the right lower quadrant was removed in your cadaver, clean the superior rectal artery descending from the inferior mesenteric artery, which should have been preserved. The accompanying superior rectal vein drains into the portal system of veins.
12. IN THE FEMALE CADAVER pull the apex of the hemisected urinary bladder backward from the body of the pubis to expose the potential retropubic space. Look for a tough white fascial band running from the neck of the bladder to the inner surface of the body of the pubis. This is the pubovesical ligament. Clean the interior of the hemisected urinary bladder and identify the ureteric orifice. The two ureteric orifices and the internal urethral orifice outline a triangular smooth area, the trigone of the bladder. Identify the half of the trigone remaining in one-half of the bladder. Notice that the urethra and base of the bladder are related to the anterior wall of the vagina. Verify that the base of the bladder is separated from the uterus superiorly by the vesicouterine pouch.
13. The female urethra courses roughly parallel to the vagina to open into the vestibule between the labia minora. Follow the urethra inferiorly from the internal urethral orifice. Realize that the urethra’s short course and external opening in the vestibule predispose to the development of urinary tract infections.
14. The uterus is usually angled anteriorly on the vagina (anteversion), and the body of the uterus usually is flexed anteriorly on the cervix (anteflexion), but this may be less apparent in an atrophied postmenopausal organ. Examine the uterine cavity and the ostium of the uterine tube. Identify the cervical canal with the external and internal ostia. If the bisection of pelvic organs was off center, you may need to use scissors to trim away part of the cervix to expose the cervical canal.
15. Study the uterine tube and find where its lateral fimbriated end turns downward and backward over the ovary. Find the abdominal ostium of the tube and realize that this is normally the only opening into the peritoneal cavity. Just below where the uterine tube joins the uterus, find ligaments diverging anterolaterally and posterolaterally from the uterus and covered by the broad ligament. The anterior ligament is the round ligament of the uterus. Follow it toward the deep inguinal ring. The posterior ligament is the ligament of the ovary, which occupies the medial edge of the mesovarium. Realize that the round ligament of the uterus and the ligament of the ovary are remnants of the gubernaculum, which was involved in descent of the embryonic ovary. Examine the ligament of the ovary. The surface of the ovary is probably scarred and irregular.
16. Study the rectouterine pouch and its relationship to the posterior fornix of the vagina. In many elderly cadavers, the uterus will have been surgically removed (hysterectomy) so that there is essentially a rectovesical pouch as seen in males.
17. Study the rectum and its relationship to the cervix and the posterior fornix of the vagina. Identify a transverse rectal fold. Is the perineal flexure recognizable in this cadaver? the cut edge of the puborectalis muscle? If the right lower quadrant was removed in your cadaver, clean the superior rectal artery descending from the inferior mesenteric artery, which should have been preserved. The accompanying vein drains into the portal system of veins. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.