Perineum
The perineum is the most inferior region of the trunk. It is a shallow compartment located between the proximal parts of the thighs and contains the external genitalia and the external openings of the urogenital and gastrointestinal systems. Although many structures of the perineum are difficult to demonstrate in a traditional dissection, a good conceptual understanding of the region is important for the practicing physician.
The perineum is separated from the pelvic cavity above by the pelvic diaphragm (Fig. 1; G11 3.2B; G12 3.3; N323, 342, 346). The perineum fills the pelvic outlet (Fig. 2A) and is covered below (i.e., superficially) by skin and superficial fascia. It is diamond-shaped when the thighs are abducted and is bounded by the pubic symphysis in the anterior midline, the ischiopubic rami anterolaterally, the ischial tuberosities laterally, the sacrotuberous ligaments posterolaterally, and the coccyx in the posterior midline. Each sacrotuberous ligament is covered superficially by the gluteus maximus muscle of its side. The pelvic outlet of the female is the inferior limit of the bony birth canal traversed by the fetus during a vaginal birth.
The perineum is subdivided into two triangular regions—the anal triangle and the urogenital triangle—by an imaginary transverse line connecting the two ischial tuberosities (Fig. 2). The two triangles lie in different planes, which is apparent when studying the skeleton of a pelvis. The anal triangle is the posterior triangle. With the pelvis in the anatomical position the anal triangle lies in an oblique plane, facing posteroinferiorly. It contains the anal canal and anus surrounded by fat.
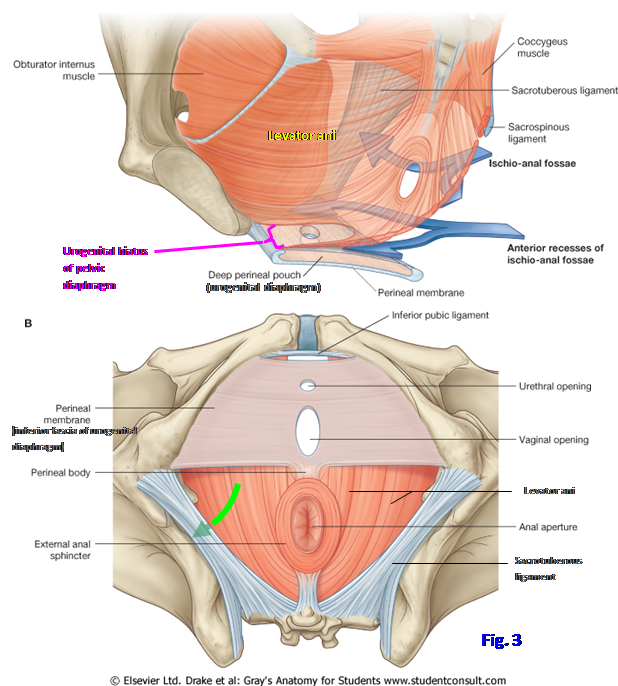
The urogenital triangle is the anterior triangle of the perineum and lies in a nearly horizontal plane. It occupies the region between the right and left ischiopubic rami and contains the fibromuscular urogenital diaphragm, which includes a tough inferior fascia, the perineal membrane (Fig. 3; G11 3.4, 3.6C; G12 3.9, 3.10, 3.15; N340). The urogenital diaphragm closes the midline urogenital hiatus of the pelvic diaphragm from below, except where structures traverse it, the urethra in both sexes and the vagina in the female (Fig. 3A). The urogenital diaphragm thus helps to support pelvic organs in the anterior midline, such as the prostate in the male. It also provides attachment for erectile bodies of the external genitalia. Erectile bodies are present in both males and females.
At the midpoint of a line joining the two ischial tuberosities is an irregular fibromuscular mass, the central tendon of the perineum. It is referred to in obstetrics as the “perineal body,” and that term is also commonly used for males (G11 3.42E, 3.44, 3.55; G12 3.48E, 3.51, 3.63; N348, 349, 358, 362). The perineal body lies deep to a thin layer of subcutaneous connective tissue and is difficult to demonstrate in dissection, except by palpation, but it is important in the integrity of the pelvic floor and the perineum because several muscles converge to attach there, along with the perineal membrane (G11 3.44, 3.51B; G12 3.51, 3.57A; N357, 358, 362, 375). These structures will be discussed in some detail later.
The perineal body is clinically important in women because it functions along with pelvic fascial ligaments (e.g., the transverse cervical ligament) and the levator ani muscle to support pelvic organs. If the perineal body is stretched or torn during childbirth, the pelvic floor is weakened and prolapse of pelvic organs, such as the uterus, may occur. In an effort to avoid tearing of the perineal body during childbirth, a surgical incision may be made to enlarge the vaginal orifice (episiotomy), either through or lateral to the perineal body. An incision made partially through the perineal body is thought to resist further tearing and to heal better than a jagged traumatic tear would but has its own associated risks (e.g., see http://www.jabfm.org/content/18/1/8.full ).
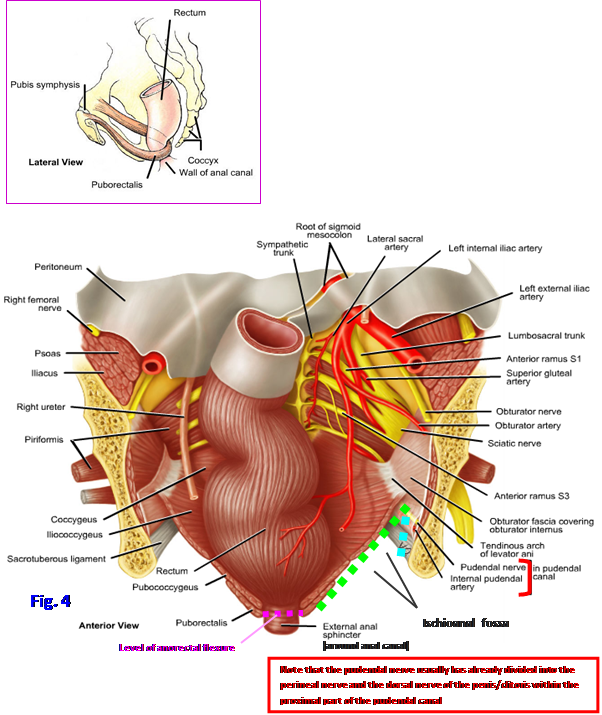
The anal triangle is the posterior triangle of the perineum. It contains the centrally located anal canal and its external opening, the anus, positioned between two spaces (Fig. 4; G11 3.10A, 3.44, 3.55; G12 3.16, 3.51, 3.63; N358, 362, 372). The anal canal is continuous above with the rectum at the pelvic diaphragm, where the pull of the puborectalis muscle produces the anorectal (perineal) flexure (Fig. 4, inset; G11 3.6B-C; G12 3.14A, 3.15A-B; N337, 339, 341, 371). The funnel shape of the pelvic diaphragm creates a wedge-shaped space, the ischioanal fossa (formerly the ischiorectal fossa), on each side in the anal triangle (Fig. 4; G11 3.13C, 3.53, 3.55, 3.56, 3.60D-E, 3.62C-E; G12 3.22C, 3.59, 3.61, 3.63, 3.66D-E, 3.70C-F; N357, 358, 372). The medial wall of the ischioanal fossa is the sloping levator ani muscle ( - - - - - - ). The nearly vertical lateral wall of the fossa ( - - - - - - ) is formed by the ischium and the part of the obturator internus muscle located below the tendinous arch of the levator ani. The obturator internus is covered by obturator fascia. Anteriorly on each side is a short extension of the ischioanal fossa above the urogenital diaphragm, the anterior recess of the ischioanal fossa (Fig. 3A; G11 3.56; G12 3.49B & D [labeled “Ischioanal fossa”]; 3.61; N350, 352, 376).
Each ischioanal fossa is filled with fat (ischioanal fat pad) and loose connective tissue (G11 3.53, 3.57, 3.59B; G12 3.59, 3.64, 3.65B; N357, 360, 372), and the two fossae communicate behind the anal canal via the deep postanal space (N376). Therefore, an ischioanal infection (e.g., due to an anal fistula [see http://www.emedicine.com/med/topic3532.htm ] or resulting from a penetrating wound to the anal triangle) may spread from one ischioanal fossa through the postanal space to the other ischioanal fossa. The ischioanal fat pads are among the last fat reserves in the body to disappear with starvation, and the loss of their support predisposes to rectal prolapse. However, there are multiple possible causes of rectal prolapse (see http://emedicine.medscape.com/article/196411-overview ).
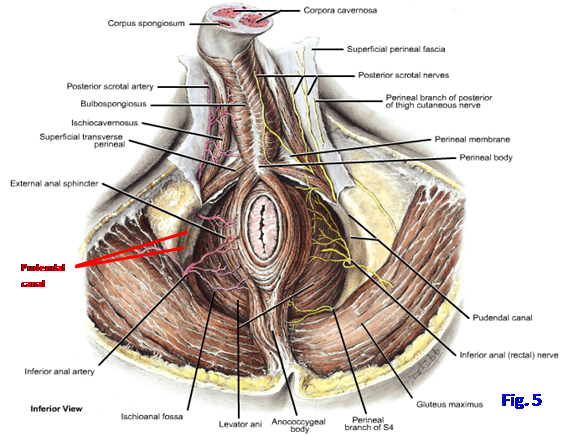
The obturator fascia on the lateral wall of the ischioanal fossa splits to form a narrow passageway for neurovascular structures, the pudendal canal (Alcock’s canal) (Figs. 4, 5; G11 3.10A, 3.13C, 3.44; G12 3.16, 3.22C, 3.51; N372, 378, 384, 385). The internal pudendal artery and vein and branches of the pudendal nerve traverse the pudendal canal en route to the urogenital triangle. They are the main blood and nerve supply to the perineum and will be considered in more detail with the urogenital triangle.
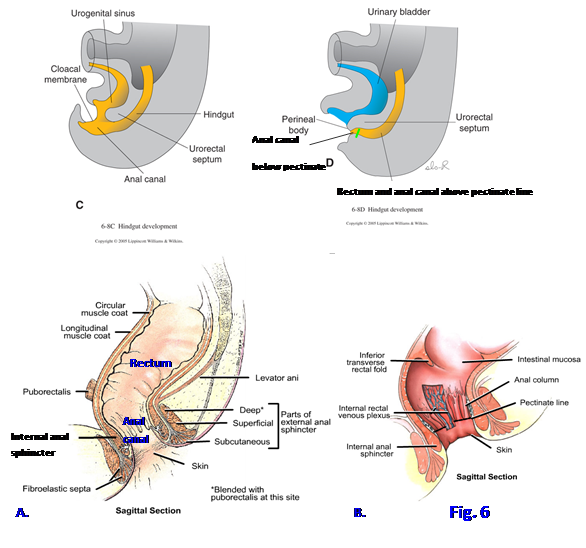
The anal canal is the terminal portion of the large intestine. It begins at the anorectal (perineal) flexure, where it is continuous with the rectum (Fig. 4; G11 3.6, 3.7, 3.9, 3.10A; G12 3.14-3.16; N346, 348, 371-374). The anal canal is surrounded by two sphincters, the internal and external anal sphincters. The internal anal sphincter surrounds the upper 2/3 of the anal canal. It is a thickening of the circular layer of smooth muscle of the intestine and, therefore, is involuntary. The internal anal sphincter stays tonically contracted under control of the sympathetic nervous system, except during defecation. The parasympathetic nervous system inhibits contraction of the internal anal sphincter and promotes peristalsis during defecation.
The external anal sphincter surrounds the lower 2/3 of the anal canal (Figs. 4, 5, 6A; G11 3.6A & C, 3.7A, 3.9, 3.10A, 3.19A, 3.44, 3.45; G12 3.14A, 3.15A & C-D, 3.16, 3.20, 3.51, 3.52A; N371-375). It is formed mainly by circular layers of skeletal muscle but also sends fibers to attach anteriorly to the perineal body and posteriorly to the coccyx. Superiorly it blends with the puborectalis muscle (N371). The external anal sphincter is described as having subcutaneous, superficial, and deep parts, but these often are indistinct and difficult to demonstrate in dissection. The external anal sphincter is supplied by inferior rectal (anal) branches (mainly S4) of the pudendal nerve, which is formed from the anterior rami of S2-4. The external sphincter acts with the puborectalis to provide voluntary control of defecation. Tearing of the external anal sphincter or stretching of the pudendal nerve to produce a nerve lesion during a traumatic childbirth may result in fecal incontinence.
Internally, the mucous membrane of the upper half of the anal canal features a series of longitudinal ridges, the anal columns (Fig 6B; G11 3.7A, 3.9B; G12 3.14A, 3.15C-D; N372, 373). The anal columns contain the terminal branches of the superior rectal arteries and veins (G11 3.10B-C; G12 3.17A; N373, 378, 379). The internal rectal venous plexus is of particular importance. The inferior ends of the anal columns are connected by crescentic folds of mucosa, the anal valves. Just above the anal valves are small recesses, the anal sinuses, which contain mucus glands.
The anal valves around the circumference of the lumen form an irregular line, the pectinate (dentate) line (Fig. 6B; G11 3.9B; G12 3.15D; N373). The pectinate line indicates the junction between the superior part of the anal canal, which developed from hindgut endoderm, and the inferior part, which developed from ectoderm of the proctodeum. This has implications for the blood supply, lymphatic drainage, and innervation. Above the pectinate line the anal canal receives blood from the superior rectal artery (inferior mesenteric) and drains mainly through the superior rectal veins into the portal system of veins (G11 2.60, 2.61A, 3.21B; G12 2.60, 2.61A, 3.29; N288, 292, 378, 379). The lymphatic drainage follows the superior rectal and inferior mesenteric arteries back to inferior mesenteric nodes, although some may follow the middle rectal arteries to the internal iliac nodes as well (N296). The nerve supply is from general visceral afferent (GVA) fibers, and so the mucosa is stimulated by stretch but relatively insensitive to pain and temperature.
Below the pectinate line the anal canal is supplied by the inferior rectal arteries (internal pudendal) (G11 3.10B-C, 3.44; G12 3.17A, 3.51; N288, 378, 384, 385). Venous blood drains through the inferior rectal veins and internal pudendal veins toward the inferior vena cava. The middle rectal veins mainly drain the muscular wall of the rectum and anal canal toward the internal pudendal veins. The lymphatic drainage inferior to the pectinate line goes to the superficial inguinal lymph nodes (G11 3.12; G12 3.17B; N387). The nerve supply is general somatic afferent (GSA) from the pudendal nerve. Therefore, mucous membrane below the pectinate line is sensitive to pain and temperature.
 At the pectinate line tributaries of the portal and inferior vena caval systems anastomose. In portal hypertension these portacaval anastomoses and superior rectal veins become dilated to form internal hemorrhoids (G11 2.61, 3.21B; G12 3.29; N291, 292, 379). It is important to remember, however, that internal hemorrhoids in the majority of patients are not due to portal hypertension (see http://www.emedicine.com/emerg/topic242.htm ). Internal hemorrhoids may prolapse through the anal canal and be compressed by contraction of the anal sphincters, impeding blood flow and resulting in strangulation and ulceration. A subcutaneous plexus of the inferior rectal veins around the anus may become thrombosed to form external hemorrhoids. Hemorrhoids may form in pregnancy due to impeded venous return (see http://www.nda.ox.ac.uk/wfsa/html/u09/u09_003.htm ) and in chronic constipation due to too little dietary fiber. Internal hemorrhoids are typically painless, as are carcinomas above the pectinate line. External hemorrhoids tend to be painful, as do cancers below the pectinate line.
At the pectinate line tributaries of the portal and inferior vena caval systems anastomose. In portal hypertension these portacaval anastomoses and superior rectal veins become dilated to form internal hemorrhoids (G11 2.61, 3.21B; G12 3.29; N291, 292, 379). It is important to remember, however, that internal hemorrhoids in the majority of patients are not due to portal hypertension (see http://www.emedicine.com/emerg/topic242.htm ). Internal hemorrhoids may prolapse through the anal canal and be compressed by contraction of the anal sphincters, impeding blood flow and resulting in strangulation and ulceration. A subcutaneous plexus of the inferior rectal veins around the anus may become thrombosed to form external hemorrhoids. Hemorrhoids may form in pregnancy due to impeded venous return (see http://www.nda.ox.ac.uk/wfsa/html/u09/u09_003.htm ) and in chronic constipation due to too little dietary fiber. Internal hemorrhoids are typically painless, as are carcinomas above the pectinate line. External hemorrhoids tend to be painful, as do cancers below the pectinate line.
1. On an articulated bony pelvis study an inferior view of the pelvic outlet. Position a clean pencil or pen connecting the two ischial tuberosities. This indicates the location of the boundary dividing the perineum into two triangles. The anterior urogenital triangle fills the interval between the right and left ischiopubic rami. The anal triangle lies posterior to the line connecting the ischial tuberosities. Now place the pencil so that it connects an ischial tuberosity with the junction of the sacrum and coccyx on that side. This indicates the approximate location of the thick sacrotuberous ligament, which is the posterolateral boundary of the anal triangle.
2. Hold the bony pelvis in the anatomical position so that the anterior superior iliac spines are in the same vertical plane as the anterior superior border of the pubic symphysis (Fig. 2). In this position the urogenital triangle occupies a nearly horizontal plane. Note that the anal triangle is obliquely oriented, facing posteriorly and slightly inferiorly. Now turn to the hemisected pelvis and perineum of the cadaver and attempt to verify these relationships.
3. Identify the anal canal on the hemisected pelvis and perineum. It is continuous with the rectum at the anorectal (perineal) flexure created by the pull of the puborectalis muscle (Figs. 4, 6A). The puborectalis portion may be difficult to distinguish, but try to identify the cut edge of the levator ani. If the bisection of the pelvis was off the midline, you may have to trim away additional tissue to open the rectum and anal canal.
4. In the anal canal look for longitudinal folds of mucous membrane. These are the anal columns. They are difficult to identify in some cadavers. If you can distinguish the anal columns, look for crescentic folds of mucosa connecting their inferior ends, the anal valves. The anal valves collectively form the pectinate line (Fig. 6B). Attempt to identify the internal anal sphincter, which is a thickening of the circular smooth muscle layer of the intestine around the upper 2/3 of the anal canal.
5. Place the cadaver in a prone position. Remove the skin remaining over the anal triangle to expose the ischioanal (ischiorectal) fossa (i.e., remove the skin as far forward as the posterior part of the scrotum or labium majus). The ischioanal fossa is filled by the ischioanal fat pad and nerves and blood vessels that supply the perineum. Before cleaning those structures attempt to identify the perineal body (central tendon of the perineum) (Figs. 3B, 5). It lies a short distance anterior to the anus, and you may see fibers of the external anal sphincter passing forward to attach there. The perineal body is usually palpable as a dense irregular mass of fibromuscular tissue, larger in females.
6. Clean the external anal sphincter. It is supplied by the inferior rectal (inferior anal) nerves and arteries (Fig. 5). These nerves branch from the pudendal nerve near its entrance into the pudendal canal and pass medially (or slightly anteromedially) toward the external anal sphincter. The accompanying inferior rectal arteries branch from the internal pudendal artery.
7.Use one of the following two approaches to find the branches of the pudendal nerve and internal pudendal artery: (1) Palpate the sacrotuberous ligament under the inferior border of the gluteus maximus muscle. If not done previously, carefully remove the lower part of the gluteus maximus, leaving the ligament intact. The sacrotuberous ligament is the inferior boundary of the lesser sciatic foramen, through which the pudendal nerve and internal pudendal vessels enter the perineum from the gluteal region. Bluntly dissect through the connective tissue in the upper part of the foramen to find the nerve and vessels. The inferior rectal nerve and vessels often branch within the gluteal region just proximal to the lesser sciatic foramen and may enter the ischioanal fossa separately from the pudendal nerve and internal pudendal vessels. Carefully remove the ischioanal fat pad piecemeal to clean the inferior rectal nerve and vessels. (2) Alternatively, use a scalpel to make a CORONAL incision from MEDIAL TO LATERAL through the ischioanal fat pad beginning at the anal canal. Insert a finger into the incision and attempt to palpate the inferior rectal vessels and nerves as they cross the ischioanal fossa from lateral to medial (or more accurately they usually course anteromedially). Clean the nerves and vessels that you find. While being careful to preserve the inferior rectal nerves and vessels, remove the ischioanal fat pad piecemeal.
8. Clean the lateral wall of the ischioanal fossa. It is formed by the ischium and the obturator internus muscle covered by obturator fascia. The pudendal canal is a split in the obturator fascia traversed by branches of the pudendal nerve and by the internal pudendal artery and vein en route to the urogenital triangle (Fig. 4). We will come back and look at these more closely later.
The urogenital triangle is the anterior half of the perineum, located between the right and left ischiopubic rami (Fig. 2). It is oriented in a nearly horizontal plane when the bony pelvis is in the anatomical position, although the external genitalia, particularly in the male, hide that orientation.
The fascia of the urogenital triangle (perineal fascia) consists of superficial and deep layers. The superficial perineal fascia, which is subcutaneous connective tissue, comprises fatty and membranous layers corresponding to, and continuous with, those of the anterior abdominal wall. The fatty layer of superficial perineal fascia is thin in the urogenital triangle of the male but substantial in the female, where it forms the substance of the labia majora and mons pubis (G11 3.53; G12 3.49, 3.59; N342, 348). In both sexes the fatty layer is continuous with the ischioanal fat pad in the anal triangle.
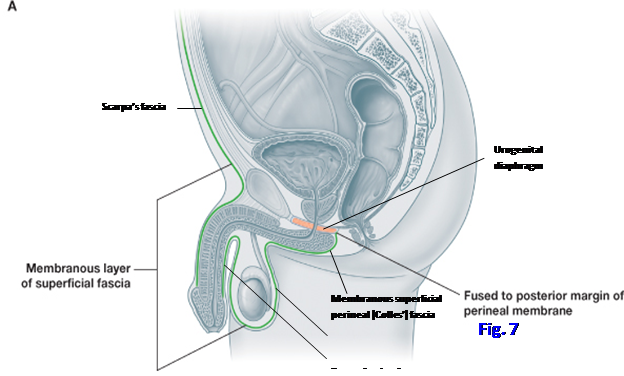
The membranous layer of superficial perineal fascia (Colles’ fascia) is attached posteriorly to the posterior margin of the perineal membrane and, therefore, doesn’t extend into the anal triangle (Fig. 7; G11 2.7B, 3.44; G12 2.7B, 3.51; N323, 346, 360). Laterally it is fused to the deep fascia of the thigh (fascia lata). Anteriorly the membranous layer is continuous with the membranous layer of superficial fascia in the anterior abdominal wall (Scarpa’s fascia). In the male, the scrotum and penis intervene in the midline, and the membranous layer is continuous with dartos fascia of the scrotum and the superficial penile fascia, which will be described later.
The deep fascia of the urogenital triangle (deep perineal fascia) is a thin layer investing the muscles that cover erectile bodies (N350, 352). Laterally the deep perineal fascia is attached to the ischiopubic rami. Anteriorly it blends with the deep fascia of the penis (Buck’s fascia) (Fig. 13C; G11 3.48A; G12 3.55A; N346) before attaching to the pubic bones and pubic symphysis.
There are two perineal pouches or compartments defined in relation to the perineal membrane. The superficial perineal pouch is a potential space superficial to the perineal membrane. It is located between the membranous layer of superficial perineal fascia (Colles’ fascia) and the perineal membrane (Fig. 7; N352, 357) and is bounded laterally by the ischiopubic rami. There are several corresponding structures in the superficial perineal pouch of males and females, but of course there also are some differences.
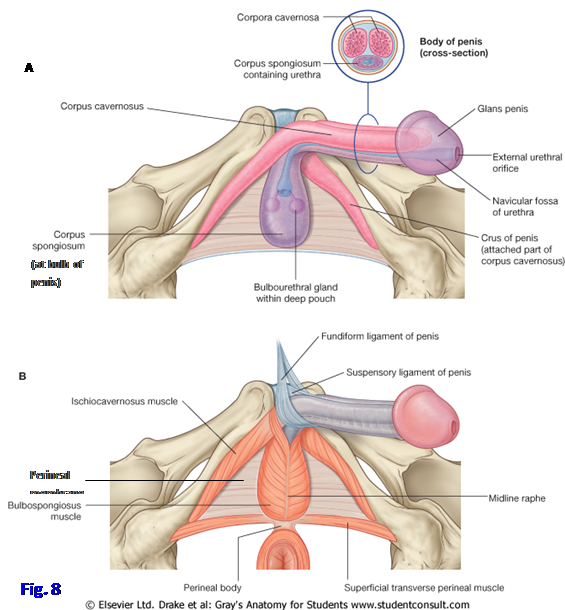
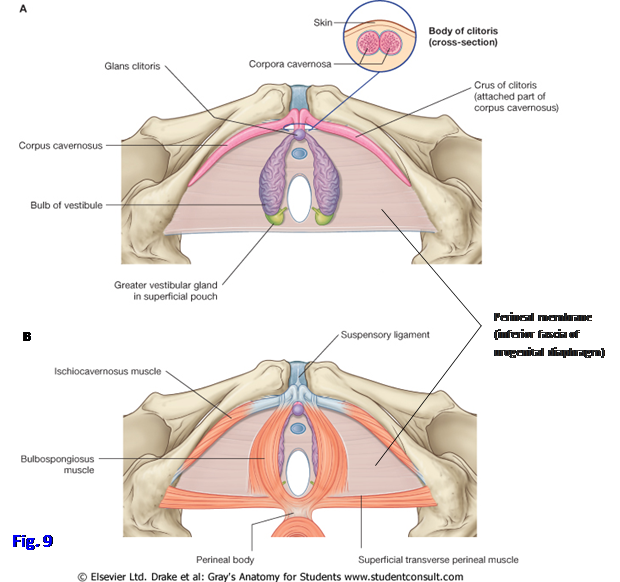
In males the superficial perineal pouch contains the bulb and crura of the penis (together the root of the penis) and their covering muscles (bulbospongiosus and ischiocavernosus, respectively), the proximal part of the spongy (penile) urethra, the superficial transverse perineal muscles, and deep perineal branches of the pudendal nerves and internal pudendal arteries and veins (Fig. 8; G11 3.42D-E, 3.44; G12 3.48D-E, 3.51; N361, 362). In females the superficial perineal pouch contains the crura of the clitoris and their covering ischiocavernosus muscles, the bulbs of the vestibule and their covering bulbospongiosus muscles, the superficial transverse perineal muscles, and the greater vestibular glands (Fig. 9; G11 3.42D-E, 3.52B, 3.54; Table 3.6 [p. 246]; G12 3.48D-E, 3.60A, 3.61, 3.62, Table 3.9 [p. 256]; N357, 358). These structures will be discussed below.
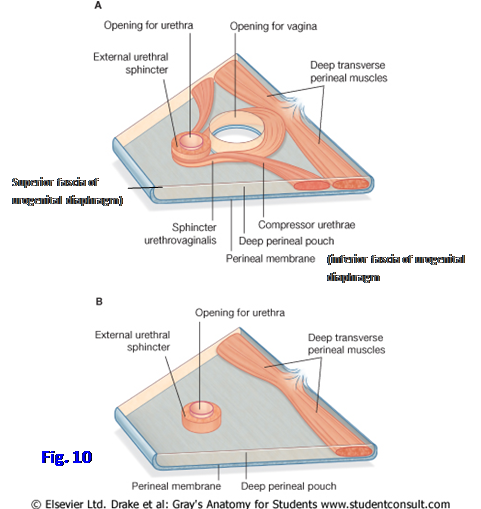
The deep perineal pouch traditionally has been described as equivalent to the urogenital diaphragm (Figs. 7, 10; G11 3.7A, 3.14B; G12 3.14A, 3.21A [unlabeled]; N350, 352, 358 and 359 [lower], 363), which consists of: 1) the tough perineal membrane (inferior fascia of the urogenital diaphragm); 2) skeletal muscles including the external urethral sphincter (sphincter urethrae); and 3) a thin superior fascia of the urogenital diaphragm. (Note: Some experts now dispute the existence of a discrete urogenital diaphragm and consider the deep perineal pouch to extend superiorly to the inferior fascia of the pelvic diaphragm, but the traditional description works well for our purposes and is still used in the clinical literature [e.g., http://www.mdconsult.com/das/article/body/228972862-2/jorg=journal&source=&sp=15875895&sid=0/N/514589/1.html?issn=00904295&_returnURL=http://linkinghub.elsevier.com/retrieve/pii/S0090429505007569%3Fshowall%3Dtrue ]. Also, the lateral portion of the urogenital diaphragm can be demonstrated in many cadavers and on coronal MRIs.)
The male urogenital triangle includes the external genitalia, perineal muscles, and urogenital diaphragm (Fig. 8). The male external genitalia include the scrotum, penis, and urethra. The scrotum is a skin-covered fibromuscular sac for the testes, spermatic cords, and associated structures. It consists of two pouches, one for each testis and spermatic cord, separated by a midline scrotal septum formed by an inward prolongation of dartos fascia. The location of the scrotal septum is indicated externally by a visible line, the scrotal raphe (G11 3.43A; G12 3.46A).
The skin of the scrotum is pigmented and wrinkled (rugose). Deep to the skin is a membranous layer of superficial fascia, the dartos fascia, devoid of fat but containing smooth muscle fibers. Contraction of the dartos muscle is responsible for the skin’s rugose appearance. The dartos fascia is continuous anteriorly with superficial penile fascia and Scarpa’s fascia of the anterior abdominal wall and posteriorly with the membranous layer of superficial perineal fascia (Colles’ fascia) (Fig. 7; N346, 360).
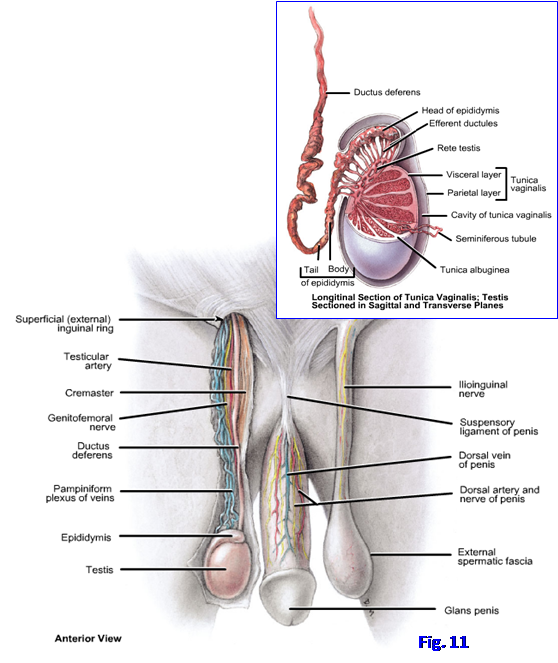
The testes are the male gonads, which produce germ cells (spermatozoa) and male hormones, mainly testosterone. The testes are suspended within the scrotum by the spermatic cords, with the left testis usually positioned lower than the right (Fig. 11; G11 2.13, 2.14, 3.19, 3.47A; G12 2.12, 2.15, 3.20, 3.54C; N367, 381, 389). The inferior pole of each testis is attached to the scrotum by a scrotal ligament, which is a remnant of the embryonic gubernaculum. Each testis has a tough fibrous outer layer, the tunica albuginea, with fibrous septa passing inward from it to divide the testis into lobules (Fig. 11, inset; G11 2.16; G12 2.15B, 2.16B; N367, 370). The lobules contain seminiferous tubules where spermatozoa are produced. Sperm are transported via the rete testis and efferent ductules to the head of the epididymis. The tunica albuginea is thickened posteriorly at the mediastinum testis where the ducts leave and blood vessels also enter or leave the testis.
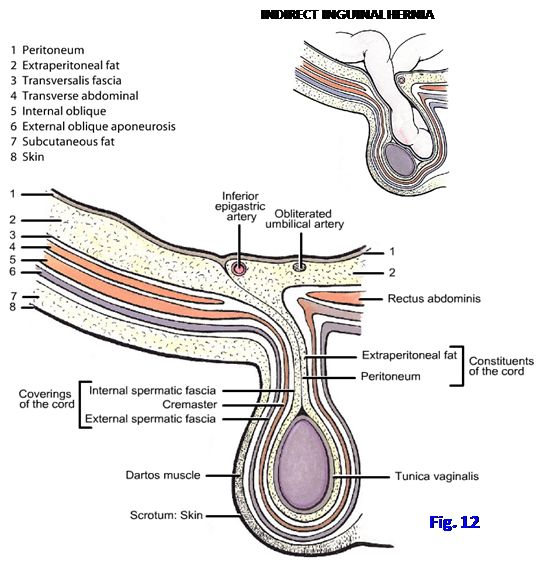
As it traversed the abdominal wall during its embryonic descent, the testis acquired fascial coverings from the layers there. From superficial to deep, these coverings are the external spermatic fascia derived from the external oblique aponeurosis, the cremasteric layer of muscle and fascia from the internal oblique muscle, and the internal spermatic fascia from the transversalis fascia (Fig. 12; G11 2.12B, 2.13, 2.15A; G12 2.12, 2.14; N243, 244, 367). Inside the spermatic fasciae the testis is covered anteriorly, medially, and laterally by a serous sac, the tunica vaginalis (G11 2.13, 2.16, 3.7A; G12 2.12B-E, 2.15B, 2.16B; N323, 367, 370). The tunica vaginalis is a remnant of the processus vaginalis, an evagination of the peritoneal cavity that accompanied the descent of the testis in the embryo. The tunica vaginalis has a visceral layer closely applied to the testis and epididymis and a parietal layer adjacent to the internal spermatic fascia. The potential cavity between the visceral and parietal layers of tunica vaginalis normally contains only a small amount of serous fluid.
The presence of excess serous fluid within the tunica vaginalis is a hydrocele, which typically results in painless enlargement of the scrotum. It may be a congenital condition due to persistence of the processus vaginalis or may be due to inflammation or other causes (e.g., see http://emedicine.medscape.com/article/777386-overview#showall ). The presence of blood within the tunica vaginalis may result from trauma and is known as a hematocele. A hydrocele may be distinguished from a hematocele by shining light on the scrotum in a darkened room (transillumination) because blood doesn’t transmit light.
The epididymis is a storage site for spermatozoa produced in the testis. It is an elongated structure applied to the top and posterolateral aspect of the testis (Fig. 11; G11 2.13, 2.14, 2.16, 3.14A; G12 2.12B-E, 2.15, 2.16, 3.20, 3.21B; N367, 370). The epididymis consists of a slender tube coiled so tightly that it appears to be solid. It has an enlarged upper end, the head of the epididymis, continuous with the efferent ductules. Below the head is the body of the epididymis. The lower end, the tail of the epididymis, is continuous with the ductus deferens.
The spermatic cord consists of structures running to and from the testis and its coverings (Figs. 11, 12; G11 2.14, 2.15A, 2.17, 3.19; G12 2.15, 2.16A-B, 3.20, 3.21B; N243-245, 367, 381, 389). The spermatic cord begins at the deep inguinal ring, traverses the inguinal canal, and emerges through the superficial inguinal ring to descend into the scrotum. As it traversed the abdominal wall during descent of the embryonic testis, the spermatic cord acquired fascial coverings, the internal spermatic fascia from the transversalis fascia, the cremasteric layer of muscle and fascia from the internal oblique muscle, and the external spermatic fascia derived from the external oblique aponeurosis. The transversus abdominis does not contribute a covering layer to the spermatic cord. The cremasteric muscle reflexly contracts in response to cold to raise the testis in the scrotum. Stroking the upper medial thigh of the male patient with a tongue depressor elicits a cremasteric reflex that tests the integrity of the L1 spinal cord segment, the ilioinguinal nerve (afferent limb of reflex arc), and the genital branch of the
genitofemoral nerve (efferent limb of reflex arc).
An indirect inguinal hernia, since it follows the path of descent of the testis, is enclosed within the three layers covering the spermatic cord (Fig. 11, inset; G11 2.15B; G12 2.14) (e.g., see http://www.emedicine.com/PED/topic2559.htm ). An indirect inguinal hernia is due to a persisting processus vaginalis and leaves the abdominal cavity through the deep inguinal ring lateral to the inferior epigastric artery. These are the most frequent type of inguinal hernias. A direct inguinal hernia pushes directly through the abdominal wall (inguinal triangle) medial to the inferior epigastric artery and is not enclosed within the three coverings of the spermatic cord (G11 2.15C; G12 2.14). It is typically due to a weak or narrow conjoint tendon. A direct inguinal hernia is covered by transversalis fascia and acquires a covering of external spermatic fascia if it pushes through the superficial inguinal ring.
The components of the spermatic cord are the ductus deferens and artery of the ductus deferens, testicular artery, cremasteric artery, pampiniform plexus of veins, genital branch of the genitofemoral nerve, sympathetic nerve fibers, and lymphatic vessels (Fig. 11; G11 2.13, 2.14, 2.17, 3.19; G12 2.12B-D, 2.15A, 2.16A-B, 3.20, 3.21B; N381, 388, 389). The ductus (vas) deferens is a thin muscular tube continuous with the tail of the epididymis. During ejaculation, contractions of its smooth muscle transport sperm from their storage site within the epididymis to the ejaculatory duct in the prostate. The small artery of the ductus deferens usually branches from the inferior vesical artery (G12 3.27A; N381).
The testicular artery is a branch of the abdominal aorta to the testis. It arises just below the origin of the renal artery. The lymphatic vessels of the spermatic cord follow the testicular artery back to the lateral aortic (lumbar) nodes (G11 2.17B; G12 2.16C; N381, 388). Therefore, testicular cancer metastasizes to the lateral aortic nodes. Scrotal cancer, on the other hand, metastasizes to the superficial inguinal lymph nodes, where most of the superficial perineum drains. Twisting of the spermatic cord (testicular torsion) deprives the testis of its blood supply and results in testicular necrosis. Testicular torsion is a surgical emergency (e.g., see http://emedicine.medscape.com/article/438817-overview#showall ).
The cremasteric artery is a branch of the inferior epigastric artery and supplies the cremasteric muscle. The genital branch of the genitofemoral nerve innervates the cremaster muscle and is the efferent limb of the cremasteric reflex arc.
The pampiniform plexus of veins ascends around the testicular artery before converging near the deep inguinal ring to form the testicular vein (Fig. 11; G11 2.13B, 2.14, 3.19A; G12 2.12D, 2.15A, 3.20; N381). The right testicular vein drains into the inferior vena cava, but the left testicular vein is a tributary of the left renal vein (G11 2.63A; G12 2.63A; N381). A varicocele is a dilated, tortuous pampiniform plexus of veins. Varicoceles occur predominantly on the left side, perhaps because of the higher venous pressure in the left renal vein than in the inferior vena cava, but they may occur on the right side. They result from defective venous valves or more serious problems, such as cancer that has metastasized along the renal vein. A palpated varicocele is described as feeling like a “bag of worms.”
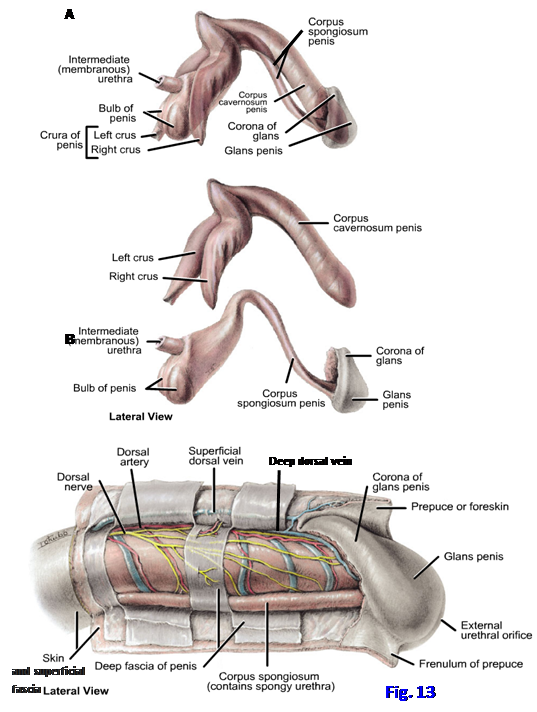
The penis is both the male sexual organ and contains the terminal portion of the urethra. In the anatomical position the penis is considered to be erect; therefore, when it is flaccid the “dorsum” is directed anteriorly. The penis is formed by three cylindrical bodies of erectile tissue, the paired corpora cavernosa dorsally and the single corpus spongiosum ventrally (Figs. 5, 8, 13; G11 3.19, 3.48, 3.49, 3.51A, 3.61B-D; G12 3.20, 3.21A, 3.55-3.58, 3.68B-C, 3.69; N346, 361, 362, 365). The corpus spongiosum contains the spongy (penile) urethra. Each erectile body has an outer fibrous covering, the tunica albuginea. The three erectile bodies are bound together by the tough deep fascia of the penis (Buck’s fascia), which is continuous with the deep perineal fascia (N346, 361). Outside the deep fascia is the superficial fascia of the penis (superficial penile fascia), which is continuous posteriorly with dartos and Colles’ fascia and superiorly with Scarpa’s fascia (Fig. 7).
The penis is subdivided into a root, body, and glans (Fig. 8; G11 3.43B, 3.47A-B, 3.49A, 3.51D; G12 3.46B, 3.54A, 3.56A, 3.58A; N331, 368). The root of the penis is the attached part and is located within the superficial perineal pouch. The root consists of the crura, the bulb, and their covering muscles. Each crus of the penis is the proximal portion of a corpus cavernosum and is attached to the ischiopubic ramus of that side and to the perineal membrane (N362). The crus is covered inferiorly by the ischiocavernosus muscle (Figs. 5, 8B; G11 3.42D-E, 3.44; Table 3.6 [p. 246]; G12 3.48D-E, 3.51, Table 3.9 [p. 256]; N361, 363 [Frontal section], 375). The bulb of the penis is the enlarged posterior portion of the corpus spongiosum. It is anchored to the perineal membrane (Fig. 8; G11 3.45, 3.51B; G12 3.52, 3.56, 3.57A-B; N362, 363 [Frontal section], 365) and is covered inferiorly by the two bulbospongiosus muscles fusing in a midline raphe (N361). The bulb is penetrated by the urethra, which continues anteriorly in the corpus spongiosum.
The body of the penis is the free part suspended from the pubic symphysis (Figs. 8A, 11, 13; G11 3.7A, 3.19; G12 3.14A, 3.20, 3.28A; N331, 346, 368). It is formed by the fused corpora cavernosa dorsally and the unpaired corpus spongiosum ventrally. The corpus spongiosum contains the spongy (penile) urethra. These erectile bodies are enclosed within the deep and superficial fasciae of the penis and skin (Figs. 7, 13C; G11 3.48A; G12 3.55A; N245, 360, 361, 362).
The glans of the penis is the distal expanded portion of the corpus spongiosum (Figs. 8A, 11, 13; G11 3.19, 3.47A-B, 3.48A-B, 3.49; G12 3.20, 3.54, 3.55A, 3.56, 3.58C; N362, 365). It is conical in shape and has a posterior margin that projects as the corona of the glans to cover the blunted anterior ends of the corpora cavernosa. The glans contains the slit-like opening of the spongy urethra, the external urethral orifice (Figs. 8A, 13C). The skin of the penis is prolonged as a double layer covering the glans, the prepuce (foreskin) (G11 3.6A; G12 3.54B, 3.55A; N346), in males in whom it hasn’t been surgically removed (circumcision). A median fold of skin, the frenulum of the prepuce, attaches the prepuce to the inferior surface of the glans (Fig. 13C; G11 3.48A; G12 3.55A; N362).
Two condensations of fascia suspend the penis at the junction of the root and the body. The suspensory ligament of the penis is a condensation of deep fascia that extends from the pubic symphysis to the deep fascia of the penis, attaching to both (Figs. 8B, 11; G11 2.14, 3.19, 3.47A; G12 2.15A, 3.20 [unlabeled], 3.54C; N244, 346). The fundiform ligament of the penis is a condensation of superficial fascia descending in the midline from the linea alba to split around the penis and blend with dartos fascia of the scrotum (G11 2.8A; G12 2.8A; N243, 346). The fundiform ligament, therefore, is superficial to the suspensory ligament of the penis.
The distal portion of the male urethra is the spongy, or penile, urethra (Figs. 8A, 13A-B; G11 3.7A, 3.14B, 3.19, 3.49; G12 3.14A, 3.20, 3.21A-B, 3.56, 3.57; N346, 365). It is the continuation of the membranous urethra, which traverses the urogenital diaphragm (Fig. 7; G11 3.7A, 3.14B, 3.19; G12 3.14A, 3.20, 3.21A; N364, 365) and is surrounded by the voluntary external urethral sphincter (sphincter urethrae). The spongy urethra enters the bulb of the penis and continues through the length of the corpus spongiosum to the external urethral orifice. Just proximal to the external urethral orifice the spongy urethra has a small expansion within the glans of the penis, the navicular fossa (Fig. 8A; G11 3.6A, 3.48B-C, 3.51D; G12 3.57D, 3.58A & C; N346, 365).
The innervation, blood supply, and lymphatic drainage of the external genitalia will be described with the rest of the perineal region.
The superficial perineal muscles are located within the superficial perineal pouch (Figs. 5, 8; G11 3.42E, 3.44, Table 3.6 [p. 246]; G12 3.48E, 3.51, Table 3.9 [p. 256]; N346, 361, 362, 375). They include the superficial transverse perineal muscles, the bulbospongiosus muscles, and the ischiocavernosus muscles. The two superficial transverse perineal muscles pass from the ischial tuberosities medially along the posterior border of the perineal membrane to attach into the perineal body (central tendon of the perineum). Through their traction on the central tendon these muscles help to stabilize the urogenital diaphragm and floor of the pelvis.
The two bulbospongiosus muscles pass from the perineal membrane and superior surface of the corpora spongiosum and cavernosa to meet in a midline raphe on the inferior surface of the bulb and corpus spongiosum (Figs. 5, 8; G11 3.42E, 3.44, Table 3.6 [p. 246]; G12 3.48E, 3.51, Table 3.9 [p. 256]; N361, 375). Posteriorly fibers attach to the perineal body. Contractions of the bulbospongiosus muscles assist in producing erections and in helping to empty the spongy urethra during ejaculation and micturition.
The ischiocavernosus muscles cover the crura of the penis (Figs. 5, 8; G11 3.42E, 3.44, Table 3.6 [p. 246]; G12 3.48E, 3.51, Table 3.9 [p. 256]; N361, 363 [Frontal section], 375). Each muscle takes origin from the ischiopubic ramus and ischial tuberosity and inserts into the perineal membrane and the inferior and medial aspect of the crus of the penis. Contractions of the ischiocavernosus muscles help produce erections.
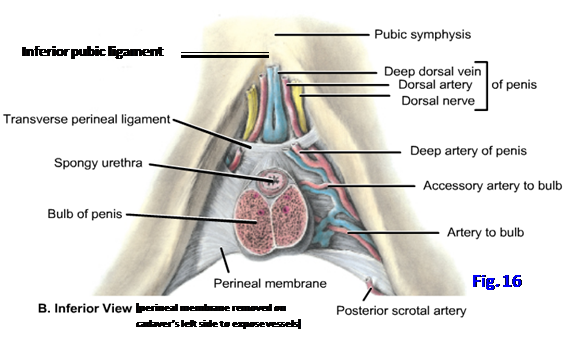
The urogenital diaphragm fills the midline urogenital hiatus of the pelvic diaphragm from below, except where structures traverse it (Fig. 3A). The urogenital diaphragm consists of an inferior fascia, muscular layer, and a superior fascia (Figs. 3A, 7, 8B, 10B; G11 3.7A, 3.14B; G12 3.14A, 3.21A; N350, 363). The inferior fascia of the urogenital diaphragm is the tough, fibrous perineal membrane, which attaches laterally to the ischiopubic rami and in the posterior midline to the central tendon. The perineal membrane provides passive support for the pelvic viscera and attachment for the erectile bodies and associated muscles. The superior fascia of the urogenital diaphragm is poorly defined. It fuses with the inferior fascia at the anterior and posterior borders of the urogenital diaphragm. At the anterior border their fusion forms a thickened band of connective tissue, the transverse perineal ligament (N346, 363). It lies behind the pubic symphysis and inferior pubic (arcuate) ligament, from which it is separated by a gap (Fig. 3B). The gap is traversed by the deep dorsal vein of the penis in the male.
The urogenital diaphragm contains a layer of skeletal muscle and connective tissue between the superior and inferior fasciae of the urogenital diaphragm (Fig. 10B; G11 3.7A, 3.42B; G12 3.14A, 3.48B; N363). The urogenital diaphragm corresponds to the traditional description of the deep perineal space. Bulbourethral (Cowper’s) glands are embedded within the urogenital diaphragm of the male, from which they secrete clear mucus into the proximal part of the spongy urethra during sexual excitement (G11 3.14A, 3.19A, 3.51D; G12 3.20, 3.21B, 3.22, 3.58A; N346, 363, 365). Branches of the pudendal nerves and internal pudendal blood vessels also penetrate the urogenital diaphragm and will be discussed below.
The muscles in the urogenital diaphragm of the male are the external urethral sphincter and the deep transverse perineal muscles (Fig. 10B; G11 3.7A, 3.19A, Table 3.6 [p. 247, upper left]; G12 3.14A, 3.20, Table 3.9 [p. 256]; N346, 363). (Note: Ignore drawings of a compressor urethrae muscle in males.) The external urethral sphincter (sphincter urethrae) is a collection of circular skeletal muscle fibers surrounding the membranous urethra. It provides voluntary control of micturition. The deep transverse perineal muscles take origin from the ischial tuberosities and pass medially along the posterior border of the urogenital diaphragm to insert into the perineal body. Therefore, the deep transverse perineal muscles join the superficial transverse perineal muscles, bulbospongiosus, external anal sphincter, levator ani, and the perineal membrane in attaching into the perineal body, helping to provide support for pelvic viscera such as the bladder.
The major nerve and blood supply to the male perineum reaches it via the pudendal canal. The pudendal (Alcock’s) canal is a passageway formed by a split in the obturator internus fascia in the lateral wall of the ischioanal fossa (Figs. 4, 5, 14; G11 3.10A, 3.13C, 3.25B, 3.44; G12 3.16, 3.22C, 3.31, 3.51; N372, 378, 385, 391, 491 [“Dorsal nerve of penis’ and “Perineal nerve” near “Sacrotuberous ligament” are traversing pudendal canal]). The pudendal nerve and the internal pudendal artery and vein enter the pudendal canal from the gluteal region via the lesser sciatic foramen.
The pudendal nerve is formed within the pelvis by the anterior rami of spinal nerves S2-4 (Fig. 14; G11 3.24- 3.26, Table 3.4 [p. 223, upper right]; G12 3.12, 3.31; N390, 391, 485, 487). It exits the pelvis via the greater sciatic foramen, curves around the ischial spine or lateral part of the sacrospinous ligament, and enters the perineum via the lesser sciatic foramen. From the lesser sciatic foramen the nerve enters the pudendal canal. As it enters the canal, the pudendal nerve gives off the inferior rectal (inferior anal) nerves, which supply the external anal sphincter and perianal skin (G11 3.25B, 3.44; G12 3.31, 3.51; N390, 391, 491).
Near the proximal end of the pudendal canal, the pudendal nerve divides into its two terminal branches, the perineal nerve and the dorsal nerve of the penis (Fig. 14; G11 3.25B, Table 3.2 [p. 192, lower]; G12 3.8A, 3.31; N390, 491). Within the pudendal canal the perineal nerve lies inferior (superficial) to the internal pudendal artery. The perineal nerve branches into the superficial perineal nerves and the deep perineal nerve (N391). The superficial perineal nerves become the posterior scrotal nerves, which provide cutaneous innervation to the posterior aspect of the scrotum (Figs. 5, 14; G11 3.44, 3.47C; G12 3.51, 3.55B; N390, 391, 491). The deep perineal nerve supplies the muscles of the superficial (e.g., bulbospongiosus) and deep (e.g., external urethral sphincter) perineal pouches.
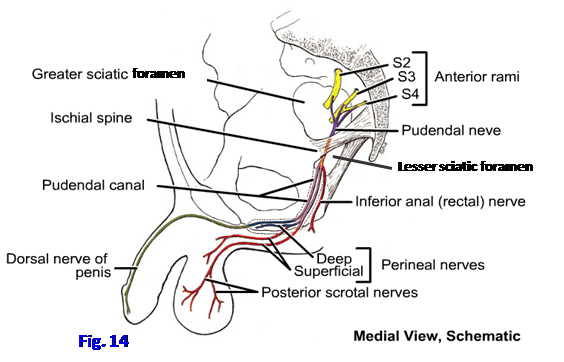
The dorsal nerve of the penis is the primary sensory nerve of the penis, especially the sensitive glans (Fig. 14; G11 2.14, 3.47A & C, 3.48A; G12 2.15A, 3.54C, 3.55A-B; N389, 390). It arises within the proximal end of the pudendal canal and passes forward superior (deep) to the internal pudendal artery. From the pudendal canal the dorsal nerve of the penis enters the urogenital diaphragm (deep perineal pouch). It pierces the perineal membrane and passes onto the dorsum of the penis, where it runs mostly lateral to the dorsal artery of the penis (Fig. 11; G11 3.48A; G12 3.55A; N361 [Transverse section], 389).
The male perineum receives additional sensory innervation. The anterior aspect of the scrotum receives cutaneous innervation from the anterior scrotal nerves, which arise from the ilioinguinal nerve and genital branch of the genitofemoral nerve (Fig. 11; G11 3.47A; G12 3.54C; N251, 389). Laterally there are small sensory contributions from the perineal branches of the posterior femoral cutaneous nerves (Fig. 5; G11 3.44; G12 3.51; N391, 491).
Postganglionic sympathetic nerve fibers are carried to the perineum mainly by the pudendal nerve and its branches (G11 3.23A). These sympathetic fibers innervate the dartos muscle of the scrotum and sweat glands. During ejaculation the sympathetic nerves in the spermatic cord cause peristaltic contractions of smooth muscle of the ductus deferens to move sperm toward the ejaculatory duct. Parasympathetic nerve fibers from the prostatic plexuses descend through the pelvic floor as the cavernous nerves to reach arteries and arteriovenous anastomoses of the erectile bodies (G12 3.31B; N390). The preganglionic parasympathetic fibers arise in the pelvic splanchnic nerves (nervi erigentes) from spinal nerves S2-4 and join the inferior hypogastric plexuses, of which the prostatic plexuses are subdivisions (G11 3.50B; G12 3.31B; N390). The parasympathetic fibers are responsible for erection.
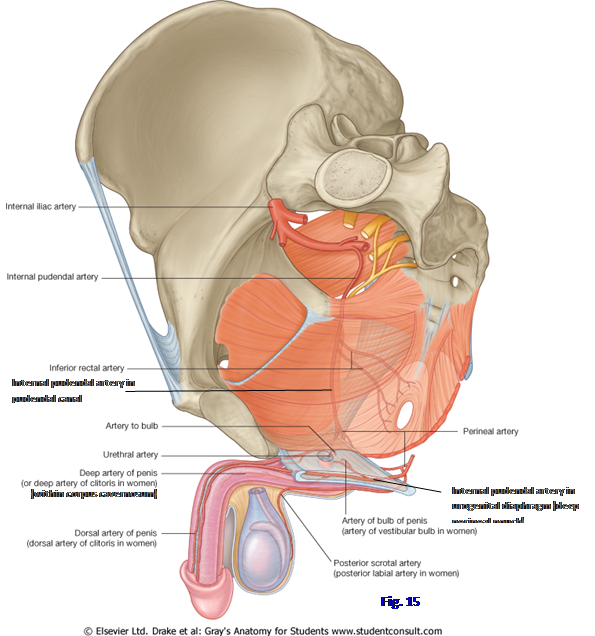
The blood supply to the perineum is mainly from the internal pudendal artery (Fig. 15; G11 Table 3.3 [pp. 212-213]; G12 3.27A, Table 3.4 [p. 225]; N383). It arises from the anterior trunk of the internal iliac artery and leaves the pelvis through the greater sciatic foramen. The internal pudendal artery follows the pudendal nerve’s short passage through the gluteal region (G11 5.25; G12 5.27A), around the ischial spine, and into the lesser sciatic foramen to reach the perineum. As the internal pudendal enters the pudendal canal, it gives off inferior rectal (inferior anal) arteries to the external anal sphincter and perianal skin (Fig. 5; G11 3.10B-C, 3.44; G12 3.17A, 3.51; N378, 385). Within the pudendal canal, the internal pudendal artery is sandwiched between the perineal nerve superficial to it and the dorsal nerve of the penis deep to it (G11 Table 3.2 [p. 192, lower]; G12 3.8). The perineal artery branches from the internal pudendal near the anterior end of the pudendal canal (N383, 385). The perineal artery sends posterior scrotal branches to accompany the nerves of the same name to the posterior aspect of the scrotum and the structures of the superficial perineal pouch.
At the anterior end of the pudendal canal, the internal pudendal artery enters the urogenital diaphragm with the dorsal nerve of the penis (N363, 391). Within the urogenital diaphragm, the internal pudendal gives off an artery to the bulb of the penis and continues forward (Figs. 15, 16; G11 3.51B; G12 3.57A; N363, 385). The artery to the bulb supplies the bulbourethral gland and then pierces the perineal membrane to reach the bulb of the penis. The terminal branches of the internal pudendal artery are the deep and dorsal arteries of the penis. The deep artery of the penis pierces the perineal membane to enter the deep surface of the crus of the penis. It travels forward in the center of the corpus cavernosum (G11 3.51A; G12 3.57B-C; N361 [Transverse section], 385). The dorsal artery of the penis pierces the perineal membrane in company with the dorsal nerve of the penis and runs along the dorsum of the penis, usually medial to the nerve (Figs. 11, 13C; G11 3.47A, 3.48A; G12 3.54C, 3.55A, 3.57C; N385).
The tributaries of the internal pudendal vein largely correspond to the branches of the artery, except for the dorsal veins of the penis. The superficial dorsal vein of the penis (Fig. 13C; G11 2.4, 3.48A; G12 2.5A, 3.55A; N250) branches and sends venous blood from the skin and superficial fascia bilaterally into the superficial external pudendal veins. The deep dorsal vein of the penis pierces the suspensory ligament of the penis and traverses the gap between the transverse perineal ligament and inferior pubic ligament (G11 3.51B; G12 3.27B, 3.57A; N363, 383) to enter the pelvis and reach the prostatic venous plexus.
DISSECTION OF THE MALE UROGENITAL TRIANGLE
9. The penis should have been sagittally sectioned when the pelvis was bisected. If the cut was off center, look first at the side with the larger portion of the organ. Identify the fundiform ligament of the penis, a condensation of superficial fascia descending in the midline from the linea alba to split around the penis. Deep to the fundiform ligament find the suspensory ligament of the penis. It is a fibrous condensation of deep fascia running downward from the pubic symphysis to the deep fascia of the penis.
10. Study the cut edge of the body of the penis and identify the corpus cavernosum dorsally and the corpus spongiosum ventrally (G11 3.19A; G12 3.20; N346). Study the thick outer fibrous covering of each erectile body, the tunica albuginea. If the section was exactly in the midline it exposed the septum penis formed by fusion of the tunica albuginea of the two corpora cavernosa in the body of the penis (G11 3.48D; G12 3.57C & E; N361). Note that the tunica albuginea sends fibrous trabeculae inward between the vascular sinuses (cavernae) of the corpus. The vascular sinuses fill with blood to produce an erection when the arteries of the penis are dilated under parasympathetic control by the cavernous nerves and venous outflow is impeded by contraction of the bulbospongiosus and ischiocavernosus muscles.
11. The narrow spongy urethra runs distally through the corpus spongiosum to open at the external urethral orifice on the glans of the penis. Verify that the glans is the expanded terminal portion of the corpus spongiosum. If the sagittal section of the penis missed the midline urethra, use small scissors to trim away tissue to open the spongy urethra and trace its course. Find where the membranous urethra pierces the urogenital diaphragm to enter the bulb of the penis (G11 3.7A, 3.14B, 3.19A; G12 3.14A, 3.20, 3.21A; N364, 365). Note a small expansion of the distal urethra, the navicular fossa, near the external urethral orifice.
12. Carefully remove the thin skin of the bisected penis to expose the vessels and nerves on the dorsum. Within the superficial fascia along the midline clean the superficial dorsal vein of the penis (Fig. 13C; N250). Retract the superficial dorsal vein and bluntly dissect through the deep fascia of the penis (Buck’s fascia) to expose the midline deep dorsal vein of the penis (N245, 361 [Transverse section]). Attempt to verify that the deep vein proximally traverses the gap between the transverse perineal ligament and the inferior pubic ligament en route to the prostatic venous plexus within the pelvis (Fig. 16; N383). Lateral to the deep dorsal vein find the dorsal artery of the penis and the dorsal nerve of the penis (Figs. 11, 13C). Be aware that the positions of the artery and nerve may be transposed.
13. Attempt to demonstrate an artery coursing down the center of the corpus cavernosum (G11 3.51A; G12 3.57B-C; N361, 385). This is the deep artery of the penis. The deep artery and the dorsal artery of the penis are the terminal branches of the internal pudendal artery within the substance of the urogenital diaphragm (Fig. 16).
14. Turn your attention to the bisected scrotum. Attempt to identify the posterior scrotal nerves and posterior scrotal vessels approaching the scrotum from the anterior portion of the pudendal canal (Figs. 5, 14). These arise as superficial perineal branches of the pudendal nerve and the internal pudendal artery and vein, respectively. Remove the thin skin of the scrotum to expose the dartos fascia. It may have a reddish tinge, depending on embalming, due to the presence of smooth muscle fibers. Look for the midline scrotal septum, which separates the two testes. It is formed by an inward extension of the dartos fascia (N367). Remove the dartos layer to expose the spermatic fasciae over the testis and spermatic cord. The spermatic fasciae are usually difficult to distinguish in a dissection, but try to visualize the arrangement of the external spermatic fascia, cremasteric layer of muscle and fascia, and the internal spermatic fascia (Fig. 12). Carefully remove the spermatic fasciae to expose the testis and spermatic cord.
15. The testis invaginates a serous sac, the tunica vaginalis, from behind (Fig. 11, inset). The internal spermatic fascia is difficult to separate from the parietal layer of the tunica vaginalis. Make a longitudinal incision through the anterior part of the parietal layer. The potential cavity of the tunica vaginalis in an elderly male may be obliterated or may contain an abnormal amount of fluid. Identify the visceral layer of the tunica vaginalis. It adheres to the anterior surface and sides of the testis and the epididymis. Now use a scalpel to make a transverse incision through the middle of the testis. Identify the tunica albuginea and fibrous septa extending inward from it to divide the testis into lobules containing seminiferous tubules. The posterior thickening of the tunica albuginea, where vessels and ducts enter or leave the testis, is the mediastinum testis.
16. Note that the inferior pole of the oval testis is anchored to the scrotum by the fibrous scrotal ligament. The scrotal ligament is a remnant of the embryonic gubernaculum that was involved in the descent of the testis.
17. Find the head of the epididymis above the superior pole of the testis (Fig. 11, inset). The head continues into the body of the epididymis posterolateral to the testis and the slender tail of the epididymis at the inferior pole of the testis. The tail of the epididymis is continuous with the ductus deferens.
18. Tease apart the components of the spermatic cord (Fig. 11). The ductus deferens is a slender muscular tube that begins at the tail of the epididymis. It has a posterior location within the spermatic cord and can be recognized by palpation due to its hard, cord-like feel. The small artery of the ductus deferens runs on the duct’s surface but is usually too small to see. The testicular artery is usually recognizable surrounded by the pampiniform plexus of veins. The pampiniform plexus may be dilated and tortuous to form a varicocele, more commonly on the left side. The other components of the spermatic cord are typically too small to identify grossly.
19. Reflect the testis and spermatic cord superiorly. Bluntly dissect through, and carefully remove, the superficial fascia over the urogenital triangle to expose the muscles of the superficial perineal pouch. The muscles are covered by a thin layer of deep perineal fascia, which is continuous with the deep fascia of the penis. The superficial transverse perineal muscles run parallel to the posterior border of the urogenital diaphragm. They are variable in size and degree of development, but attempt to find this muscle on the hemipelvis you are studying.
20. Identify the cut edge of the bulb of the penis. The bulbospongiosus is a thin layer of skeletal muscle covering the superficial surface of the bulb and proximal corpus spongiosum. Clean the bulbospongiosus. There are two ways to find the ischiocavernosus muscle. One way is to palpate the ischial tuberosity and follow the ischiopubic ramus anteriorly and superiorly from it. The ischiocavernosus covers the crus of the penis, which is attached to the ischiopubic ramus. The other way to find the ischiocavernosus is to follow the base of the corpus cavernosum to its origin in the crus (Fig. 8). Reflect the thin ischiocavernosus muscle to expose the crus.
21. Between the bulbospongiosus and ischiocavernosus muscles find a tough, often glistening, fibrous sheet. This is the perineal membrane, which is the inferior fascia of the urogenital diaphragm (Figs. 5, 8B, 16). Push against the perineal membrane to feel its toughness. The perineal membrane provides passive support for the anterior pelvic organs, as well as attachment for the erectile bodies and their covering muscles. Attempt to lift the bulb of the penis away from the perineal membrane and observe that it is firmly attached.
22. On one half of the perineum open the urogenital diaphragm (deep perineal pouch) from below by careful removal of the perineal membrane. Distinguishing the external urethral sphincter and deep transverse perineal muscles is difficult, but be aware of their basic arrangement (Fig. 10B). Bulbourethral glands are embedded within the urogenital diaphragm of the male, but they are small and difficult to demonstrate.
23. Now go to the lateral wall of the ischioanal fossa and locate the pudendal canal (Fig. 5; G11 3.10A, 3.44; G12 3.16, 3.51). This can be done either by tracing the posterior scrotal nerves and vessels to their origin from the perineal nerve and internal pudendal vessels, respectively, or by palpating these neurovascular structures through the obturator internus fascia (Figs. 4, 5). Using blunt dissection open the pudendal canal. Verify that from superficial to deep (i.e., inferior to superior) the contents of the pudendal canal are the perineal nerve, internal pudendal vessels, and dorsal nerve of the penis.
24. Follow the internal pudendal artery from the pudendal canal into the substance of the urogenital diaphragm. The internal pudendal artery gives off the artery to the bulb before its terminal division into the deep artery of the penis and the dorsal artery of the penis (Fig. 16). Find the artery to the bulb piercing the perineal membrane to enter the bulb of the penis. Clean the deep artery of the penis. It pierces the perineal membrane to enter the crus. The dorsal artery of the penis, which joins the dorsal nerve of the penis to travel along the dorsum, was seen earlier. XXX
The female urogenital triangle includes the female external genitalia, perineal muscles, and urogenital diaphragm (Figs. 9, 17; G11 3.52A; G12 3.47B; N 356-358). The female external genitalia comprise the mons pubis and labia majora enclosing the pudendal cleft, the labia minora enclosing the vestibule, and the clitoris. The interchangeable terms “vulva” and “pudendum” include all of these parts. The external genitalia of the female and the male are homologous, and the muscles, nerves, and vessels of the female perineum are almost identical with those of the male.
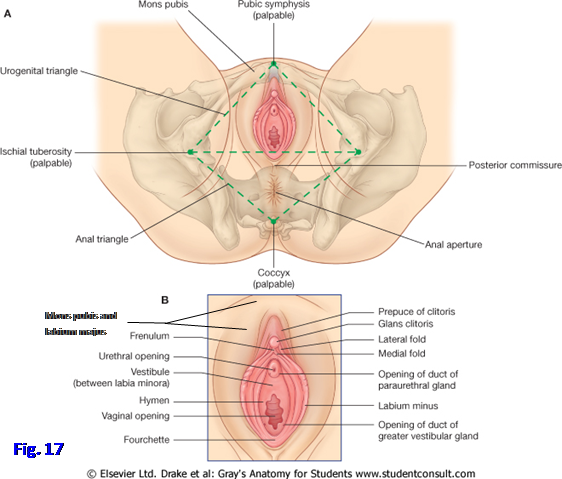
The mons pubis is a rounded eminence anterior to the pubic symphysis and the bodies of the pubic bones (Fig. 17). The eminence is formed by a mass of subcutaneous fat where the two
labia majora come together. The amount of fat typically decreases after menopause. After puberty the mons pubis is covered with pubic hair.
The labia majora are prominent folds of skin and subcutaneous fat on either side of the pudendal cleft (Fig. 17; G11 3.52A, 3.53; G12 3.47B, 3.59; N356). They join posteriorly in the posterior labial commissure, originally a ridge, but which typically becomes a depression after the first vaginal childbirth. The posterior labial commissure overlies the perineal body. The round ligament of the uterus, which is a remnant of the gubernaculum in the female, ends in the subcutaneous tissue of the labium majus after traversing the inguinal canal (G11 2.11A&C, 3.53; G12 2.11A & C, 3.59; N357). The skin over the lateral aspect of each labium majus is pigmented and features pubic hair. The skin over the medial aspect is smooth and hairless.
The labia minora are thin folds of hairless skin enclosing the vestibule (vestibule of the vagina), into which both the urethra and the vagina open (Fig. 17; G11 3.52A, 3.56; G12 3.47B, 3.61; N356, 359). Anteriorly each labium minus divides into two folds that diverge around the glans of the clitoris. The medial folds of the two labia unite posterior to the glans of the clitoris to form the frenulum of the clitoris. The lateral folds unite anterior to the glans to form the prepuce of the clitoris. Posteriorly the labia minora of sexually inactive young women are connected by a small transverse fold, the fourchette (frenulum of the labia minora).
The clitoris is an erectile organ. It is strictly an organ of sexual arousal and is unrelated to the urethra. The clitoris consists of a root, body, and glans (Figs. 9A, 18; G11 3.54; G12 3.62; N342, 358). The root of the clitoris is the attached part and is located in the superficial perineal pouch. The root consists of the two crura of the clitoris. Each crus is the proximal portion of a corpus cavernosum and is attached to the ischiopubic ramus and perineal membrane. The crus is covered inferiorly by the ischiocavernosus muscle (Fig. 9B; G11 3.42D-E, Table 3.6 [p. 246]; G12 3.48D-E, Table 3.9 [p. 256]; N358, 359).
The body of the clitoris is the part suspended from the pubic symphysis by a condensation of deep fascia, the suspensory ligament of the clitoris (G11 3.56; G12 3.61; N357, 358). The body of the clitoris is formed by the fusion of the two corpora cavernosa. It is largely covered by the prepuce of the clitoris.
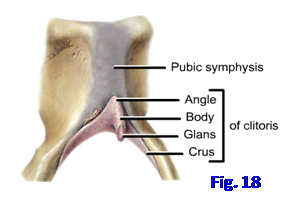
The glans of the clitoris is the distal portion (Figs. 9A, 18; G11 3.52A, 3.54; G12 3.47B, 3.62; N356). Together the body and glans of the clitoris are approximately 2 cm in length but < 1 cm in diameter. The glans is densely supplied with sensory nerve endings by the dorsal nerve of the clitoris (N393).
There is no corpus spongiosum in females, but the structures corresponding to the bulb of the penis are the bulbs of the vestibule (Fig. 9A; G11 3.42D, 3.54A; G12 3.48D, 3.62A; N358, 359). These are elongated erectile bodies deep to the labia minora on either side of the vestibule. The bulbs have a slender connection anteriorly with the glans of the clitoris. Each bulb of the vestibule is covered by a bulbospongiosus muscle (Fig. 9B; G11 3.42E, 3.56, Table 3.6 [p. 246]; G12 3.48E, 3.61, Table 3.9 [p. 256]; N358, 359, 375).
Located deep to the posterior end of each bulb of the vestibule, and partly hidden by it, is a greater vestibular (Bartholin’s) gland (G11 3.42D, 3.54A, 3.57; G12 3.48D, 3.62A, 3.64; N358, 359, 384). The greater vestibular gland corresponds to the bulbourethral gland of the male but is located within the superficial perineal pouch rather than within the deep perineal pouch. The duct of the greater vestibular gland opens into the vestibule at the side of the vagina and secretes mucus during sexual arousal.
Trauma to the bulb of the vestibule (e.g., in a high school athlete who falls while jumping high hurdles) may result in hematoma formation in the labia majora (e.g., see http://emedicine.medscape.com/article/270286-overview#showall ). The greater vestibular gland may be the site of an adenocarcinoma or can become infected and inflamed (Bartholinitis). An infected gland may swell to 4 cm or more.
The vestibule is the space between the labia minora (Fig. 17; G11 3.52A, 3.53-3.56; G12 3.47B, 3.59, 3.61-3.63; N356, 359). The urethra descends through the urogenital diaphragm, where it is surrounded by the external urethral sphincter, to open into the anterior part of the vestibule at the external urethral orifice. On each side of the external urethral orifice is the opening of a duct of the paraurethral glands. Behind the external urethral orifice is the vaginal orifice. Its size and appearance varies with the condition of the hymen, a thin annular fold of mucous membrane around the circumference of the vaginal orifice. The hymen partly closes the opening of the vagina but ruptures when a woman first becomes sexually active or as a result of vigorous physical exertion in female athletes, so that only fragments (hymenal caruncles) remain. The hymen has no known function.
The superficial perineal muscles are located within the superficial perineal pouch (Fig. 9B; G11 3.42E, 3.56, Table 3.6 [p. 246]; G12 3.48E, 3.61, Table 3.9 [p. 256]; N357, 358, 375). They consist of the superficial transverse perineal muscles, the bulbospongiosus muscles, and the ischiocavernosus muscles. The two superficial transverse perineal muscles pass medially from the ischial tuberosities along the posterior border of the perineal membrane to attach to the perineal body. Along with the other muscles that attach at the perineal body, the superficial transverse perineal muscles help to stabilize the urogenital diaphragm and floor of the pelvis, resisting increases in intra-abdominal pressure.
The bulbospongiosus muscle on each side covers the bulb of the vestibule and the greater vestibular gland superficially (Fig. 9B; G11 3.42E, 3.54A, 3.56; G12 3.48E, 3.61, 3.62A; N358, 375). Posteriorly, fibers of the bulbospongiosus attach to the perineal body. The anterior end of the bulbospongiosus passes to the pubic arch and corpora cavernosa and blends with the ipsilateral ischiocavernosus muscle. The bulbospongiosus compresses the bulb of the vestibule and greater vestibular gland. The former action reduces venous outflow so that the bulb of the vestibule becomes firm.
Each ischiocavernosus muscle covers a crus of the clitoris (Fig. 9; G11 3.42E, 3.56; G12 3.48E, 3.61; N358, 359, 375). The ischiocavernosus takes origin from the ischial tuberosity and ischiopubic ramus and inserts into the crus and the perineal membrane medial to the crus. This muscle helps to maintain erection of the clitoris by compressing veins to restrict venous outflow.
The urogenital diaphragm closes the midline urogenital hiatus of the pelvic diaphragm from below, except where structures traverse the urogenital diaphragm (Fig. 3A). The urogenital diaphragm consists of an inferior fascia, muscular layer, and a superior fascia (Figs. 10A; G11 3.56, 3.57; G12 3.61, 3.64; N358, 359, 384). The inferior fascia of the urogenital diaphragm is the tough, fibrous perineal membrane, which attaches laterally to the ischiopubic rami and in the posterior midline to the perineal body. The perineal membrane provides passive support for the pelvic viscera and attachment for the erectile bodies and their associated muscles. The superior fascia of the urogenital diaphragm is poorly defined. It fuses with the inferior fascia at the anterior and posterior borders of the urogenital diaphragm. At the anterior border their fusion forms a thickened band of connective tissue, the transverse perineal ligament (N348). The transverse perineal ligament lies behind the pubic symphysis and inferior pubic (arcuate) ligament, from which it is separated by a gap. The gap is traversed by the dorsal vein of the clitoris in the female.
The urogenital diaphragm contains a layer of skeletal muscle and connective tissue between the superior and inferior fasciae of the urogenital diaphragm (Fig. 10A). The urogenital diaphragm corresponds to the traditional description of the deep perineal space. Branches of the pudendal nerves and internal pudendal blood vessels traverse the urogenital diaphragm and will be discussed below.
The muscles of the urogenital diaphragm in the female are more complicated than those in the male, with two additional muscles (Fig. 10; G11 3.42B, Table 3.6 [p. 247, upper right]; G12 3.48B, Table 3.9 [p. 256]; N348, 349, 358). There is an external urethral sphincter (sphincter urethrae) surrounding the membranous urethra, as in the male, to provide voluntary control of micturition. The detailed structure of the external urethral sphincter in females is currently a matter of debate. The sphincter urethrovaginalis muscle surrounds the urethra and vagina as a unit. It passes from an origin at the perineal body in an anterior direction around the sides of the vagina and urethra to unite with the muscle of the other side anterior to the urethra. The compressor urethrae passes medially from an origin on the ischiopubic ramus to meet the opposite muscle anterior to the urethra. The sphincter urethrovaginalis and compressor urethrae are considered to be accessory urethral sphincters. Involuntary spasms of the perivaginal muscles (vaginismus) may interfere with pelvic examinations and cause painful sexual intercourse (dyspareunia).
The final muscles of the urogenital diaphragm in the female are the paired deep transverse perineal muscles, which may be smooth muscle. They arise from the ischial tuberosities and pass medially at the posterior edge of the urogenital diaphragm to attach to the perineal body. Therefore, the deep transverse perineal muscles join the superficial transverse perineal muscles, sphincter urethrovaginalis, bulbospongiosus, external anal sphincter, levator ani, and the perineal membrane in attaching into the perineal body. The attachment of muscles that cross the pelvic outlet and of the perineal membrane into the perineal body helps to provide support for pelvic viscera, such as the bladder and the uterus. If these attachments are torn during childbirth, the pelvic floor loses support and pelvic organs (e.g., the uterus) may prolapse.
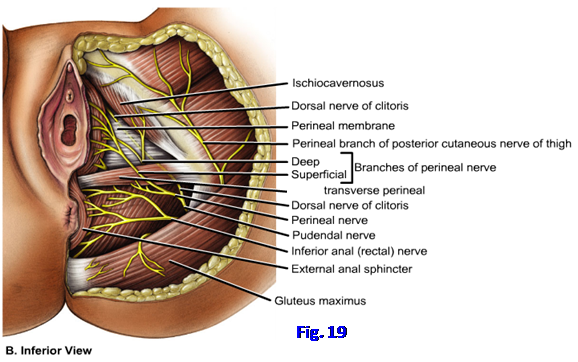
The major nerve and blood supply to the female perineum reaches it via the pudendal canal. The pudendal (Alcock’s) canal is a passageway formed by a split in the obturator internus fascia in the lateral wall of the ischioanal fossa (Fig. 4; G11 3.10A, 3.13C; G12 3.16, 3.22C; N372, 384, 393). The pudendal nerve and the internal pudendal artery and vein enter the pudendal canal from the gluteal region through the lesser sciatic foramen (N491).
The pudendal nerve is formed in the pelvis by the anterior rami of spinal nerves S2-4 (Fig. 14; G11 3.26, Table 3.4 [p. 223]; G12 Table 3.9 [p. 256]; N485, 487). It exits the pelvis via the greater sciatic foramen, curves around the ischial spine or lateral part of the sacrospinous ligament, and enters the perineum via the lesser sciatic foramen. As it enters the pudendal canal, the pudendal nerve gives off the inferior rectal (inferior anal) nerve(s), which supplies the external anal sphincter and perianal skin (G11 3.11, 3.52B, 3.53; G12 3.59, 3.60; N393). Near the proximal end of the pudendal canal, the pudendal nerve divides into its two terminal branches, the perineal nerve and the dorsal nerve of the clitoris (Fig. 19; G11 3.52B; G12 3.60; N393). Within the pudendal canal the perineal nerve usually lies inferior (superficial) to the internal pudendal artery. The perineal nerve branches into the superficial perineal nerves and the deep perineal nerve. Superficial perineal nerves become the posterior labial nerves, which provide cutaneous innervation to the posterior aspect of the labia majora and labia minora and vestibule (G11 3.53; G12 3.59; N393). The deep perineal nerve supplies the muscles of the superficial (e.g., bulbospongiosus) and deep (e.g., external urethral sphincter) perineal pouches.
The dorsal nerve of the clitoris is the primary sensory nerve of the clitoris, especially the sensitive glans. It arises near the proximal end of the pudendal canal (Fig. 19; G11 3.52B; G12 3.60A; N393, 394) and passes forward in the canal superior (deep) to the internal pudendal artery. From the pudendal canal the dorsal nerve of the clitoris enters the urogenital diaphragm (deep perineal pouch) (G11 3.57; G12 3.64; N393). It passes onto the dorsum of the clitoris, where it runs with the dorsal artery of the clitoris (G11 3.54; G12 3.62; N 359).
The female perineum receives additional sensory innervation. The mons pubis and anterior aspect of the labia receive cutaneous innervation from the anterior labial nerves, which arise from the ilioinguinal nerve and genital branch of the genitofemoral nerve (G11 2.11A & C, 3.53; G12 2.11A-C, 3.59; N393). Laterally on each side is a small contribution from the perineal branch of the posterior femoral cutaneous nerve (G11 3.53; G12 3.59; N393).
To relieve perineal pain during childbirth, a local anesthetic is injected around the pudendal nerve (pudendal nerve block) as it crosses the sacrospinous ligament at the ischial spine. This may be done intravaginally or percutaneously but is done carefully because the fetus’ head is usually positioned within the lesser pelvis at this stage. To abolish pain from the anterior portion of the perineum, the ilioinguinal and genitofemoral nerves must also be blocked. Following these nerve blocks, patients may continue to experience perineal pain due to overlapping innervation from the perineal branch of the posterior femoral cutaneous nerve. Local anesthesia of the perineal nerve supply doesn’t block pain from the upper part of the birth canal.
Postganglionic sympathetic nerve fibers are carried to the perineum mainly by the pudendal nerve and its branches. The sympathetic fibers supply cutaneous vessels and glands. Parasympathetic nerve fibers from the uterovaginal plexuses descend through the pelvic floor as cavernous nerves to reach the clitoris and bulbs of the vestibule. The preganglionic parasympathetic fibers arise in the pelvic splanchnic nerves from spinal nerves S2-4 and join the inferior hypogastric plexuses, of which the uterovaginal plexuses are subdivisions (G11 3.37B; G12 3.40; N392). The parasympathetic fibers are responsible for the engorgement of erectile tissues.
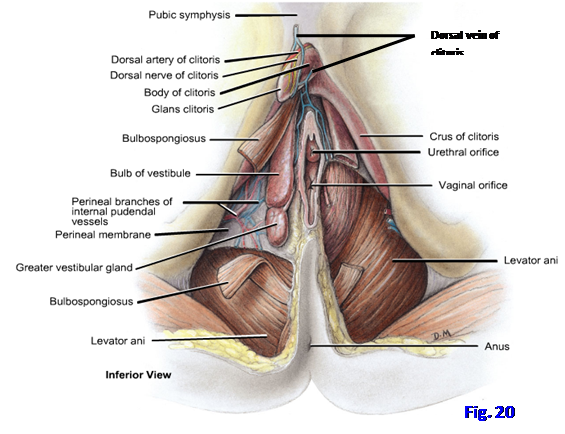
The blood supply to the perineum is mainly from the internal pudendal artery (Fig. 15; G11 Table 3.5 [pp. 234-235]; G12 3.39A, Table 3.7 [p. 243]; N382, 384). It arises from the anterior trunk of the internal iliac artery and leaves the pelvis through the greater sciatic foramen. The internal pudendal artery follows the pudendal nerve’s short passage through the gluteal region (G11 5.25; G12 5.27A), around the ischial spine, and into the lesser sciatic foramen to reach the perineum. As the internal pudendal enters the pudendal canal, it gives off inferior rectal (inferior anal) arteries to the external anal sphincter and perianal skin (G11 3.53; G12 3.59). The internal pudendal artery travels anteriorly within the pudendal canal sandwiched between the perineal nerve superficial to it and the dorsal nerve of the clitoris deep to it. The perineal artery branches from the internal pudendal near the anterior end of the pudendal canal (G11 3.53, 3.54; G12 3.59, 3.62; N384). The perineal artery sends posterior labial branches to accompany the nerves of the same name to the posterior aspect of the labia and the structures of the superficial perineal pouch.
At the anterior end of the pudendal canal, the internal pudendal artery enters the urogenital diaphragm with the dorsal nerve of the clitoris. Within the urogenital diaphragm, the internal pudendal gives off an artery to the bulb of the vestibule (N359, 384) and continues forward. The artery to the bulb of the vestibule pierces the perineal membrane to reach the bulb. The terminal branches of the internal pudendal artery are the deep and dorsal arteries of the clitoris. The deep artery of the clitoris pierces the perineal membane to enter the deep surface of the crus of the clitoris. It travels forward in the center of the corpus cavernosum. The dorsal artery of the clitoris pierces the perineal membrane in company with the dorsal nerve of the clitoris and runs along the dorsum of the body of the clitoris, usually medial to the nerve (Fig. 20; G11 3.54, 3.57; G12 3.62, 3.64; N359, 384).
The tributaries of the internal pudendal vein largely correspond to the branches of the artery, except for the dorsal vein of the clitoris. The dorsal vein of the clitoris (Fig. 20) divides and sends venous blood from the skin and superficial fascia bilaterally into the superficial external pudendal veins. The dorsal vein then pierces the suspensory ligament of the clitoris and traverses the gap between the transverse perineal ligament and inferior pubic ligament to enter the pelvis to reach the vesical venous plexus (N342, 359). (Note: Some authors describe separate superficial and deep dorsal veins of the clitoris corresponding to those of the penis in the male.)
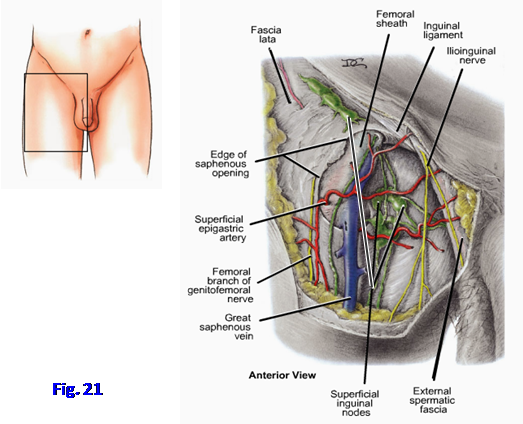
Most of the lymphatic drainage from the perineum goes to the superficial inguinal lymph nodes, which are located just below the inguinal ligament in the upper anterior thigh (Fig. 21; G11 5.11B, 5.12; G12 5.13, 5.15C; N 386-388, 473). This includes lymphatic drainage from the anal canal below the pectinate line and from the urogenital triangle. A significant exception in males is the testes, from which lymph vessels follow the testicular arteries back to the lateral aortic (lumbar) nodes. In females, a clinically significant side note is that uterine cancer occasionally metastasizes along lymphatic vessels that accompany the round ligament of the uterus to the labium majus. From the labium majus, cancer cells pass to the superficial inguinal nodes, and their enlargement may be the first sign of uterine cancer.
DISSECTION OF THE FEMALE UROGENITAL TRIANGLE
25. The clitoris should have been sagittally sectioned when the pelvis and perineum were bisected. If the cut was off center, the body and glans of the narrow clitoris may be located completely on one side. Go to the side of the perineum that has the larger portion and identify the clitoris. Look for the suspensory ligament of the clitoris, a fibrous condensation of deep fascia descending from the pubic symphysis. The body of the clitoris corresponds to the body of the penis in the male but has no corpus spongiosum and is unrelated to the urethra (Figs. 18, 20). The body of the clitoris is formed by fusion of the two corpora cavernosa. The body terminates anteriorly in the glans of the clitoris, which is the rounded tubercle between the prepuce of the clitoris and the frenulum of the clitoris (Fig. 17B; G11 3.56; G12 3.61; N356). Identify the origins of the prepuce and frenulum in folds arising from the anterior end of the labium minus to meet those of the opposite side in the midline. Be aware of the dorsal vein of the clitoris, dorsal arteries of the clitoris, and dorsal nerves of the clitoris (Fig. 20), but don’t attempt to find them on the body of the clitoris. The dorsal vein of the clitoris drains, in part, into the vesicle venous plexus within the pelvis via a gap between the transverse perineal ligament and the inferior pubic ligament.
26. Identify the labium majus and labium minus and carefully remove the skin from them. Attempt to clean the posterior labial nerves and posterior labial arteries within superficial fascia as they approach the labia from the anterior portion of the pudendal canal. These are the continuation of superficial perineal branches of the pudendal nerve and the internal pudendal artery, respectively (Fig. 19). Their origin will be traced shortly.
27. Note that the fatty layer of superficial perineal fascia is continuous with the corresponding fascial layer laterally in the thigh and posteriorly in the anal triangle. Anteriorly, the fatty layer is continuous through the mons pubis with Camper’s fascia of the anterior abdominal wall. The membranous layer of superficial perineal fascia (Colles’ fascia) attaches posteriorly to the posterior border of the perineal membrane and laterally to the fascia lata of the upper thigh. Anteriorly, Colles’ fascia is continuous with Scarpa’s fascia. Be aware of, but don’t attempt to demonstrate, these relationships.
28. Examine the vestibule of the vagina (Figs. 17, 20). Verify that the urethra opens into the vestibule anteriorly and the vagina opens into it posteriorly. If the sagittal section missed the urethra, use small scissors to trim away tissue and open the urethra. Study its course through the urogenital diaphragm from the bladder. This is the route that a catheter or cystoscope must take. The tiny opening of the duct of the greater vestibular gland can sometimes be seen within the vestibule lateral to the vaginal orifice.
29. Remove any remaining skin from the labium majus and labium minus. Bluntly dissect through and remove the superficial fascia from over the urogenital triangle to expose the muscles of the superficial perineal pouch. The muscles are covered by a thin layer of deep perineal fascia. The superficial transverse perineal muscles run parallel to the posterior border of the urogenital diaphragm. They are variable in size and degree of development, but attempt to find this muscle on the hemipelvis you are studying. Next palpate the bulb of the vestibule as a firm body just lateral to the vestibule, deep to where the labium minus was removed. The bulbospongiosus is a thin layer of skeletal muscle covering the superficial surface of the bulb of the vestibule. Carefully clean the bulbospongiosus.
30. There are two ways to find the ischiocavernosus muscle. One way is to palpate the ischial tuberosity and follow the ischiopubic ramus anteriorly and superiorly from it. The ischiocavernosus covers the crus of the clitoris, which is attached to the anterior portion of the ischiopubic ramus. The other way to find the ischiocavernosus is to follow the corpus cavernosum from the body of the clitoris proximally to the crus (Fig. 9A). Reflect the thin ischiocavernosus muscle on one side of the perineum to expose the crus.
31. Between the bulbospongiosus and ischiocavernosus muscles locate a tough, often glistening, fibrous sheet. This is the perineal membrane, which is the inferior fascia of the urogenital diaphragm (Figs. 9, 10A, 19). Push against the perineal membrane to verify its toughness. The perineal membrane provides passive support for the anterior pelvic organs, such as the uterus, as well as attachment for the erectile bodies and their covering muscles.
32. On one half of the perineum open the urogenital diaphragm (deep perineal pouch) by carefully removing the perineal membrane. The external urethral sphincter and other muscles of the urogenital diaphragm are difficult to distinguish in dissection, but be aware of their basic arrangement (Fig. 10A).
33. Now go to the lateral wall of the ischioanal fossa and locate the pudendal canal. This can be done either by tracing the posterior labial nerves and vessels to their origin from the pudendal nerve and internal pudendal vessels, respectively, or by palpating neurovascular structures through the obturator internus fascia (Figs. 4, 5; N384, 393). Using blunt dissection open the pudendal canal. Verify that from superficial to deep (i.e., from inferior to superior) the contents of the pudendal canal are the perineal nerve, internal pudendal vessels, and dorsal nerve of the clitoris.
34. Follow the internal pudendal artery from the pudendal canal into the substance of the urogenital diaphragm. The internal pudendal artery gives off the artery to the bulb of the vestibule before dividing into the deep artery of the clitoris and the dorsal artery of the clitoris (N359, 384). These correspond to arteries in the male. Find the artery to the bulb of the vestibule piercing the perineal membrane to enter the bulb. Clean the deep artery of the clitoris. It pierces the perineal membrane distally to enter the crus of the clitoris. The dorsal artery of the clitoris joins the dorsal nerve of the clitoris to travel along the dorsum of the clitoris (Fig. 20). These arteries may be difficult to demonstrate. XXX
SELECTED REFERENCES
Barber, M. D. 2005 Contemporary views on female pelvic anatomy. Cleveland Clinic Journal of Medicine, Vol. 72, Suppl. 4, S3-S11.
Wallner C., Dabhoiwala N. F., DeRuiter M. C., and Lamers W. H. 2008 The anatomical components of urinary continence. European Urology ( http://www.europeanurology.com/article/S0302-2838(08)00973-1/fulltext ).
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.