Triangles of the Neck I
The sternocleidomastoid (SCM) muscle is the principal muscular landmark of the neck (G11 Tables 8.2, 8.3 [pp. 724-725]; G12 Tables 8.2, 8.3 [pp. 752-753]; N26). It divides the neck between the anterior border of the trapezius and the anterior midline into a posterior cervical triangle (posterior triangle of the neck, lateral cervical region) and an anterior cervical triangle (anterior triangle of the neck, anterior cervical region). Therefore, the posterior cervical triangle is bounded by the anterior border of the trapezius, posterior border of the SCM, and middle third of the clavicle. The anterior cervical triangle is bordered by the anterior border of the SCM, the midline of the neck, and the lower border of the mandible.
Several structures are located within the superficial fascia overlying the posterior and anterior cervical triangles. The platysma muscle is a muscle of facial expression, which has an attachment from the pectoral fascia over the upper part of the pectoralis major and ascends superficial to the clavicle and SCM to reach the lower border of the mandible and corner of the mouth (G11 Tables 7.1 [p. 603], 8.1 [p. 722], Fig. 8.3; G12 Tables 7.1 [p. 629], 8.1 [p. 722], Fig. 8.5; N25). The platysma, like the other muscles of facial expression, develops from the second pharyngeal arch of the embryo and is innervated by the facial nerve (CN VII).
Deep to the platysma, but superficial to the SCM, are the external jugular vein and cutaneous branches of the cervical plexus of nerves. The external jugular vein is formed near the angle of the mandible by the union of the posterior division of the retromandibular vein and the posterior auricular vein (G11 8.3, 8.4; G12 8.2, 8.5; N30, 31). It descends vertically across the SCM and pierces the investing layer of deep cervical fascia (N27, 30) to end in the subclavian vein. If the external jugular is severed where it pierces the investing layer of deep cervical fascia, the lumen is held open by fascia and air may be sucked into it to obstruct blood flow through the right side of the heart (venous air embolism). The chain of superficial cervical lymph nodes follows the external jugular vein. The superficial cervical chain receives lymph mainly from the posterior and posterolateral scalp regions via regional nodes and drains into the deep cervical lymph nodes located along the internal jugular vein.
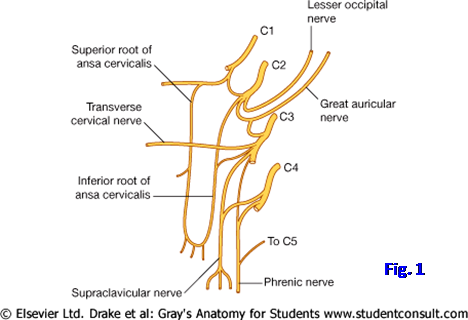
The cervical plexus of nerves is formed by the anterior rami of spinal nerves C1-4. Its cutaneous branches arise from nerve loops between adjacent anterior rami and enter subcutaneous tissue near the middle of the posterior border of the sternocleidomastoid muscle (Fig. 1; G11 8.3A, Table 8.6 [p. 760]; G12 8.5A-B; N2, 31, 32). The lesser occipital nerve (C2) ascends roughly parallel to the posterior border of the SCM to help innervate the scalp. The great auricular nerve (C2,3) ascends vertically across the SCM parallel to the external jugular vein to supply skin over the angle of the mandible, lower part of the auricle, and mastoid process. The transverse cervical nerve (C2,3) passes horizontally forward across the SCM to supply skin over most of the anterior triangle of the neck. The supraclavicular nerves (C3,4) descend to supply skin over the base of the neck and upper thorax from the manubrium as far laterally as the acromion (N30). There typically are medial, intermediate, and lateral supraclavicular branches. Pain referred from the diaphragmatic pleura or peritoneum (e.g., in cholecystitis) by the phrenic nerves to spinal cord segments C3,4 may be “felt” by the patient as ipsilateral shoulder pain in the distribution of the supraclavicular nerves.
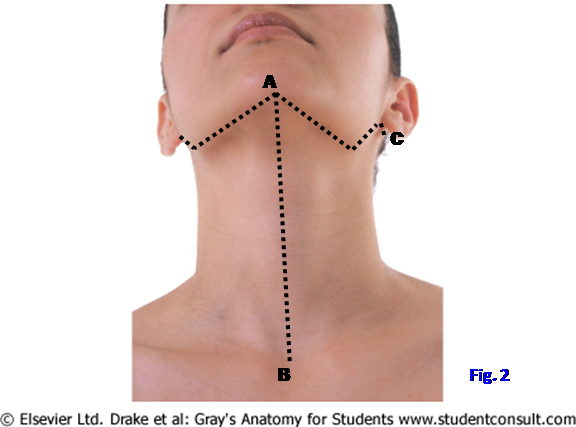
1. THE FOLLOWING INCISION NEEDS TO BE VERY SHALLOW! MAKE AN INCISION THROUGH SKIN ONLY down the anterior midline of the neck from the mental protuberance of the mandible to the suprasternal notch (Fig. 2, A⇒B). From the top of the first incision cut the skin along the inferior border of the mandible on the left side as far laterally as the angle of the mandible, from the angle to the external ear, under the ear, and posteriorly until you reach the previously dissected area (A⇒C). Make the equivalent incision on the right side. Carefully remove the skin from the neck, leaving the thin subcutaneous platysma muscle intact. Reflect the platysma muscle superiorly and medially toward its mandibular and facial attachments.
2. Identify and clean the external jugular vein as it descends across the SCM muscle. Dissect and preserve the cutaneous branches of the cervical plexus—the lesser occipital, great auricular, transverse cervical, and supraclavicular nerves. Look for the lesser occipital nerve coursing roughly parallel to the posterior border of the SCM. The great auricular nerve ascends parallel to, and usually just behind, the external jugular vein. The transverse cervical nerve passes anteriorly, almost horizontally, across the SCM and divides into branches to supply skin over most of the anterior triangle of the neck. Look for the medial, intermediate, and lateral branches arising from the supraclavicular nerve to descend superficially across the clavicle. XXX
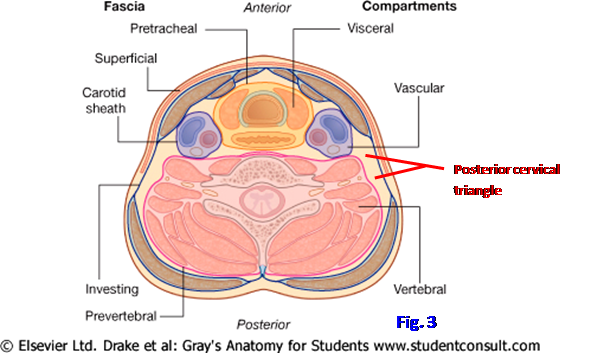
Deep to the superficial fascia (subcutaneous connective tissue) of the neck, the outermost layer of deep fascia is the investing layer of deep cervical fascia (Fig. 3; G11 8.1B; G12 8.1C; N25, 27, 34). The investing layer encloses a series of smaller cylindrical compartments formed by other parts of the deep fascia. Fascial planes between these layers allow the easy separation of tissues during surgery and direct the spread of infection in specific directions, although abscesses occasionally rupture through adjacent fascial layers. Pretracheal fascia encloses the cervical portions of the respiratory and digestive systems within the visceral compartment. Prevertebral fascia encloses the vertebral column and associated muscles within the vertebral compartment. The carotid sheath encloses the carotid artery, internal jugular vein, and vagus nerve (CN X) within a vascular compartment on each side. The investing layer of deep cervical fascia is the roof of the posterior cervical triangle and the prevertebral fascia and underlying muscles form the floor (Fig. 3).
The inferior belly of the omohyoid muscle subdivides the posterior triangle into the small, inferior subclavian (supraclavicular, omoclavicular) triangle and the larger occipital triangle (N26). The pulse of the subclavian artery can be felt within the subclavian triangle, and the artery can be compressed against the first rib there to control axillary or upper extremity bleeding.
The main structure within the occipital triangle is the accessory nerve (CN XI). It descends obliquely through the triangle from a point near the junction of the upper and middle thirds of the posterior border of the SCM to disappear deep to the trapezius about 5 cm above the clavicle (G11 8.3A-C; G12 8.5A, D-E; N31, 126). The accessory nerve supplies motor innervation to both the sternocleidomastoid and trapezius muscles. Branches from spinal nerves C3 and C4 carrying proprioceptive fibers may join the accessory nerve or may enter the trapezius separately. The accessory nerve is commonly injured during surgery in the posterior cervical triangle (iatrogenic injury) with paralysis of the trapezius. The shoulder droops and the patient may have difficulty raising his arm above the horizontal plane due to weakened scapular rotation. The nerve supply of the trapezius can be tested by asking the patient to shrug his/her shoulder against resistance.
Other contents of the posterior triangle of the neck include the transverse cervical (cervicodorsal) and suprascapular arteries and veins (G11 8.3D, 8.7A, 8.20; G12 8.5F, 8.17A, Table 8.5 [p. 765], 8.17A; N31, 32). Both arteries are branches of the thyrocervical trunk from the first part of the subclavian artery and pass anterior to the anterior scalene muscle. The transverse cervical artery courses posteriorly and laterally within the posterior triangle to disappear deep to, and supply, the trapezius muscle. Sometimes the transverse cervical artery divides into a superficial branch and a deep branch. The superficial branch (superficial cervical artery) descends in the fascial interval between the trapezius and the levator scapulae and rhomboid muscles (N171). The deep branch (dorsal scapular artery) courses deep to the rhomboids. Alternatively, a dorsal scapular artery may branch directly from the third part of the subclavian artery to supply the levator scapulae and rhomboids (N415).
A group of lymph nodes along the transverse cervical artery and vein, the supraclavicular lymph nodes, are often hard and enlarged as the first sign of thoracic or abdominal cancers. For that reason, they have been referred to as “sentinel nodes,” but that term now is usually reserved for the first lymph node(s) to receive lymph from a cancer-containing area.
The suprascapular artery courses laterally behind the clavicle and joins the suprascapular nerve en route to the suprascapular notch (G11 6.11A-B, 6.27; G12 6.7A-B, 6.39; N31, 32, 415), where the artery passes above the superior transverse scapular ligament. The suprascapular artery and nerve supply the supraspinatus and infraspinatus muscles. A lesion of the suprascapular nerve results in inability to initiate abduction of the arm and weakened lateral rotation. Importantly, the artery participates in the collateral circulation around the scapula that may allow safe ligation of the axillary artery proximal to its subscapular branch (G11 6.11A-B; G126.7A-B; N415).
3. Bluntly dissect through the tough fascia of the posterior cervical triangle in a posteroinferior direction beginning about the junction of the upper and middle thirds of the sternocleiodmastoid. This will expose the accessory nerve. Next clean the transverse cervical and suprascapular arteries. The transverse cervical artery traverses the lower part of the triangle, passing posteriorly and laterally from behind the SCM to disappear deep to the trapezius. Is there a division of the transverse cervical artery into superficial and deep branches on this side? If there is, remember that the deep branch is also termed the “dorsal scapular artery.”
4. Look for the suprascapular artery coursing immediately behind the clavicle. Identify the suprascapular nerve branching from the superior trunk of the brachial plexus (N417, 418). XXX
The prevertebral fascia encloses the vertebral column and associated muscles. Deep to the prevertebral fascia in the floor of the posterior triangle, from superior to inferior, are the splenius capitis; levator scapulae; and posterior, middle, and anterior scalene muscles (N26).
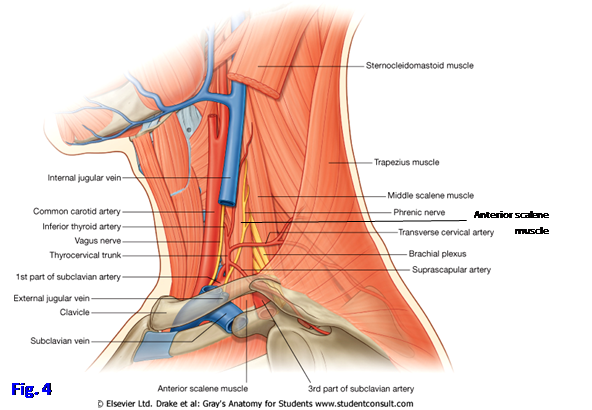
The anterior scalene muscle is one of the principal landmarks of the neck (Fig. 4; G11 8.3 C-D, 8.20, 8.22; G12 8.5E-F, 8.17A-B; N 29, 31). It descends from the anterior tubercles of vertebrae C3-6 to attach to the first rib. The subclavian artery and roots of the brachial plexus pass above the first rib behind the anterior scalene, between it and the middle scalene muscle. The subclavian artery becomes the axillary artery at the lateral border of the first rib.
The subclavian vein is the medial continuation of the axillary vein and passes anterior to the anterior scalene. Also located anterior to the anterior scalene muscle are the phrenic nerve (C3,4,5) descending medially across its surface and the transverse cervical and suprascapular arteries passing laterally into the posterior triangle (Fig. 4).
Review the structure of the brachial plexus (N418). The brachial plexus is formed by the anterior rami of spinal nerves C5-T1. The anterior rami of C5 and C6 join to form the upper (superior) trunk. C7 forms the middle trunk. The anterior rami of C8-T1 form the lower (inferior) trunk. The lower trunk of the brachial plexus and/or the subclavian artery may be stretched over a cervical rib or compressed by a hypertrophied anterior scalene muscle between the anterior and middle scalene muscles. These are two forms of thoracic outlet syndrome.
Each trunk of the brachial plexus splits into an anterior division destined to supply the flexor compartments of the upper extremity and posterior division destined to supply the extensor compartments. The anterior divisions of the upper and middle trunks join to form the lateral cord, and the anterior division of the lower trunk forms the medial cord. The posterior divisions of all three trunks join to form the posterior cord.
The lateral cord of the brachial plexus (C5,6,7) gives off the lateral pectoral nerve (C5,6,7) and then divides into the musculocutaneous nerve (C5,6,7) and lateral root of the median nerve (C5,6,7). The medial cord gives off the medial pectoral nerve, medial brachial cutaneous, and medial antebrachial cutaneous nerves, all containing fibers from C8,T1. The medial cord then divides into the ulnar nerve (C8,T1) and medial root of the median nerve (C8,T1). The posterior cord (C5-T1) gives off upper subscapular (C5,6), middle subscapular [thoracodorsal] (C6,7,8), and lower subscapular (C5,6) branches before dividing into the radial (C5-T1) and axillary (C5,6) nerves. Remember that some branches of a cord do not contain nerve fibers from all of the anterior rami that contribute to that cord (e.g., the posterior cord [C5-T1] gives off the axillary nerve [C5,6]).
Other branches of the brachial plexus include the dorsal scapular nerve from the anterior ramus of C5 and the suprascapular nerve (C5,6) and the nerve to the subclavius (C5) from the upper trunk. The nerve to the subclavius may give off an accessory phrenic branch containing nerve fibers from C5. This is clinically important if the phrenic nerve has to be crushed in a patient with intractable hiccups or to rest a lung. The long thoracic nerve forms from the anterior rami of C5,6,7 and descends on the superficial surface of the serratus anterior muscle to supply it.
5. Detach the clavicular head of the sternocleidomastoid muscle and reflect it medially. Make two saw cuts through the clavicle ON THE CADAVER’S RIGHT SIDE ONLY, one 5 cm medial to the acromioclavicular joint and the other 4-5 cm lateral to the sternoclavicular joint, and remove the middle portion of the bone. This will expose the divisions of the brachial plexus and allow examination of the plexus from its roots to its terminal branches. Identify each of the components of the brachial plexus. XXX
Now turn your attention to the anterior cervical triangle (anterior cervical region). Deeper structures within the anterior cervical triangle are located partly in relation to palpable bones and cartilages and partly in relation to smaller triangles, which represent subdivisions of the anterior triangle (Fig. 5; G11 8.2A, 8.16B, 8.17A-B; G12 8.3, 8.4A, 8.7B, 8.14A; N15, 27, 28). In the anterior midline, from superior to inferior, palpate the hyoid bone, thyroid cartilage, cricoid cartilage, and tracheal rings of cartilage.
Two of the subdivisions of the anterior cervical triangle are above the hyoid bone (suprahyoid), and two are below the hyoid bone (infrahyoid) (G11 Tables 8.2, 8.3 [pp. 724-725], Figs. 8.8, 8.9 [Note: in Fig. 8.9 the superior thyroid artery is mislabeled]; G12 Tables 8.2, 8.3 [p. 752-753], Figs. 8.9A, 8.10; N 26-28, 31). The two suprahyoid triangles are the submandibular and submental triangles, and the two infrahyoid triangles are the carotid and muscular triangles. The submandibular triangle is named for the presence of the large submandibular gland, one of the three major pairs of salivary glands. It also contains submandibular lymph nodes, which may be enlarged in facial and some oral cavity infections or cancer, and part of the hypoglossal nerve (CN XII). The boundaries of the submandibular triangle are the inferior border of the mandible and the anterior and posterior bellies of the digastric muscle.
The submental triangle is bounded by the midline of the neck, the hyoid bone, and the anterior belly of the digastric muscle. (Note: some authors describe a single submental triangle between the anterior bellies of the right and left digastric muscles.) The submental triangle contains submental lymph nodes and tributaries of the anterior jugular vein (N30, 72).
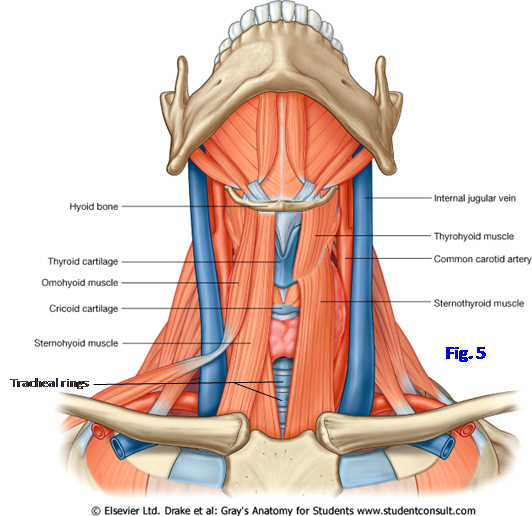
The carotid triangle is named for the ease of approach through it to the carotid arterial system. It is bounded by the SCM, posterior belly of the digastric muscle, and superior belly of the omohyoid muscle. The carotid triangle contains the terminal portion of the common carotid artery and its bifurcation into the internal and external carotid arteries (N27, 31, 33). This is a region of special importance due to the frequent development of atherosclerosis at the origin of the internal carotid artery. The atherosclerotic plaque may have to be surgically removed (carotid endarterectomy) to prevent a transient ischemic attack (TIA) or cerebrovascular accident (stroke) [for more on TIA, see http://www.nejm.org/doi/full/10.1056/NEJMcp020891 ].
The muscular triangle contains the infrahyoid muscles and viscera, such as the thyroid gland. It is bounded by the superior belly of the omohyoid muscle, anterior border of the SCM, and the midline of the neck.
Within the superficial fascia overlying the anterior triangle are the upper portion of the platysma muscle, anterior jugular vein(s), and branches of the transverse cervical nerve (G11 8.3A, 8.4A, 8.16A-B; G12 8.2, 8.5A-B, 8.6, 8.7B; N2, 24, 25). The platysma muscle has already been described. It is innervated by the cervical branch of the facial nerve (CN VII), which descends to it from posterior to the angle of the mandible.
The anterior jugular vein is formed by the convergence of submental veins and descends just lateral to the midline (N30). The anterior jugular veins of the two sides typically communicate by a jugular venous arch located in a split in the investing layer of deep cervical fascia, the suprasternal space, just superior to the suprasternal notch. The jugular venous arch is in danger during a tracheostomy. Occasionally, a single median anterior jugular vein is present instead of right and left veins. A communicating vein connecting the facial vein and anterior jugular vein along the anterior border of the SCM sometimes is quite large (G11 8.4A, 8.16A-B; G12 8.2A, 8.6, 8.7B; N30). The lower part of the anterior jugular vein passes laterally deep to the SCM and is a tributary of the external jugular vein.
The transverse cervical nerve (C2,3) is a cutaneous branch of the cervical plexus. It passes anteriorly, almost horizontally, across the sternocleidomastoid muscle deep to the platysma and divides into branches that pierce the platysma to supply the skin over the anterior triangle (N2, 30).
6. If the platysma muscle hasn’t been reflected superiorly to the lower border of the mandible, please do so now. Clean the anterior jugular veins and find the jugular venous arch. Again identify the transverse cervical nerves. Sever the sternal attachment of the sternocleidomastoid and reflect the muscle superiorly, preserving the transverse cervical nerve if possible. XXX
The infrahyoid muscles are called “strap muscles” due to their appearance (Fig. 6; G11 8.8- 8.10, 8.16B-C, Table 8.5 [p. 740]; G12 8.7B, 8.9A, 8.10, 8.11, 8.13A, Table 8.4 [p. 761]; N 26-28). They are arranged in two layers on each side of the anterior midline. The superficial layer consists of the medial sternohyoid muscle and the lateral omohyoid muscle. The deep layer is formed by the sternothyroid and thyrohyoid muscles. The sternohyoid muscle passes superiorly to the hyoid bone from the posterior aspect of the manubrium and medial end of the clavicle.
The omohyoid muscle consists of two bellies joined by an intermediate tendon. The inferior belly is attached to the superior border of the scapula just medial to the suprascapular notch. It passes anteriorly, subdividing the posterior cervical triangle into occipital and subclavian triangles. The superior belly of the omohyoid is attached to the hyoid bone just lateral to the sternohyoid muscle. The intermediate tendon is bound to the medial end of the clavicle by a fascial sling. The sternohyoid and omohyoid muscles depress the hyoid bone or fix it in position from below (stabilize it).
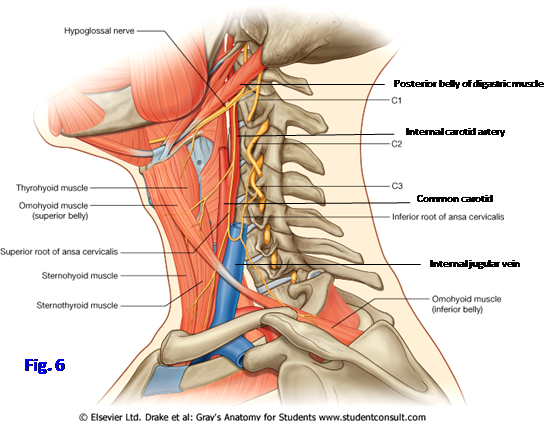
The sternothyroid muscle ascends from the posterior surface of the manubrium to the oblique line of the thyroid cartilage (G11 8.16C, 8.34; G12 8.13A, 8.28; N28, 77). The thyrohyoid is a short muscle that passes from the oblique line to the hyoid bone. The sternothyroid muscle depresses the larynx and the thyrohyoid elevates it. Acting together, the sternothyroid and thyrohyoid muscles can depress or stabilize the hyoid bone.
The infrahyoid muscles are innervated by a nerve loop (ansa), the ansa cervicalis (Figs. 1, 6; G11 8.8-8.10; G12 8.9-8.11; N 31, 32). The ansa cervicalis is formed at a variable level between the angle of the mandible and the upper border of the clavicle. The superior root from C1 travels with, and appears to branch from, the hypoglossal nerve (CN XII) before descending along the internal and common carotid arteries. The inferior root (C2,3) passes either lateral or medial to the internal jugular vein to join the superior root.
Branches to the sternohyoid, omohyoid, and sternothyroid muscles arise from the ansa cervicalis. The nerve fibers to the thyrohyoid muscle and another suprahyoid muscle, the geniohyoid, travel forward with the hypoglossal nerve after the superior root of the ansa cervicalis separates from it (G11 8.12, 8.13A; G12 8.19A-C; N 32, 33).
7. Clean the fascia from the superficial layer of infrahyoid muscles, preserving the delicate nerves that innervate them. Detach the sternohyoid muscle from the manubrium of the sternum and clavicle and reflect it superiorly to expose the deep layer of infrahyoid muscles. Remove the fascia from the sternothyroid and thyrohyoid muscles. You may have to retract the superior belly of the omohyoid muscle laterally to achieve good exposure.
8. Clean the ansa cervicalis by carefully probing through the carotid sheath enclosing the carotid artery and internal jugular vein. It may be easier either to pick up a muscular branch of the ansa cervicalis and follow it back to the loop or to find the hypoglossal nerve and trace the superior root of the ansa cervicalis as it appears to branch from the hypoglossal. After isolating the muscular branches from the ansa cervicalis, follow the hypoglossal nerve forward until the nerve to the thyrohyoid leaves it to enter that muscle. XXX
The thyroid gland is an “H”-shaped endocrine gland located anterior and lateral to the trachea, partly hidden by the infrahyoid muscles (G11 8.16B-C, 8.17-8.21; G12 8.7B, 8.13A, 8.14-8.17A; N28, 30, 74). The thyroid gland consists of right and left lateral lobes joined across tracheal rings 2-3 by a horizontal isthmus. In some people, a pyramidal lobe extends superiorly from the isthmus and is attached to the hyoid bone by connective tissue or a slender muscle (levator glandulae thyroideae). A pyramidal lobe is a remnant of the thyroglossal duct, which marks the path of migration of the embryonic thyroid gland from the foramen cecum of the tongue into the anterior neck. Occasionally part of the thyroglossal duct persists in children as a midline thyroglossal duct cyst and must be surgically removed (e.g., see http://emedicine.medscape.com/article/845125-overview#showall ). Ectopic thyroid tissue also may be present along the path of migration and may be the only thyroid tissue present, resulting in inadvertent thyroidectomy if it is removed.
Like other endocrine glands the thyroid gland has a rich blood supply (G11 8.6, 8.16D; G12 8.15-16, Table 8.5 [p. 765]; N69, 74-76). The thyroid gland is supplied by the superior thyroid artery from the external carotid, the inferior thyroid artery from the thyrocervical trunk, and 10% of the time by a thyroid ima artery from the brachiocephalic trunk or arch of the aorta. The external branch of the superior laryngeal nerve (external laryngeal nerve) (X) descends with the superior thyroid artery. The recurrent laryngeal branch of the vagus nerve (CN X) ascends in the tracheoesophageal groove close to the inferior thyroid artery (G11 8.16E, 8.20, 8.21; G12 8.15, 8.16A, 8.17A; N74-76).
The external laryngeal nerve may be injured during surgical removal of the thyroid gland (thyroidectomy). The recurrent laryngeal nerve passes either anterior or posterior to the inferior thyroid artery near the inferior pole of the lateral lobe of the thyroid gland and also may be injured during a thyroidectomy or if the thyroid gland is enlarged (goiter). A goiter may compress the trachea and esophagus, resulting in difficulty breathing (dyspnea) and swallowing (dysphagia), respectively (see http://emedicine.medscape.com/article/120034-overview#showall ). Superior enlargement of the thyroid gland is prevented by attachment of the sternothyroid muscle to the oblique line of the thyroid cartilage, and so the gland may enlarge inferiorly behind the sternum (retrosternal goiter) and compress thoracic structures. The thyroid ima artery may be a troublesome source of bleeding during a thyroidectomy or tracheostomy.
The thyroid gland is drained by superior and middle thyroid veins to the internal jugular vein and by one or more inferior thyroid veins to the left brachiocephalic vein (G11 8.16F; G12 8.13; N74). The inferior thyroid vein may be large and can be a source of troublesome bleeding during a tracheostomy.
The parathyroid glands are endocrine glands essential for life. There typically are paired superior and inferior parathyroid glands located on the posterior surface of the lateral lobes of the thyroid gland (G11 8.17C, 8.21, 8.35; G12 8.15B, 8.16A, 8.29A; N75, 76). They are small, oval bodies located within the pretracheal fascia and sometimes inside the fibrous capsule of the thyroid gland. The parathyroid glands typically receive their major blood supply from branches of the inferior thyroid arteries.
The superior parathyroid glands develop from the fourth pharyngeal pouches of the embryo and the inferior glands from the third pharyngeal pouches and migrate to their adult positions. The inferior parathyroid glands are especially variable in position, which is important if one or more must be surgically removed (e.g., to treat parathyroid adenoma; see http://www.ghorayeb.com/parathyroidadenomamethyleneblue.html ). Occasionally the adult inferior parathyroid glands lie close to the thymus, with which they migrated into the superior mediastinum.
9. Cut the manubrial attachment of the sternothyroid muscle on one side and reflect it superiorly to the thyroid cartilage. On both sides trace the descent of the superior thyroid artery from the external carotid artery to the superior pole of the lateral lobe of the thyroid gland. Look for the small external laryngeal nerve descending with the artery. Cut the isthmus of the gland to separate ONE lateral lobe from the trachea. Retract the mobilized lateral lobe of the thyroid gland away from the midline.
10. Find the recurrent laryngeal nerve ascending within the tracheoesophageal groove. Clean the inferior thyroid artery where it crosses the recurrent laryngeal nerve (G11 8.21; G12 8.16A). Look for the parathyroid glands on the posterior surface of the lateral lobe. They often appear as slight areas of discoloration on the thyroid gland and are difficult to find, but they may be traceable by following branches of the inferior thyroid artery. XXX
The carotid triangle is bounded by the sternocleidomastoid (SCM), posterior belly of the digastric, and superior belly of the omohyoid muscles (G11 8.8, 8.9, 8.10A-B, Table 8.2 [p. 724]; G12 8.9A, 8.10, 8.11A-B, Table 8.2 [p. 752]; N27, 31, 33). It contains many important structures, including parts of the carotid arterial system; internal jugular vein; and the vagus, hypoglossal, and glossopharyngeal nerves.
The common carotid artery differs in origin on the two sides (G11 1.42, 1.43, 1.59, 8.6; G12 1.42, 1.43, 1.62, Table 8.5 [pp. 764-765]; N75, 187, 231). The right common carotid artery branches from the brachiocephalic trunk, and the left common carotid comes directly from the arch of the aorta. The common carotid artery ascends within the carotid sheath and usually has no branches until it reaches the superior border of the thyroid cartilage, where it branches into the external carotid and internal carotid arteries (N69). The common carotid artery crosses over the enlarged anterior tubercle of vertebra Cv6 (carotid tubercle) and may be compressed against it to control bleeding from parts of the carotid arterial system where direct pressure is difficult.
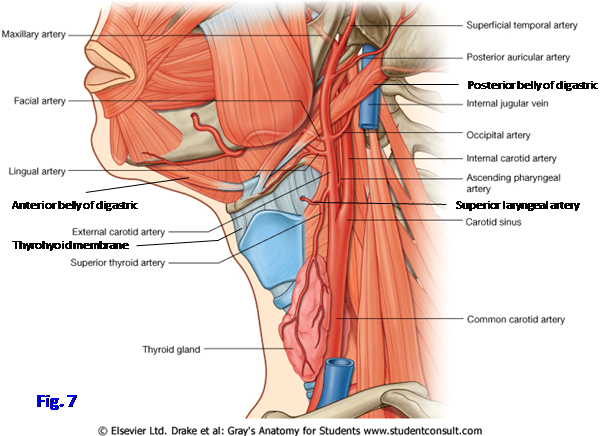
Near the site of bifurcation of the common carotid artery are two specialized sensory receptors, the carotid sinus and the carotid body (Fig. 7; G11 Table 9.11 [p. 816]; G12 Table 9.11 [p. 834]; N71, 124). They are innervated by the carotid sinus branch of the glossopharyngeal nerve (CN IX) and perhaps also by the vagus nerve (CN X). The carotid sinus is a dilatation of the proximal part of the internal carotid artery, and possibly the terminal part of the common carotid, that functions as a baroreceptor responsive to changes in arterial blood pressure.
In some middle-aged and older individuals the carotid sinus becomes hypersensitive to external pressure, which acts reflexly through the vagus nerve to produce a decrease in heart rate and possible fainting (carotid sinus syncope; e.g., see http://emedicine.medscape.com/article/153312-overview#showall ). For this reason, the upper border of the thyroid cartilage is not a good place to check a pulse, especially in elderly individuals or anyone suspected of having cardiovascular disease. Unfortunately, this is exactly where some fitness trainers, and even some health care professionals, are taught to take the pulse (e.g., see Moore p. 610 under “Carotid Pulse”).
The carotid body is a small mass of tissue resembling fat deep (medial) to the bifurcation of the common carotid artery. It contains chemoreceptors for blood gases (e.g., level of blood oxygen) that, when stimulated, produce reflex increases in the rate and depth of respiration.
The external carotid artery has 8 branches, of which 4-5 leave it within the carotid triangle (Fig. 7). The superior thyroid artery arises near the origin of the external carotid artery and descends anteromedially to the apex of the lateral lobe of the thyroid gland, often sharing a fascial covering with the external laryngeal nerve (CN X) (G11 8.9, 8.10B, 8.16C-E; G12 8.10, 8.11B, 8.13A, 8.15A , 8.16A; N69, 74, 75). En route to the thyroid gland the superior thyroid artery gives off a superior laryngeal branch that pierces the thyrohyoid membrane with the internal laryngeal nerve (CN X).
The ascending pharyngeal artery alternates with the superior thyroid as the first or second branch of the external carotid artery. It arises from the deep (medial) side of the external carotid and may be difficult to see from a lateral view (G11 8.28B; G12 8.23A; N33, 69). The lingual artery arises near the level of the greater horn of the hyoid bone (G11 8.6, 8.9, 8.10, 8.13A-B; G12 8.10, 8.11, 8.19D, 8.20, Table 8.5 [p. 765]; N33, 59, 69). It passes above the greater horn, deep to the hypoglossal nerve, and disappears deep to the hyoglossus and mylohyoid muscles.
The facial artery arises from the anterior aspect of the external carotid just superior to the lingual artery or, 20% of the time, in a common faciolingual stem with it (G11 8.9, 8.10, 8.11; G12 8.10, 8.11, 8.19A; N3, 33, 69). The facial artery ascends deep to the posterior belly of the digastric and stylohyoid muscles. It grooves the deep surface of the submandibular gland and crosses the inferior border of the mandible at a shallow notch, which is a pressure point to control bleeding from the facial artery. Before crossing the mandible, the facial artery gives off a small submental artery that runs anteriorly with the mylohyoid branch of the mandibular nerve (CN V3) toward the anterior belly of the digastric muscle (G11 8.9, 8.11; G12 8.10, 8.19A; N39, 69). Note that the facial vein, which is joined by the anterior branch of the retromandibular vein to form the common facial vein, passes superficial to the submandibular gland (G11 8.4A, 8.8, Table 7.4 [p. 607]; G12 8.2A, 8.9A, Table 7.4 [p. 633]; N31, 70). The lingual vein also occasionally joins the common facial vein.
The occipital artery arises from the posterior aspect of the external carotid opposite the facial artery or somewhat higher and may not be located in the carotid triangle at its origin (G11 8.6, 8.9, 8.10A; G12 8.10, 8.11A, Table 8.5 [p. 764]; N3, 33, 69). The occipital artery passes posteriorly along the base of the skull, where it usually causes a shallow groove (G11 7.4A; G12 7.5A; N10), and through the upper part of the posterior cervical triangle to ascend into the back of the scalp with the greater occipital nerve. The artery’s sternocleidomastoid branch hooks over the hypoglossal nerve to descend to the SCM.
11. Clean the common carotid artery superiorly to its bifurcation. Find the carotid sinus swelling at the origin of the internal carotid artery and look for the carotid body deep to the bifurcation. The carotid body may resemble a small glob of fat. Look for the carotid sinus nerve descending between the external and internal carotid arteries.
12. Clean the superior thyroid artery as it descends to the thyroid gland. Find its superior laryngeal branch piercing the thyrohyoid membrane with the internal laryngeal nerve. Look for the small external laryngeal nerve descending with the superior thyroid artery en route to the cricothyroid muscle. Identify the lingual artery arising from the anterior aspect of the external carotid above the superior thyroid artery. Trace it to where it disappears deep to the hyoglossus muscle. Attempt to find the facial artery arising above the lingual artery or from a common faciolingual stem with it and disappearing deep to the submandibular gland. Finding the origin of the facial artery may be difficult at this point in the dissection. Look for the occipital artery arising posteriorly from the external carotid, and identify its sternocleidomastoid branch looping over the hypoglossal nerve to descend to the SCM.
13. Look for the facial and common facial veins. The facial vein descends superficial to the submandibular gland. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.