Triangles of the Neck II
During this period we will complete the dissection of structures of the carotid triangle and will dissect suprahyoid structures of the neck. We will then turn our attention to deep structures at the root of the neck.
The internal jugular vein is the continuation of the sigmoid sinus, the dural venous sinus within the cranial cavity that eventually receives most of the blood from the brain. It begins in a dilatation, the superior bulb of the internal jugular vein, at the jugular foramen in the base of the skull (G11 7.16, 8.5A, 8.9; G12 7.21, 8.10, 8.12; N28, 46, 70, 102, 103). The vein descends within the carotid sheath lateral to the carotid artery and receives several tributaries corresponding to branches of the external carotid artery. Inferiorly the internal jugular vein has an inferior bulb just superior to its union with the subclavian vein to form the brachiocephalic vein. The inferior bulb of the internal jugular vein contains a bicuspid valve that prevents backflow into the vein (e.g., during increased intrathoracic pressure or when Dr. Roy is standing on his head).
Note that the deep cervical lymph nodes form a chain along the internal jugular vein into which all of the lymph of the head and neck drains, either directly or through regional groups of lymph nodes (G11 7.52D, 8.5A, 8.17D, 8.23; G12 7.47D, 7.79D, 8.17C, 8.32; N72, 73). Therefore, the deep cervical nodes and internal jugular vein on one side may have to be removed in a radical neck dissection for cancer (e.g., see http://emedicine.medscape.com/article/849895-overview#showall ). A catheter may be inserted into the internal jugular vein, typically the right one, for diagnostic or therapeutic reasons. One place this is done is through the triangular interval formed with the clavicle by the sternal and clavicular heads of the sternocleidomastoid muscle. Also, remember that jugular venous distention is an indication of obstructed venous return to the right atrium, such as occurs in superior vena cava syndrome, tension pneumothorax, and cardiac tamponade.
The vagus nerve (CN X) exits the cranial cavity through the jugular foramen and descends within the carotid sheath behind and between the carotid artery and internal jugular vein. The superior laryngeal branch of the vagus courses anteriorly and inferiorly to enter the carotid triangle, where it divides into the internal laryngeal and external laryngeal nerves (G11 8.9, 8.10B, 8.16C & E, 8.28A-B, Table 8.7 [pp. 766-767]; G12 8.10, 8.11B, 8.13A, 8.15A, 8.23A-B, Table 8.9 [p. 788]; N71, 74, 76, 125). The internal laryngeal nerve pierces the thyrohyoid membrane between the thyroid cartilage and hyoid bone along with the superior laryngeal artery. The nerve is sensory to the mucosa of the piriform recesses (laryngopharynx), upper half of the larynx, epiglottis, and a small area at the root of the tongue (G11 8.38A, Table 8.8 Posterior View [p. 784]; G12 8.29B, Table 8.10 Posterior View [p. 802]; N62, 71, 76, 80).
The external laryngeal nerve descends with the superior thyroid artery deep to the sternothyroid muscle (G11 8.9B, 8.16C & E, Table 8.7 [pp. 766-767]; G12 8.10, 8.13A, 8.15A Table 8.9 [p. 788]; N71, 74, 125). The nerve innervates the cricothyroid muscle, which is the only intrinsic muscle of the larynx not innervated by the recurrent laryngeal branch of the vagus.
The (spinal) accessory nerve (CN XI) leaves the jugular foramen with the glossopharyngeal and vagus nerves and descends through the uppermost part of the carotid triangle just lateral to the hypoglossal nerve to reach the SCM muscle (G11 8.8, 8.9, 8.10A, Table 9.13 [p. 820]; G12 8.9A, 8.10, 8.11A, Table 9.13 [p. 838]; N31, 33, 126). It passes deep to or through the deep part of the sternocleidomastoid muscle, innervating it. The nerve then enters the posterior triangle en route to the trapezius muscle, where it was seen previously.
The hypoglossal nerve (CN XII) is the motor nerve of the tongue. It exits the skull through the hypoglossal canal and descends between the internal carotid artery and internal jugular vein. The hypoglossal nerve forms a loop slightly below the posterior belly of the digastric and stylohyoid muscles before passing between the mylohyoid and hyoglossus muscles to enter the tongue (G11 8.9, 8.10A-B, 8.11, 8.12, 8.13A; G12 8.10, 8.11A-B, 8.19A-C; N33, 69, 71, 127). As previously seen, the superior root of the ansa cervicalis and nerve to the thyrohyoid muscle (C1) travel with, and appear to branch from, the hypoglossal nerve, but they are actually separate nerves arising from the cervical plexus. Nerve fibers that supply the geniohyoid muscle also travel with the hypoglossal nerve (G11 8.13A, Table 9.14 [p. 821]; G12 8.9B, 8.19C, Table 9.14 [p. 839]; N32, 59, 127).
1. Preserve the previously exposed ansa cervicalis during the following dissection. Carefully remove the remnants of the carotid sheath from the internal jugular vein and look for its superior and middle thyroid tributaries. Briefly look for deep cervical lymph nodes along the internal jugular vein. They may be difficult to demonstrate but remember their clinical significance. Use a probe to separate the common carotid artery and internal jugular vein and clean the vagus nerve. Again find its internal laryngeal branch piercing the thyrohyoid membrane with the superior laryngeal artery and the delicate external laryngeal branch descending with the superior thyroid artery as far as the cricothyroid muscle.
2. Retract the sternocleidomastoid laterally and find the accessory nerve within the uppermost part of the carotid triangle. Clean the posterior belly of the digastric and stylohyoid muscles and find the hypoglossal nerve looping just inferior to them. Again look at the superior root of the ansa cervicalis and the nerve to the thyrohyoid appearing to branch from the hypoglossal nerve. XXX
The suprahyoid region lies between the hyoid bone and the inferior border of the mandible and contains the submandibular and submental triangles. The submandibular triangle is bounded by the inferior border of the mandible and the anterior and posterior bellies of the digastric muscle (G11 8.9, 8.10A-B, 8.11, Table 8.5 [p. 740]; G12 8.10, 8.11A-B, 8.19A, Table 8.4 [p. 761]; N26, 27, 53). The anterior belly of the digastric muscle attaches at the digastric fossa of the mandible (G11 7.44F; G12 7.40F; N17) and descends posteriorly to end in an intermediate tendon. The posterior belly of the digastric attaches in the mastoid notch of the temporal bone, medial to the mastoid process (G11 8.27A; G12 7.5A; N10), and descends anteriorly to the intermediate tendon. The intermediate tendon is bound to the hyoid bone by fascia.
The stylohyoid muscle runs downward from the styloid process of the temporal bone (G11 8.27; G12 7.5B, Table 8.4 [p. 761]; N10, 26) parallel to the posterior belly of the digastric. It splits around the intermediate tendon of the digastric muscle to attach to the hyoid bone, which is a useful landmark.
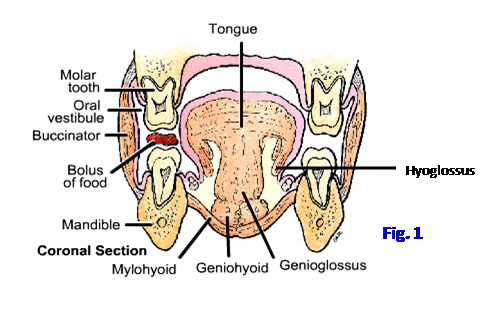
The floor of the submandibular triangle is formed by the mylohyoid and hyoglossus muscles (G11 8.11, 8.12, 8.15A; G12 8.8A-B, 8.19A-B; N26, 27, 68). The mylohyoid muscle has a superior attachment to the mylohyoid line on the medial surface of the body of the mandible (G11 7.44F; G12 7.40F; N17). Its posterior fibers descend to attach to the hyoid bone, and its middle and anterior fibers insert with the muscle of the other side into a median fibrous raphe. The mylohyoid muscles of the two sides form the floor of the oral cavity (Fig. 1; G11 7.53B, 8.11, 8.12, 8.15A; G12 7.48B, 8.8A-B, 8.19A-B; N27, 53). The hyoglossus muscle is one of the extrinsic muscles of the tongue. It takes origin from the greater horn and body of the hyoid bone and passes upward into the tongue (G11 Table 7.11 [p. 667]; G12 Table 7.11 [p. 677]; N53, 59). It will be studied in more detail later.
The anterior belly of the digastric muscle and the mylohyoid muscle are innervated by the mylohyoid branch of the inferior alveolar nerve (V3). The posterior belly of the digastric muscle and sylohyoid develop from the second pharyngeal arch and are innervated by the facial nerve (CN VII).
The submandibular gland is the largest structure within the submandibular triangle (G11 8.8, 8.11, 8.12; G12 8.9A, 8.19A-B; N26, 61). This C-shaped salivary gland wraps around the posterior border of the mylohyoid muscle. The small deep portion of the gland lies within the floor of the oral cavity above the mylohyoid muscle and will be seen during a later dissection.
Two to three large and some smaller submandibular lymph nodes are associated with the submandibular gland (G11 8.8; G12 8.9A; N 72). Lymph from the upper lip, lateral part of the lower lip, and lateral part of the anterior 2/3 of the tongue drains to the submandibular nodes, which in turn drain to the deep cervical lymph nodes (G12 7.47C-D, 7.79). This route of metastasis is clinically important given the incidence of oral cancers among tobacco and alcohol users, but some patients have no known risk factors. Although your dental colleagues may have more opportunities to spot oral cancers (see “Dentist Version” at http://www.ada.org/2607.aspx ), a physician can pick up signs during a routine physical examination.
The facial artery and vein traverse the submandibular triangle deep and superficial, respectively, to the submandibular gland (G11 8.8, 8.9; G12 8.9A, 8.10; N70 [Note in Plate 69 the facial artery uncharacteristically passing superficial to the submandibular gland]). The facial artery gives off the submental branch and then ascends across the lower border of the mandible into the face. The submental artery runs forward with the nerve to the mylohyoid parallel to, and sometimes hidden by, the inferior border of the mandible. The facial vein is joined by the anterior branch of the retromandibular vein to form the common facial vein, which usually drains into the internal jugular vein (G11 8.4A, 8.8, 8.9; G12 8.2A, 8.9A, 8.10; N31, 70). The common facial vein is often cut to provide better exposure during a carotid endarterectomy.
The cervical branch of the facial nerve (CN VII), and sometimes the marginal mandibular branch, emerges from the parotid gland to cross superficial to the submandibular gland or just below it (G11 7.8, 8.3A, 8.8; G12 7.13, 8.5A, 8.9A; N24, 122). The cervical branch supplies the platysma muscle. The marginal mandibular branch supplies muscles of facial expression of the lower lip and chin.
The nerve to the mylohyoid branches from the inferior alveolar nerve (V3) deep to the ramus of the mandible. It descends to run forward approximately parallel to the submental artery near the lower border of the mandible (G11 8.9, 8.11; G12 8.10, 8.19A; N 45, 71). The mylohyoid nerve innervates the mylohyoid and anterior belly of the digastric muscles. These muscles develop from the first pharyngeal arch and, like other first arch muscles, are innervated by branches of the mandibular division of the trigeminal nerve (V3).
The hypoglossal nerve (XII) leaves the carotid triangle to enter the submandibular triangle (G11 8.9, 8.10A-B, 8.11; G12 8.11A-B, 8.19A-C; N33, 59, 71, 127). It has a short course in the submandibular triangle before disappearing deep to the mylohyoid muscle. Pay attention to the fact that the hypoglossal nerve passes lateral (superficial) to the hyoglossus muscle and the lingual artery passes medial (deep) to it. This relationship will be useful when we study the floor of the oral cavity.
3. Find and clean the facial vein superficial to the submandibular gland and the cervical branch of the facial nerve superficial to, or just inferior to, the gland. Identify where the anterior branch of the retromandibular vein joins the facial vein to form the common facial vein. Notice the submandibular lymph nodes before removing them.
4. Clean the fascia from the submandibular gland and mobilize the gland. The superficial portion of the gland may be removed on ONE SIDE of the cadaver. Clean the portion of the facial artery deep to the submandibular gland and follow it to the inferior border of the mandible just anterior to the masseter muscle. Palpate the shallow notch made in the inferior border of the mandible by the artery and appreciate that the facial artery may be compressed there to slow bleeding from the face. When you hands are clean, feel the pulse of your facial artery there. On the cadaver find the submental branch of the facial artery and the accompanying nerve to the mylohyoid.
5. Clean the anterior belly of the digastric muscle. In some individuals the anterior belly of the digastric may have an accessory origin from the hyoid bone (G11 8.11; G12 8.19A) and/or the anterior bellies of the two sides may be fused in the midline. Again look at the slender stylohyoid muscle as it splits around the intermediate tendon of the digastric. Clean the mylohyoid muscle that forms the floor of the submental triangle and most of the submandibular triangle.
6. From where you previously saw the hypoglossal nerve within the carotid triangle, trace it deep to the posterior belly of the digastric muscle and stylohyoid. Note the vertical fibers of the hyoglossus muscle posterior to the mylohyoid. Observe that the hypoglossal nerve disappears from view between the mylohyoid and hyoglossus muscles (N33); therefore, it courses lateral to the hyoglossus muscle. XXX
The root of the neck is the deep portion of the neck lateral to the trachea and esophagus, just above the superior thoracic aperture. It is normally hidden by the intact sternocleidomastoid and infrahyoid muscles. The contents of the root of the neck include parts of the common carotid and subclavian arteries, internal jugular and subclavian veins, thoracic duct (on the left side), vagus nerve and its recurrent laryngeal branch, cervical sympathetic trunk and stellate ganglion, and cervical pleura and apex of the lung.
The common carotid artery has already been studied. The subclavian artery is subdivided into three parts in relation to the anterior scalene muscle (Fig. 2). The first part of the subclavian artery is medial to the anterior scalene and the second part is posterior to the muscle. The third part of the subclavian artery lies between the lateral border of the anterior scalene muscle and the lateral border of the first rib, where the subclavian is continuous with the axillary artery.
The branches of the first part of the subclavian artery are the vertebral artery, thyrocervical trunk, and internal thoracic artery. The vertebral artery ascends slightly posteriorly to enter the transverse foramen of the 6th cervical vertebra at the apex of a triangle formed laterally by the anterior scalene muscle and medially by the longus colli muscle (to be studied later) (Fig. 2; G11 8.22, 8.24; G12 8.17B, Table 8.6 [p. 774-775]; N135, 136, 167). A good landmark in this area is the carotid tubercle, the enlarged anterior tubercle of Cv6. Occasionally the vertebral artery enters the transverse foramen of a vertebra higher than Cv6. The upper part of the vertebral artery was seen within the suboccipital triangle during the deep back dissection (N172). The arteries of the two sides ascend through the foramen magnum and join to form the basilar artery, which supplies the brainstem and posterior aspect of the cerebral hemispheres.
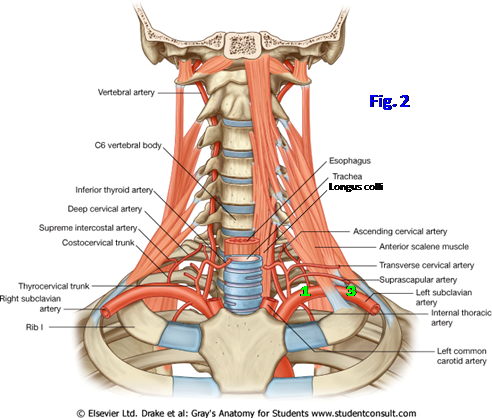
The thyrocervical trunk arises from the first part of the subclavian artery lateral to the vertebral artery. It has three branches (Fig. 2; G11 8.20, 8.24; G12 8.17A, Table 8.6 [pp. 774-775]; N31, 32, 75). The transverse cervical and suprascapular arteries have already been seen passing laterally anterior to the anterior scalene muscle to enter the posterior cervical triangle. The third branch of the thyrocervical trunk is the inferior thyroid artery, which loops medially to reach the lateral lobe of the thyroid gland. Near the inferior pole of the lateral lobe, the inferior thyroid artery is closely related to the recurrent laryngeal nerve.
The inferior thyroid artery gives off the small ascending cervical artery as it starts to turn medially. The ascending cervical artery supplies not only prevertebral muscles but also contributes to segmental medullary arteries, which are important for the blood supply of the spinal cord (N164). (Note: some anatomists consider the ascending cervical artery a fourth branch of the thyrocervical trunk.)
The inferior thyroid artery gives off the small ascending cervical artery as it starts to turn medially. The ascending cervical artery supplies not only prevertebral muscles but also contributes to segmental medullary arteries, which are important for the blood supply of the spinal cord (N164). (Note: some anatomists consider the ascending cervical artery a fourth branch of the thyrocervical trunk.)
The internal thoracic artery branches from the subclavian artery opposite the thyrocervical trunk or just distal to it (G11 1.20, 8.24; G12 1.20, 8.17B, Table 8.6 [p. 774-775]; N183, 184). It descends through the superior thoracic aperture lateral to the sternum. The internal thoracic artery may be used in coronary bypass surgery because it is more durable than a great saphenous vein graft. A radial artery graft may be used instead.
The second part of the subclavian artery has one branch, the costocervical trunk. The costocervical trunk arches posteriorly over the cervical pleura (pleural cupula) and apex of the lung, which project through the superior thoracic aperture into the root of the neck. The costocervical trunk divides into an ascending deep cervical artery and a descending superior (supreme) intercostal artery (G11 8.6A; G12 Table 8.5A [p. 764]; N 135). The deep cervical artery contributes to segmental medullary arteries and then anastomoses with the descending branch of the occipital artery, potentially providing collateral circulation between the subclavian and carotid arterial systems. The superior (supreme) intercostal artery descends anterior to the neck of the first rib and divides into the posterior intercostal arteries of the first two intercostal spaces.
The third part of the subclavian artery often does not give off a branch. When it does, the branch is usually a dorsal scapular artery, which takes the place of the deep branch of the transverse cervical artery, passing deep to and supplying the levator scapulae and rhomboid muscles (G11 6.27B-C, 8.22A; G12 6.39B-C, 8.17B; N31, 415).
7. Clean the first part of the subclavian artery and its branches. Find the vertebral artery as it ascends to the transverse foramen of Cv6. Remove the vertebral vein if it obscures your view. Slightly lateral to the vertebral artery, find the thyrocervical trunk. Clean the origin of its transverse cervical, suprascapular, and inferior thyroid branches. If you have difficulty finding the thyrocervical trunk, follow the previously dissected portion of the transverse cervical or suprascapular artery medially to its origin. Find the small ascending cervical artery branching from the inferior thyroid and ascending on prevertebral muscles. Look for the origin of the internal thoracic artery.
8. With a probe explore the second part of the subclavian artery posterior to the anterior scalene muscle. Attempt to find the origin of the costocervical trunk. Be aware that it divides into the ascending deep cervical artery and descending superior (supreme) intercostal artery, but don’t attempt to clean these branches. Look to see if the third part of the subclavian artery gives off a dorsal scapular artery. XXX
The internal jugular and subclavian veins unite to form the brachiocephalic vein (G11 1.42, 8.3D, 8.5A-B, 8.22; G12 1.42, 8.5F, 8.9C, 8.12; N70, 74, 200, 205). The internal jugular vein has already been studied. The subclavian vein usually receives only one tributary, the external jugular vein. Other veins corresponding to arteries in the region drain into different vessels. The large vertebral vein descends anterior to the vertebral artery and may obscure its view (N 167 (no image)). The vertebral vein is a tributary of the brachiocephalic vein.
The thoracic duct drains into the junction of the left internal jugular and subclavian veins (left venous angle) (G11 1.71, 8.21, 8.22, 8.23; G12 1.73, 8.16A, 8.17B-C; N232, 233, 295). The thoracic duct carries lymph from the entire body below the diaphragm and the left half of the thorax. It typically receives the left jugular trunk carrying lymph from the left half of the head and neck and the left subclavian trunk carrying lymph from the left upper extremity (G11 1.71; G12 1.73). In addition, the thoracic duct may receive the left bronchomediastinal trunk carrying lymph from the upper lobe of the left lung and part of the lower lobe. On the right side, the right lymphatic duct is typically formed by the confluence of the right jugular, subclavian, and bronchomediastinal lymph trunks. The right bronchomediastinal trunk carries lymph from the right lung and the inferior lobe of the left lung (G11 1.38; G12 1.38; N202).
The vagus nerve (CN X) was seen earlier descending within the carotid sheath behind and between the carotid artery and internal jugular vein (G11 8.16C & E, 8.20, 8.21, 8.28A-B; G12 8.13A, 8.15A, 8.16A, 8.17A, 8.23A-B; N31, 71, 74, 75). It continues inferiorly in front of the first part of the subclavian artery and into the thorax. During the thoracic dissection the left recurrent laryngeal nerve was seen branching from the left vagus nerve beside the ligamentum arteriosum and passing posteriorly under the arch of the aorta (G11 1.43, 1.59, 1.61, 1.63; G12 1.43, 1.62, 1.64A, 1.65; N125, 206, 226, 234). It was later seen ascending within the upper part of the tracheoesophageal groove, where its close relationship to the inferior thyroid artery was noted.
The right recurrent laryngeal nerve normally recurs around the first part of the right subclavian artery and, therefore, is shorter than the left. Its longer course is why the left recurrent laryngeal nerve is more likely than the right to be involved in disease processes, such as bronchogenic carcinoma or an aortic arch aneurysm, producing left vocal cord palsy and hoarseness. A less common paralysis of the right vocal cord, as demonstrated at laryngoscopy, warrants examination of the apex of the right lung for a Pancoast tumor.
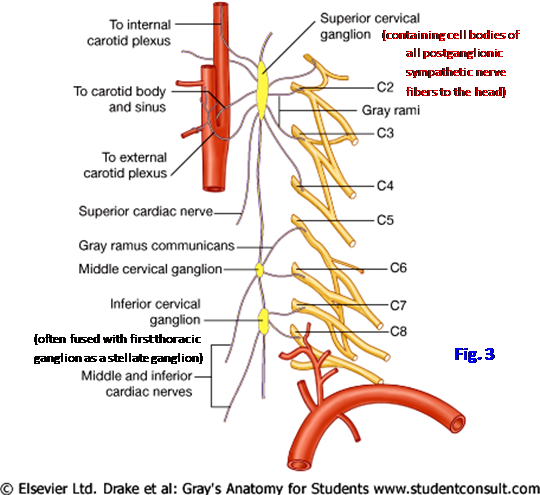
The cervical portion of the sympathetic trunk can be exposed at this point, and a basic understanding of its organization is helpful (Fig. 3; G11 Table 8.6; G12 Table 8.6A [p. 774]; N71, 129, 160). The cervical sympathetic trunk consists mainly of ascending preganglionic sympathetic fibers from upper thoracic spinal cord levels. It is located posterior to the carotid sheath in the prevertebral fascia covering the longus colli and longus capitis muscles. The cervical sympathetic trunk usually has three ganglia formed by the fusion of 8 ganglionic primordia of the embryo. Each cervical sympathetic ganglion contains the cell bodies of postganglionic sympathetic neurons. The large superior cervical sympathetic ganglion is formed by the fusion of primordia 1-4 and sends gray communicating rami carrying postganglionic sympathetic fibers to spinal nerves C1-4 (N129). The superior cervical sympathetic ganglion contains the cell bodies of ALL postganglionic sympathetic neurons to the head, which are distributed mainly along the external and internal carotid arteries and their branches.
The middle cervical sympathetic ganglion is formed by ganglionic primordia 5-6, usually at the level of the cricoid cartilage. It sends gray communicating rami to spinal nerves C5-6. The middle cervical sympathetic ganglion is the most variable of the cervical sympathetic ganglia and may be double or absent on a side.
The inferior cervical sympathetic ganglion sends gray communicating rami to spinal nerves C7-8. In addition to their connection by the cervical sympathetic trunk, the middle and inferior ganglia are connected by a loop around the subclavian artery, the ansa subclavia (G11 8.24, Table 8.6; G12 Table 8.6A [p. 774]; N129, 220). Approximately 80% of the time the inferior cervical ganglion is fused with the first thoracic ganglion to form a large stellate (cervicothoracic) ganglion anterior to the neck of the first rib.
The stellate ganglion may be invaded by a Pancoast tumor of the apex of the lung (e.g., see http://emedicine.medscape.com/article/428469-overview#showall ). Local anesthetic may be injected to block the stellate ganglion in some pain syndromes (e.g., complex regional pain syndrome [reflex sympathetic dystrophy]) and in vascular insufficiency of the upper extremity (e.g., Raynaud’s syndrome). Anesthesia or pathological damage to the ganglion results in Horner syndrome characterized by an ipsilateral drooping eyelid (ptosis), constricted pupil (miosis), vasodilation (facial flushing and warmth), and absence of sweating (anhidrosis).
9. Clean the junction of the left internal jugular and subclavian veins (left venous angle). Verify that the only tributary of the subclavian vein is the external jugular vein in the posterior cervical triangle. Find the thoracic duct arching superolaterally from behind the carotid sheath to enter the left venous angle. The thoracic duct may be pale or may contain dried blood and have a bluish tinge, but unlike most veins, it typically has scalloped margins. Briefly look for the right lymphatic duct entering the right venous angle.
10. Find the right vagus nerve crossing anterior to the first part of the subclavian artery and identify its recurrent laryngeal branch. Trace the right recurrent laryngeal nerve under the subclavian artery and superiorly within the tracheoesophageal groove to near the cricoid cartilage. If not previously done, find the left recurrent laryngeal nerve within the tracheoesophageal groove. Again note the close relationship of each recurrent laryngeal nerve to the inferior thyroid artery of its side.
11. Bluntly dissect through the prevertebral fascia in a longitudinal direction posterior, and slightly medial to, the common carotid artery. Find the cervical sympathetic trunk, which appears as a slender strand of nerve, or sometimes as two strands, joining sympathetic ganglia. At the level of the cricoid cartilage, look for the middle cervical sympathetic ganglion. It may be absent or there may be two small ganglia. The stellate (cervicothoracic) ganglion may be difficult to see anterior to the neck of the first rib when looking from above. If so, once again remove a lung from the thoracic cavity so that you can follow the thoracic sympathetic trunk superiorly to the ganglion, which may be as large as the distal 2/3 of a little finger. Replace the lung in the pulmonary cavity and notice the proximity of the lung apex to the stellate ganglion, which is important if a Pancoast tumor is present. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.