Face and Scalp
ORGANIZATION OF THE HEAD AND SUPERFICIAL FACE
Study the osteology of the anterior part of the skull. The head is organized around a series of functional spaces (Fig. 1), and this organization is reflected in the structure of the skull. The orbits are concerned with vision. They contain the eyeballs and optic nerves, extraocular muscles that move the eyes, and associated nerves and blood vessels.
The nasal cavities (viewed through the piriform aperture in the prepared skull) are the uppermost parts of the respiratory system. They are separated by the nasal septum and have scroll-like projections of bone (nasal conchae) in their lateral walls. The lining nasal mucosa consists of a large respiratory portion that warms and humidifies air and traps particulate matter. Its surface area is increased by the presence of the nasal conchae. A small superior olfactory portion of the nasal mucosa contains sensory receptors for the sense of smell (olfaction).
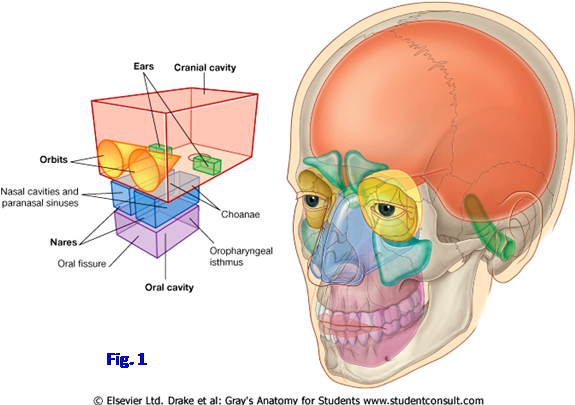
The oral cavity is inferior to the nasal cavities and separated from them by the palate. The oral cavity proper is part of the mouth and is defined in the skull by the hard palate and maxillary alveolar arch and teeth above. The floor of the oral cavity consists entirely of soft tissues, but the inferior portion of this functional space is roughly outlined on the skull by the mandibular alveolar arch and teeth.
The cranial cavity and the middle and inner ears are the other major functional spaces. The cranial cavity contains the brain and its blood supply, the meninges, and cerebrospinal fluid. The ear is the organ of hearing, and the inner ear is involved also in sensing the position of the body in space and maintaining equilibrium. The cranial cavity and ear will be studied later.
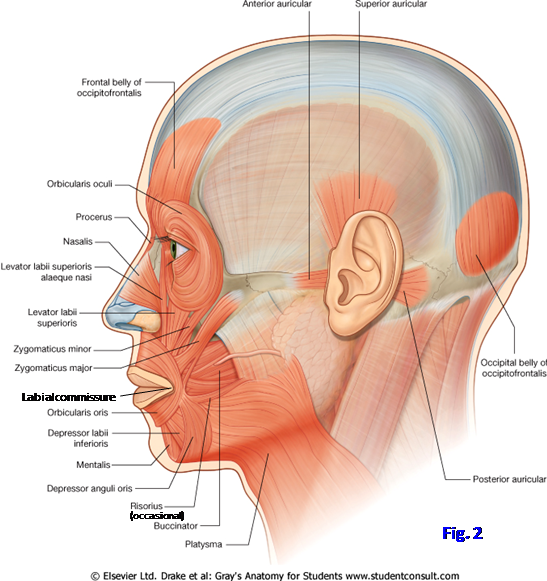
The muscles of facial expression are unusual in that they are subcutaneous voluntary muscles (i.e., subcutaneous skeletal muscles). In general they arise from bone or fascia and insert into skin. In addition to their function in communication (facial expressions), they constrict or dilate the orifices of the face—the palpebral fissures (between the eyelids), nares or nostrils (openings into the vestibules of the nasal cavities), and oral fissure (between the lips). The muscles of facial expression all develop from the second pharyngeal arch of the embryo and are innervated by the nerve of that arch, the facial nerve (CN VII).
Before considering the muscles of facial expression, some descriptive terms of the face need to be defined. The upper lip consists not just of the red transitional zone bordering the oral fissure, but rather the entire region between the oral fissure and the nose. It is separated from the cheeks laterally by the nasolabial grooves descending from the alae (wings) of the nose to pass some distance lateral to the oral fissure. The midline vertical groove in the upper lip is the philtrum. The lower lip is separated from the chin by the almost horizontal labiomental groove, which deepens with age. The upper and lower lips are connected to each other at the corners (angles) of the mouth by the thin, fragile labial commissures.
The muscles of facial expression can be grouped according to the orifice with which they are associated (Fig. 2; G11 7.7, 7.9, Table 7.1 [p. 603]; G12 7.12, 7.14, Table 7.1 [p. 629]; N 25, 54, 122). We will consider only the major ones, and even those often are thin and pale in the cadaver, making them difficult to demonstrate in dissection. Muscles of the oral fissure and mouth include the orbicularis oris forming the substance of the lips. It has a complex structure with intrinsic muscle fibers and contributions from surrounding muscles, such as the buccinator, levator anguli oris, and depressor anguli oris.
Ascending to the angle of the mouth from near the lower border of the mandible is the triangular depressor anguli oris muscle (G11 7.7, 7.8; G12 7.12, 7.13; N25, 54). The depressor labii inferioris arises from the lower mandible partly deep to depressor anguli oris and ascends medial to it toward the orbicularis oris. Fibers from the platysma muscle blend with both of these muscles (G11 Tables 7.1 [p. 603], 8.1 [p. 722]; G12 Tables 7.1 [p. 629], 8.1 [p. 746]; N25). Although usually described with the facial muscles, the risorius muscle approaching the angle of the mouth from laterally is frequently absent. The mentalis, which allows us to protrude the lower lip in pouting when someone else just ate the last chocolate chip cookie, arises from the mandible just below the incisor teeth and descends to the skin of the chin.
Converging on the orbicularis oris from above are, from lateral to medial, the zygomaticus major, zygomaticus minor, levator labii superioris, and levator labii superioris alaque nasi muscles. The zygomaticus major arises from the zygomatic bone near the prominence of the cheek and descends medially to the angle of the mouth (G11 7.7, 7.8, 7.10; G12 7.12, 7.13, 7.15; N25, 54). The zygomaticus minor courses inferomedially parallel to the zygomaticus major to near the angle of the mouth. The zygomaticus major and minor muscles may be fused, or the minor may be absent.
The levator labii superioris takes origin from the maxilla just above the infraorbital foramen and descends slightly medially to the orbicularis oris of the upper lip (G12 7.12, 7.15A). The levator labii superioris alaque nasi arises from the frontal process of the maxilla and descends on the medial side of the levator labii superioris. Some of its fibers attach to the greater alar cartilage of the nose with its more lateral fibers continuing into the upper lip. Running at nearly a right angle to these two muscles and deep to them is the levator anguli oris (G11 7.10, Table 7.1 [p. 603]; G12 7.15, Table 7.1 [p. 629]; N54). It arises from the canine fossa of the maxilla inferior to the infraorbital foramen and descends to the angle of the mouth.
The buccinator muscle is the muscle of the cheek, occupying the space between the maxilla and mandible (G11 7.7, 7.45, 7.47; G12 7.12, 7.41A, 7.42; N25, 54, 55, 60). It arises from the maxilla and mandible opposite the molar teeth and from the pterygomandibular raphe, a fibrous junction between the buccinator and the superior pharyngeal constrictor muscle (G11 8.30A, 8.32F, Table 8.7 [p. 766]; G12 8.23C, 8.25A, 8.27F, Table 8.9 [p. 788]; N55, 68). The buccinator contributes muscle fibers, some crossed, to the orbicularis oris in both the upper and lower lips. It helps to hold food between the teeth during chewing (mastication) and forcefully expels air in buglers and trumpet players. To clarify a point of frequent confusion, the buccinator muscle is a muscle of facial expression and, therefore, is innervated by the facial nerve, not by the buccal branch of the mandibular nerve (V3), which pierces the muscle to supply sensory innervation to the buccal mucosa. If the buccinator muscle is paralyzed due to a facial nerve lesion, as in Bell’s palsy or following parotid gland surgery, the buccal mucosa may slip between the teeth during chewing and be repeatedly lacerated.
The largest and best developed of the muscles of the nasal group is the nasalis. It consists of a thin transverse part (compressor naris), which arises from the maxilla and meets the muscle of the opposite side on the dorsal midline of the nose, and an alar part (dilator naris), which ascends from the maxilla to the greater alar cartilage (N35). The alar part draws the alar cartilage inferiorly and laterally, dilating the nostril. The function of the transverse part of the nasalis is probably compression but is controversial.
The main orbital muscle of facial expression is the orbicularis oculi (G11 7.7, 7.9A, Table 7.1 [p. 603]; G12 7.12, 7.14A, Table 7.1 [p. 629]; N25). It has three parts, of which we will study the larger two. The orbital part forms concentric rings that overlie the bony margin of the orbit. It closes the eyelids forcefully, as in protecting the eye against a sudden exposure to bright light or the entry of a foreign object. The palpebral part is in the eyelids and closes them gently, as during blinking. Paralysis of the orbicularis oculi eliminates blinking to spread lacrimal fluid across the cornea and visible sclera and will result in drying and ulceration of the cornea if protective steps aren’t taken.
Two other muscles in the orbital region, but not concerned with closing the eyelids, are the procerus and the corrugator supercilii (G11 7.7, 7.10; G12 7.12, 7.15; N25, 35). The procerus lies over the root of the nose. It takes origin from the nasal bones and upper part of the lateral nasal cartilages and ascends to the skin between the eyebrows. The procerus produces horizontal wrinkles over the root of the nose. The corrugator supercilii lies deep to the eyebrow. It takes origin from the medial end of the superciliary arch and ascends laterally to insert into the skin near the middle of the eyebrow. The corrugator supercilii produces vertical wrinkles above the nose.
The occipitofrontalis (epicranius) is a muscle of facial expression largely located within the scalp (N25). It consists of frontal (frontalis) and occipital (occipitalis) bellies joined by an aponeurotic tendon (epicranial aponeurosis or galea aponeurotica). The frontalis blends inferiorly with the orbicularis oculi and into the skin of the eyebrows and root of the nose. It elevates the eyebrows and wrinkles the skin of the forehead.
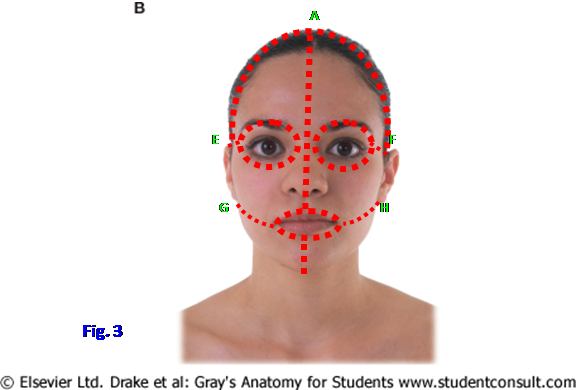
1. In order to demonstrate the muscles of facial expression, it is important to make SHALLOW INCISIONS THROUGH SKIN ONLY! Make a vertical midline incision through skin from the vertex of the skull down the forehead, along the dorsum of the nose, and through the upper lip to the oral fissure (Fig. 3, A⇒B). Make a second midline incision from the oral fissure through the skin of the lower lip and chin (C⇒D). From the initial midline incision make incisions laterally around the orbital margin on each side from the root of the nose to the top of the auricles (i.e., to E and F). Make incisions laterally from the midline at B and C around the red transition zone of the upper and lower lips, respectively, to the angles of the mouth and continuing to the bottom of the auricles (i.e., to G and H). Make coronal incisions from the beginning of the original midline incision at the vertex of the skull to the top of the auricles (A⇒E and A⇒F). Remove the flaps of skin freed by these incisions CAREFULLY because the subcutaneous facial muscles insert into the dermis—if done correctly, you should see a pitted, orange peel appearance on the deep surface of the removed skin.
2. Clean as many of the muscles of facial expression as you can identify on your cadaver. Be sure and study the facial muscles on other cadavers, which may have better examples of some muscles. Clean the oval fibers of the orbicularis oris within the upper and lower lips. Dissect the triangular depressor anguli oris ascending to the corner of the mouth. Just medial to the depressor anguli oris and emerging from deep to it find the depressor labii inferioris. Note that fibers of the platysma blend with these muscles. Do not spend time looking for the mentalis, which is often difficult to demonstrate, but be aware of its arrangement.
3. Clean the zygomaticus major muscle descending medially from the prominence of the cheek to the corner of the mouth. Look for the zygomaticus minor, which may be fused with the major or may be absent. Clean the levator labii superioris descending to the orbicularis oris from just below the infraorbital margin. Find the levator labii superioris alaeque nasi descending from the frontal process of the maxilla in the angle between the nose and cheek. Next, look for the levator anguli oris descending laterally to the angle of the mouth from deep to the levator labii superioris.
4. Clean the anterior portion of the buccinator muscle. Part of the buccinator is deep to the ramus of the mandible, and part is hidden by the buccal fat pad, which may have largely disappeared in an emaciated individual. The duct of the parotid gland (parotid duct) pierces the muscle.
5. Look for the thin transverse part of the nasalis. Be aware of the major features of the cartilages of the external nose (G11 7.62A-D; G12 7.57A-D; N35), but don’t spend time on them now. They will be studied later.
6. Carefully remove the thin skin of the eyelids. Clean the orbital and palpebral parts of the orbicularis oculi. Find the procerus between the two orbicularis oculi muscles at the root of the nose. Clean the frontalis muscle in the forehead. Do not look for corrugator supercilii. XXX
The facial artery was seen branching from the external carotid artery and traversing the submandibular triangle deep to the submandibular gland to reach the lower border of the mandible just anterior to the masseter muscle. The artery continues up the face lateral to the angle of the mouth and beside the nose to the medial angle of the eye (G11 7.7, 7.8, 7.43A, 8.6, Table 7.3 [p. 606]; G12 7.12, 7.13, [p. 662A], Tables 7.3 [p. 632], 8.5 [p. 765]; N3, 35, 69). It becomes the angular artery after it gives off its lateral nasal branch. Unlike most arteries, the facial artery takes a tortuous course, presumably to accommodate chewing and swallowing movements.
Major branches of the facial artery include the inferior and superior labial arteries and the lateral nasal artery. The angular artery anastomoses with the dorsal nasal artery, a branch of the ophthalmic artery from the internal carotid, near the medial angle of the eye (N69, 85). This anastomotic connection is potentially important if the internal carotid artery becomes slowly occluded by atherosclerosis.
The facial vein descends on the face just lateral to the artery (G11 7.7, 7.16A, 8.4A, Table 7.4 [p. 607]; G12 7.12, 7.21, 8.2A, Table 7.4 [p. 633]; N3, 70). It begins as the angular vein by the confluence of the supratrochlear and supraorbital veins and receives tributaries corresponding to branches of the facial artery. Crossing superficial to the submandibular gland, the facial vein is joined by the anterior branch of the retromandibular vein to form the common facial vein. The facial vein is clinically important because facial vein thrombophlebitis secondary to an infection of the middle third of the face (danger area) may result in the potentially fatal spread of infectious agents to the cavernous sinus with clot formation (cavernous sinus thrombosis) and the development of meningitis. The cavernous sinus is a dural venous sinus at the base of the brain and is connected by emissary veins with the angular vein and with the pterygoid venous plexus within the infratemporal fossa, which is located deep to the ramus of the mandible (N70, 85, 103) (see http://emedicine.medscape.com/article/791704-overview#showall ). Although a relatively uncommon condition, diagnosis of cavernous sinus thrombosis is important because the mortality rate without early treatment is close to 100%.
7. Identify and clean the facial artery and facial vein. Find the origins of the superior labial and inferior labial branches of the facial artery to the upper and lower lips, respectively. Identify the lateral nasal artery branching beside the external nose. Follow the facial artery and vein to where they are continuous with the angular artery and vein above the origin of the lateral nasal branch. XXX
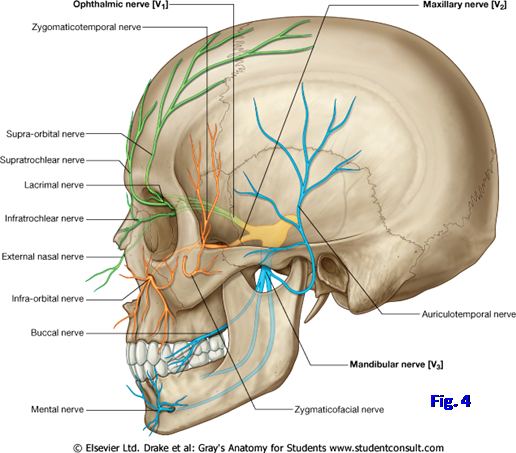
The trigeminal nerve (CN V) is the main sensory nerve of the face (Fig. 4; G11 7.10, Table 7.2 [p. 605]; G12 7.15, Table 7.2 [p. 631]; N2, 121). Its three divisions—ophthalmic, maxillary, and mandibular—are named according to their principal area of termination. Only the mandibular division of the trigeminal nerve contains motor fibers, which innervate the muscles that developed from the first pharyngeal arch of the embryo.
The ophthalmic division of the trigeminal nerve (V1) supplies skin of the dorsum of the nose and the forehead (Fig. 4; N2, 44). It gives infratrochlear and external nasal branches to the nose and supratrochlear and supraorbital branches to the forehead. The small lacrimal branch of the ophthalmic division supplies the lateral part of the upper eyelid. A herpes zoster viral infection may involve the ophthalmic division of V with the eruption of vesicles along its course. This herpes zoster ophthalmicus may produce painful ulceration and scarring of the cornea.
The maxillary division (V2) supplies cutaneous innervation to the middle third of the face and anterior temple (Fig. 4; N2, 44). The infraorbital nerve exits the infraorbital foramen deep to the levator labii superioris to distribute to the middle face. The zygomaticofacial nerve supplies a small area over the zygomatic bone. The zygomaticotemporal nerve supplies skin over the anterior temple.
The mandibular division of the trigeminal nerve (V3) supplies cutaneous innervation to the skin of the chin and lower lip through its mental branch (N2, 45, 71). The mental nerve emerges onto the face via the mental foramen inferior to the second mandibular premolar tooth, deep to the depressor anguli oris. The buccal branch of the mandibular nerve passes from the infratemporal fossa into the cheek deep to the ramus of the mandible. It pierces the buccinator muscle but is a sensory nerve. The auriculotemporal nerve leaves the infratemporal fossa posterior to the neck of the mandible. It supplies skin anterior to the upper part of the auricle and in the temporal region, as well as the anterior superior part of the auricle itself. The mandibular nerve will be studied in more detail during the infratemporal fossa dissection.
8. Preserve the facial artery and vein while cleaning the major cutaneous branches of the trigeminal nerve. Notice that the supraorbital (V1), infraorbital (V2), and mental (V3) nerves emerge onto the face in a more or less vertical line. The supraorbital notch often can be palpated by running your fingertip along the supraorbital margin. Even if the notch is bridged over by bone to form a foramen, there often is a shallow indentation to indicate the location. Find the supraorbital nerve and artery ascending into the forehead from the supraorbital notch. Look just medial and slightly inferior to the supraorbital nerve, at the medial end of the supraorbital margin, for the supratrochlear nerve and artery.
9. The infraorbital foramen is deep to the levator labii superioris. The depression at the opening of the foramen can often be palpated through the muscle. Probe deep to the levator labii superioris or make a short (1 cm) cut through it on one side of the face to expose the infraorbital nerve and artery.
10. The mental foramen is hidden by the depressor anguli oris. Reflect the muscle on one side of the face or make a short (1 cm) incision through it to expose the mental nerve and artery. In an edentulous cadaver, the alveolar process of the mandible usually will have been resorbed, and the mental foramen may be situated on the superior border of the body of the mandible. Be aware of the distribution of the other cutaneous branches of the trigeminal nerve, but don’t attempt to find them at this time. XXX
The superficial part of the parotid gland is located on the side of the face, just anterior and inferior to the auricle (G11 7.7, 7.8, 7.43; G12 7.12, 7.13, [p. 662A-B]; N24, 25). It overlies the posterior part of the masseter muscle and the ramus of the mandible. The parotid gland is the largest of the three major salivary glands—parotid, submandibular, and sublingual. It is partly wrapped around the posterior border of the mandibular ramus and is enclosed within parotid fascia, which is formed by a split in the investing layer of deep cervical fascia. The tough parotid fascia and the gland’s location between the ramus of the mandible and the mastoid process of the temporal bone, where it is compressed during chewing, causes pain when the gland is inflamed (parotiditis, parotitis), usually as a result of infection (e.g., mumps). Severely ill patients who become dehydrated may develop acute bacterial parotiditis, which is often fatal (80%) without antibiotic treatment (e.g., see http://emedicine.medscape.com/article/882461-overview#showall ).
The parotid duct leaves the anterior aspect of the gland and passes forward across the masseter muscle and buccal fat pad to the buccinator muscle (G11 7.7, 7.8; G12 7.12, 7.13; N24, 61), which it pierces opposite the second maxillary molar tooth. The site is indicated on the inside of the cheek by a mucosal fold, the parotid papilla, which most of us have bitten and irritated at one time or another.
Several major structures traverse the parotid gland. They are, from superficial to deep, the facial nerve, the retromandibular vein and its tributaries, and the external carotid artery and its terminal branches. The facial nerve (CN VII) exits the stylomastoid foramen in the base of the skull and passes forward into the substance of the parotid gland. It typically divides into temporofacial and cervicofacial divisions (Fig. 5; G11 7.8, 7.43A-B; G12 7.13, [p. 662A-B]; N24, 61, 122). Both contribute buccal branches. The temporofacial division also gives temporal and zygomatic branches to the upper muscles of facial expression. The cervicofacial division also gives marginal mandibular and cervical branches to the lower muscles of facial expression. One of the more socially acceptable pneumonics to remember the five major branches of the facial nerve to the muscles of facial expression is: The Zoo Borrowed My Crocodile. The facial nerve may be injured by infectious agents, during parotid gland surgery, or idiopathically (Bell’s palsy) with paralysis of the muscles of facial expression on that side and other consequences. For a discussion of Bell’s palsy, see http://emedicine.medscape.com/article/1146903-overview#showall
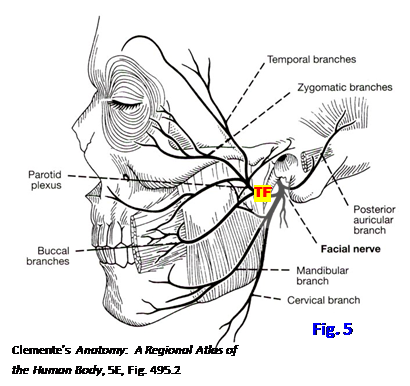
11. Remove the parotid fascia to expose the parotid gland. Find the thick parotid duct passing forward from the gland parallel to the zygomatic arch to pierce the buccinator muscle. Clean the stem and branches of the facial nerve (Fig. 5). This can be done either by finding the branches emerging from the parotid gland and tracing them posteriorly or by finding the stem of the nerve exiting the stylomastoid foramen medial to the mastoid process of the temporal bone and tracing it anteriorly. Perhaps the two easiest branches to find are the zygomatic branch coursing toward the lateral angle of the eye and the marginal mandibular branch coursing just above or below the inferior border of the mandible. Dissect the temporal, zygomatic, and buccal branches of the facial nerve. Clean the marginal mandibular and cervical branches. The parotid gland will have to be picked away piecemeal to clean the facial nerve. XXX
The retromandibular vein is formed behind the neck of the mandible by the union of the superficial temporal and maxillary veins (G11 8.4A, Table 7.4 [p. 607]; G12 8.2A, Table 7.4 [p. 633]; N 70). It descends through the parotid gland medial to the facial nerve and divides near the angle of the mandible into anterior and posterior branches (divisions). The anterior branch of the retromandibular vein joins the facial vein to form the common facial vein, which usually drains into the internal jugular vein. The posterior branch of the retromandibular vein is joined by the posterior auricular vein to form the external jugular vein, which was previously seen descending vertically across the sternocleidomastoid muscle.
The external carotid artery ascends through the parotid gland deep to the retromandibular vein. Posterior to the neck of the mandible it divides into its terminal branches, the superficial temporal artery and maxillary artery (G11 7.7, 7.8, 7.43, 7.47, 7.48A, Table 7.3 [p. 606]; G12 7.12, 7.13, [p. 662A-B], 7.42, 7.43A, Table 7.3 [p. 632]; N3, 39, 69). The superficial temporal artery ascends anterior to the upper part of the auricle and divides into anterior and posterior branches to supply the scalp of the temple region. It gives off the transverse facial artery just below the zygomatic arch. The transverse facial artery usually passes forward parallel to, and between, the zygomatic arch and the parotid duct. The maxillary artery passes deep to the ramus of the mandible into the infratemporal fossa and will be studied during the next period.
The auriculotemporal nerve (V3) leaves the infratemporal fossa behind the neck of the mandible and ascends through the upper part of the parotid gland (G11 7.7, 7.8, Table 7.2 [p. 605]; G12 7.12, 7.13, Table 7.2 [p. 631]; N2, 45, 71). It continues across the zygomatic arch with the superficial temporal vessels and provides cutaneous sensation to the temple. Typically the slender auriculotemporal nerve can be found just posterior and deep to the superficial temporal vessels.
12. Clean the superficial temporal artery and vein as they ascend over the zygomatic arch and anterior to the upper part of the auricle. Find the slender auriculotemporal nerve just posterior and deep to these vessels. Attempt to trace the retromandibular vein and external carotid artery through the parotid gland. This may be easier to do following removal of the upper half of the ramus of the mandible in a later lab period. XXX
The scalp is the part of the head above the face, covering the calvaria (skullcap). We are going to study the scalp before reflecting it. During the next lab period we will remove the calvaria and associated meninges, remove the brain, and study features of the cranial base, notably the dural venous sinuses and cranial nerves.
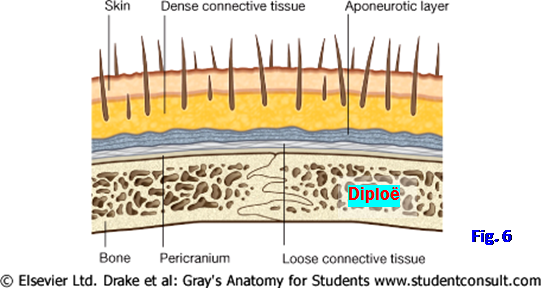
The scalp extends from the superciliary arches on the frontal bone to the external occipital protuberance and superior nuchal lines on the occipital bone. It is a five-layered structure covered with a variable amount of hair (Fig. 6; G11 7.11A; G12 7.16A; N101). The five layers are easily remembered by the letter-word association: S – Skin C – dense Connective tissue A – Aponeurotic layer L – Loose connective tissue P – Pericranium.
The skin of the scalp is unremarkable, but the presence of too much hair in middle-aged males may detract from its appearance (see Dr. Roque). Skin is anchored to the aponeurotic layer by dense connective tissue. The dense connective tissue contains the arteries, veins, and nerves of the scalp. The aponeurotic layer is actually a musculoaponeurotic layer consisting of the frontalis muscle in the forehead and the occipitalis muscle in the occiput joined by the strong, broad epicranial aponeurosis (galea aponeurotica) (G11 7.11B; G12 7.16B; N25). The frontalis and occipitalis are muscles of facial expression innervated by the facial nerve (CN VII).
In a scalp laceration, the dense connective tissue of the second layer holds blood vessels open, resulting in profuse, and potentially fatal, bleeding. Since arteries of the scalp ascend into it, hemorrhage can often be controlled in an emergency by tying a tie, shoelaces, etc., around the head just above the eyebrows and ears. The superficial three layers—skin, dense connective tissue, and the aponeurotic layer—are tightly bound together and separate from the deeper layers as a unit during surgery and in a scalping injury. Necrosis of calvarial bone doesn’t typically occur in scalping injuries because the main blood supply to the bone is from the middle meningeal arteries.
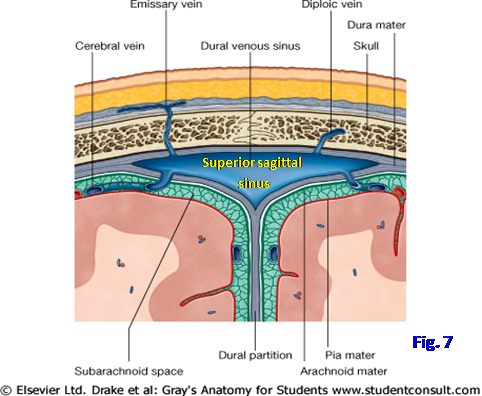
The loose connective tissue layer of the scalp facilitates movement of the scalp over the calvaria. Unfortunately, it also provides a pathway for the spread of infections through the scalp. An infection in this layer may spread through emissary veins to dural venous sinuses within the cranial cavity (e.g., the superior sagittal sinus) (Fig. 7) with potentially fatal consequences. Blood in the loose connective tissue layer can enter the eyelids, producing “black eyes,” because the frontalis muscle inserts into skin and dense subcutaneous connective tissue rather than into bone.
“Pericranium” is the name given to the periosteum on the external surface of the calvaria. It is continuous with the fibrous connective tissue of sutures and is firmly adherent to them.
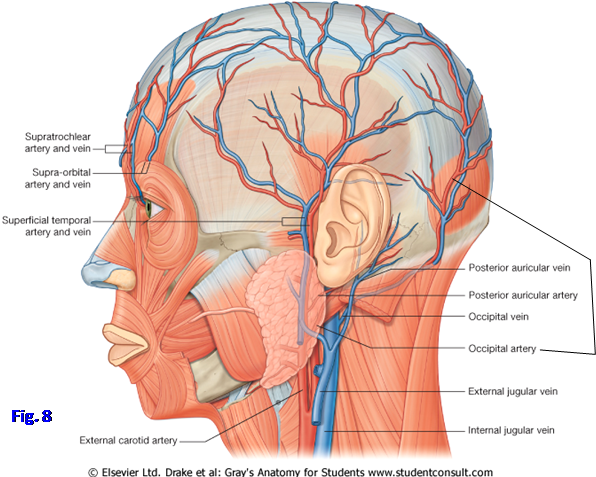
The rich blood supply of the scalp is derived from branches ascending into it from both the internal and external carotid arteries. The branches anastomose and this contributes to the profuse bleeding from scalp wounds. The ophthalmic branch of the internal carotid artery gives supraorbital and supratrochlear arteries that leave the orbit to ascend into the forehead (Fig. 8; G11 Table 7.3 [p. 606]; G12 Table 7.3 [p. 632]; N3, 69). They supply the anterior and superior parts of the scalp to near the vertex.
The three major branches of the external carotid artery that supply blood to the scalp are the superficial temporal artery, posterior auricular artery, and occipital artery (Fig. 8; N3, 69). The superficial temporal artery has already been seen branching from the external carotid artery and ascending anterior to the auricle with the superficial temporal vein and auriculotemporal nerve. The posterior auricular artery is a small posterior branch of the external carotid that arises just below the auricle and ascends behind it. The posterior auricular artery supplies the scalp posterior to the external ear. The occipital artery may have been seen branching from the external carotid in the carotid triangle. Its termination was cleaned during the back dissection as the artery ascended medially on the back of the scalp to run with the greater occipital nerve (G11 4.28; G12 4.31, 4.38; N172).
The veins of the scalp accompany the arteries (Fig. 8; G11 Table 7.4 [p. 607]; G12 Table 7.4 [p. 633]; N3, 70). In addition to draining the scalp, they drain calvarial diploic veins that course between the internal and external tables of compact bone (Fig. 7; G11 7.11D; G12 7.16D; N99, 101). Emissary veins connecting scalp veins with dural venous sinuses provide a route for the intracranial spread of infection.
The sensory innervation of the scalp is from the trigeminal nerve (CN V) and branches of cervical spinal nerves (G11 Table 7.2 [p. 605]; G12 Table 7.2 [p. 631]; N2, 35, 71, 171).
All three divisions of the trigeminal nerve contribute to innervation of the scalp anterior to a coronal plane at the level of the auricles. The supraorbital and supratrochlear nerves from the ophthalmic division (V1) ascend from the orbit into the forehead and continue superiorly across the scalp (Fig. 4). The zygomaticotemporal nerve from the maxillary division (V2) exits the zygomaticotemporal foramen to supply the anterior part of the temple. The auriculotemporal nerve from the mandibular division (V3) has already been seen emerging from the infratemporal fossa behind the neck of the mandible and ascending anterior to the auricle to enter the scalp.
The innervation of the scalp posterior to the auricles is mainly from the lesser occipital and greater occipital nerves (G11 4.28, 8.3A; G12 4.31, 8.5; N2, 171). The lesser occipital nerve is a branch of the cervical plexus that contains nerve fibers from the anterior ramus of C2. It supplies the scalp behind the ear. The greater occipital nerve is a branch of the posterior ramus of C2. During the suboccipital triangle dissection the greater occipital nerve was traced from below the obliquus capitis inferior muscle through the semispinalis capitis and through, or just lateral to, the trapezius into the posterior scalp (G11 4.28, 4.35, 4.36; G12 4.31, 4.38, 4.39; N172). It innervates most of the scalp posterior to the vertex.

REFLECTION OF THE SCALP
13. Place a block under the neck to elevate the head from the table. To reflect the scalp and expose the calvaria, MAKE TWO INCISIONS AT A RIGHT ANGLE DOWN TO BONE as follows (Fig. 9): (1) Make a midsagittal incision from between the eyebrows near nasion to the external occipital protuberance (A⇒B). (2) Make a coronal incision across the vertex of the skull from ear to ear (C⇒D).
14. Separate the scalp from the skull deep to the aponeurotic layer, along the loose connective tissue layer, and reflect the four flaps downward. Clean any remaining tissue from the exposed calvaria. To do this, it will be necessary to scrape the temporalis muscle downward to near the level of the zygomatic arch.
15. Before spraying and covering the body, fold the four flaps of scalp back up over the calvaria. It will be studied during the next lab. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.