Temporal and Infratemporal Regions
Review the osteology of the lateral aspect of the skull (Fig. 1; N6). The zygomatic arch is formed by the temporal process of the zygomatic bone and the zygomatic process of the temporal bone. The shallow depression in the cranial vault superior to the zygomatic arch is the temporal fossa. It is bounded superiorly by the superior temporal line, which continues posteriorly and superiorly from the zygomatic process of the frontal bone. The floor of the temporal fossa is formed by the squamous part of the temporal bone, parietal bone, frontal bone, and the greater wing of the sphenoid bone. These bones meet at a somewhat “H”-shaped junction, the pterion. The pterion marks a site where the bone is relatively thin and where the middle meningeal artery usually occupies a deep groove, if not an actual canal, on the internal surface of the cranial vault. A blow to the region of the pterion may fracture the bone, tearing the middle meningeal artery to produce an epidural (extradural) hematoma. An epidural hematoma increases intracranial pressure and may be fatal within hours if untreated.
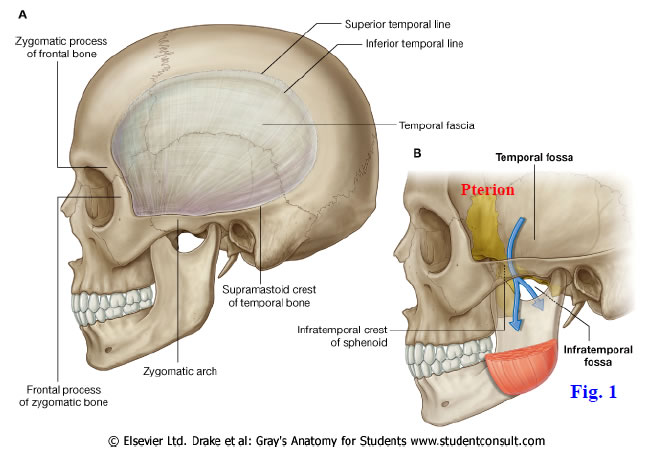
The infratemporal fossa is an irregular space inferior to the zygomatic arch and deep to the ramus of the mandible (Figs. 1, 2; Gr 7.44; N6). It communicates with the temporal fossa above through the space deep to the zygomatic arch. The lateral wall of the infratemporal fossa is formed by the ramus of the mandible, the medial wall by the lateral pterygoid plate, the anterior wall by the infratemporal surface of the maxilla, and the posterior wall by the tympanic plate and styloid process of the temporal bone. The roof of the infratemporal fossa is formed by the infratemporal surface of the greater wing of the sphenoid bone with its infratemporal crest designated as the actual boundary between the temporal and infratemporal fossae.
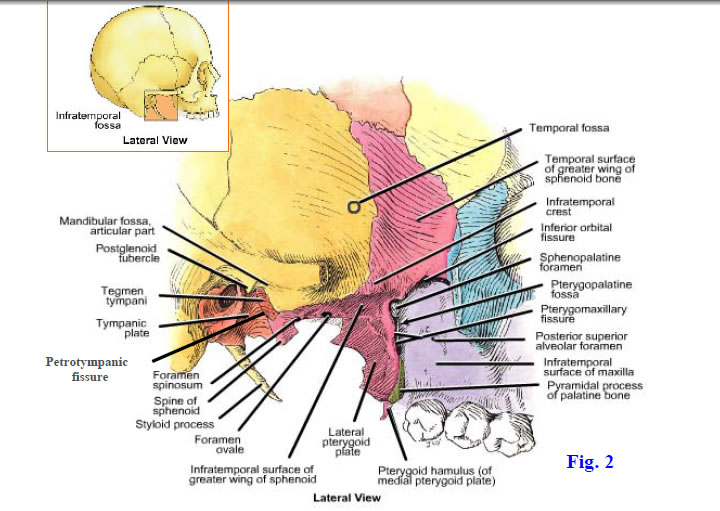
The infratemporal fossa communicates with a number of other spaces, and understanding these relationships is one of the keys to understanding the anatomy of the head. Superiorly, the foramen ovale and foramen spinosum pierce the greater wing of the sphenoid bone to connect the middle cranial fossa (of the cranial cavity) and the infratemporal fossa (Fig. 2). Anterosuperiorly, the inferior orbital fissure connects the infratemporal fossa with the orbit. Posterosuperiorly, the narrow petrotympanic fissure permits the chorda tympani nerve to enter the infratemporal fossa from the tympanic (middle ear) cavity. Medially, the pterygomaxillary fissure located between the pterygoid process of the sphenoid bone and the maxilla connects the infratemporal fossa with the small, but important, pterygopalatine fossa. The structures that traverse these communications will be studied during this dissection.
Superficial structures of the temporal region include the previously dissected temporal branches of the facial nerve, the auriculotemporal nerve, and the superficial temporal vessels (N2, 3, 24). The auriculotemporal nerve is a branch of the mandibular division of the trigeminal nerve (V3) that leaves the infratemporal fossa posterior to the neck of the mandible to ascend in front of the auricle into the temporal region. It is sensory to the superior part of the auricle and the scalp.
The superficial temporal artery is one of the two terminal branches of the external carotid artery (N3, 69). It ascends over the zygomatic arch in front of the auricle with the auriculotemporal nerve to divide into anterior (frontal) and posterior (parietal) branches. Over the zygomatic arch is an easy place to take a pulse from the superficial temporal artery, although some people are sensitive about having their faces touched. The transverse facial artery branches from the superficial temporal to travel anteriorly parallel to, and a finger’s width below, the zygomatic arch.
The superficial temporal vein accompanies the superficial temporal artery in front of the auricle (N3, 70). Behind the neck of the mandible, it joins the maxillary vein superficial to the external carotid artery to form the retromandibular vein.
1. The superficial temporal artery and vein were seen earlier in the fascia anterior to the auricle. Find them again, along with the small auriculotemporal nerve that usually runs just posterior and deep to these vessels. The retromandibular portions of these structures will be easier to study once part of the ramus of the mandible has been removed. XXX
The temporal and infratemporal fossae are considered part of the deep face. The main contents of these spaces are muscles of mastication, branches of the mandibular division of the trigeminal nerve (V3), branches of the maxillary artery, and the pterygoid plexus of veins. The maxillary artery is one of the terminal branches of the external carotid artery. The pterygoid venous plexus coalesces to form the maxillary vein(s).
The four major muscles of mastication, all developed from the first pharyngeal arch of the embryo, are the temporalis, masseter, lateral pterygoid, and medial pterygoid (N54, 55). They are innervated by the mandibular division of the trigeminal nerve (V3). All except the lateral pterygoid muscle elevate the mandible, closing the jaws. The fan-shaped temporalis muscle occupies most of the temporal fossa. It takes origin from bone of the temporal fossa and from the deep surface of the overlying temporal fascia, passes deep to the zygomatic arch, and inserts on the coronoid process and anterior border of the ramus of the mandible. In addition to closing the jaws, the horizontal posterior fibers of the temporalis are described as retracting the protruded mandible. The temporalis is innervated by the deep temporal nerves (V3), which enter the temporal fossa deep to the muscle (N45).
The ramus of the mandible is covered externally by the powerful masseter muscle (N54). The masseter attaches superiorly to the inferior border and medial surface of the zygomatic arch and inferiorly to the lateral surface of the ramus and angle of the mandible. A smaller deep part of the masseter with more vertical fibers may be seen posterior to the upper portion of the main superficial part. The masseteric nerve (V3) and artery traverse the mandibular (sigmoid) notch (N17) from the infratemporal fossa to enter the deep surface of the masseter.
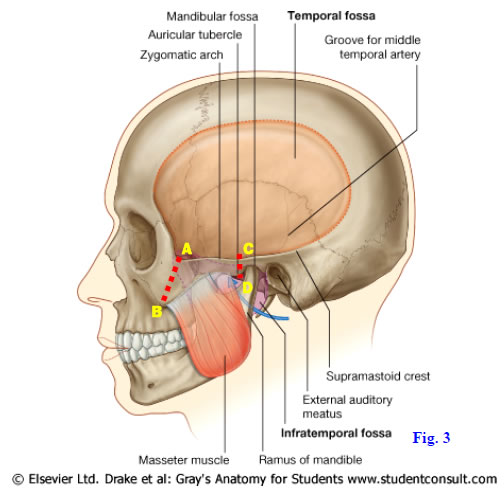
2. This dissection involves FIVE SAW CUTS (Figs. 3, 3A). Scrape the periosteum from the superficial surface of the zygomatic arch. Put a probe deep to the zygomatic arch and push it as far anteriorly as possible (note that when this is done properly, the probe will be oriented obliquely downward and forward). (1) Using a Stryker saw, cut through the bone superficial to the probe (A⇒B). (2) Now make a second vertical saw cut posteriorly, just IN FRONT OF the temporomandibular joint (C⇒D). The condyle of the mandible protrudes slightly laterally below the temporal bone and can be used as a landmark if you are unsure of the correct location. Now reflect the zygomatic arch and attached masseter muscle downward toward the angle of the mandible, but DO NOT COMPLETELY DETACH THE MASSETER from the mandible. The masseteric nerve and vessels will be torn during this procedure, but look for them as you are reflecting the muscle.
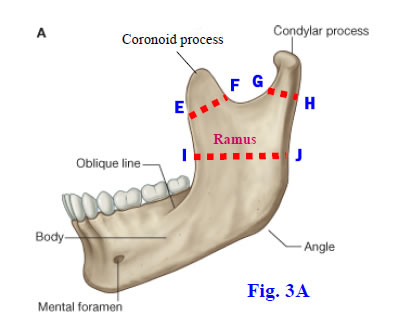
3. Remove the tough temporal fascia from the temporalis muscle and follow the muscle to its attachment on the coronoid process and ramus of the mandible. Note the fan-like shape of the temporalis muscle. Now insert a probe deep to the coronoid process and angle it backward and upward. (3) Saw through the bone superficial to the probe (E⇒F) and reflect the coronoid process and attached temporalis superiorly.
4. (4) Cut through the neck of the mandible near the base of the condylar process (G⇒H). Then place a probe or the handle of a scalpel (without the blade!) deep to the ramus of the mandible and orient it horizontally. Push the probe inferiorly as far as possible—it will catch on the sphenomandibular ligament, which attaches to the lingula of the mandible. (5) Using the probe as an indicator of the appropriate level, saw through the ramus (I⇒J). DO NOT SAW THROUGH THE RAMUS INFERIOR TO THE LODGED PROBE OR SCALPEL HANDLE, or you will cut the inferior alveolar nerve and vessels. Remove the freed portion of the ramus. XXX
The maxillary artery is one of the terminal branches of the external carotid artery. It is divided into three parts in relation to the lateral pterygoid muscle (Gr 7.47, 7.48; N39, 69, 135). The first (mandibular) part passes from the posterior border of the ramus to the lateral pterygoid muscle. Its first two branches, the deep auricular and anterior tympanic arteries, are small and may be difficult to find. The important middle meningeal branch passes through a split in the auriculotemporal nerve and traverses the foramen spinosum to enter the middle cranial fossa. It divides into anterior and posterior branches that supply the meninges and overlying bone of much of the cranial vault (Gr 7.12; N100). The accessory meningeal artery branches either directly from the maxillary artery or from the middle meningeal artery. It traverses the foramen ovale to enter the middle cranial fossa. The inferior alveolar artery is the principal blood supply to the mandible and mandibular teeth. It descends to enter the mandibular foramen.
The second (pterygoid) part of the maxillary artery may pass either superficial or deep to the lateral pterygoid muscle (Gr 7.47A, 7.48A; N39, 69). It sends masseteric, deep temporal, and pterygoid branches to the muscles of mastication. Its buccal branch passes forward deep to the ramus of the mandible and leaves the infratemporal fossa to supply the buccinator muscle of the cheek.
The third (pterygopalatine) part enters the pteryopalatine fossa via the pterygomaxillary fissure (Gr 7.47A, 7.48A; N39, 69). Two of its branches are frequently visible in this dissection, the posterior superior alveolar and infraorbital arteries. The posterior superior alveolar artery enters the posterior superior alveolar foramen on the infratemporal surface of the maxilla. There may be two or three smaller arteries instead of a single larger one. The infraorbital artery traverses the inferior orbital fissure to enter the orbit. The other branches of the third part of the maxillary artery are currently hidden from view and will be seen in later dissections.
The pterygoid plexus of veins is clinically important, but often difficult to demonstrate in dissection. The plexus surrounds the lateral pterygoid muscle before coalescing laterally to form one or two maxillary veins, which join the superficial temporal vein to form the retromandibular vein. The pterygoid plexus receives tributaries corresponding to branches of the maxillary artery. It connects superiorly with the cavernous sinus beside the sella turcica in the middle cranial fossa via an emissary vein (Gr 7.16A, Table 7.4 [p. 607]; N70, 85). The emissary vein may traverse an occasional foramen, the sphenoidal emissary foramen (of Vesalius), or the foramen ovale (N13). Thus an infection in the pterygoid plexus, carried to it from an abscessed tooth or from the facial vein via the deep facial vein, can travel to the cavernous sinus. Even with antibiotic treatment, the resulting cavernous sinus thrombosis results in life-threatening meningitis.
The mandibular branch of the trigeminal nerve (V3) is the only division of the trigeminal nerve that carries motor fibers to skeletal muscles (Gr 7.23A, Tables 9.5 [p. 806], 9.8 [p. 810]; N45, 71, 117, 121). The mandibular division leaves the sensory trigeminal ganglion in the middle cranial fossa and descends through the foramen ovale to reach the infratemporal fossa. This sensory division is followed and joined by the small motor division of V just below foramen ovale. The masseteric and deep temporal branches have already been described.
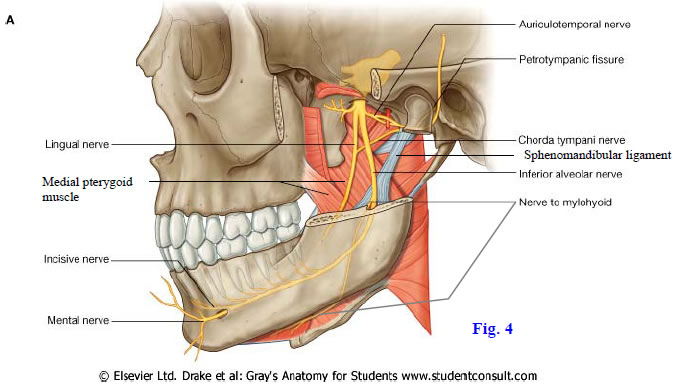
Other branches of the mandibular nerve are the inferior alveolar, lingual, auriculo-temporal, and buccal nerves. The inferior alveolar nerve descends toward the mandibular foramen, giving off the nerve to the mylohyoid just before entering. The inferior alveolar nerve is sensory to the mandibular teeth (Fig. 4; Gr 7.47, 7.49, 7.60A; N45, 71). The nerve enters the mandibular foramen lateral to the whitish, flattened spheno-mandibular ligament, which descends from the spine of the sphenoid bone to the lingula of the mandible (N55). The mental branch of the inferior alveolar nerve exits the mental foramen below the second premolar tooth to supply skin of the lower lip and chin, mucous membrane of the lower lip and the labial gingiva. The other terminal branch of the inferior alveolar nerve is the incisive nerve to the mandibular canine and incisor teeth.
The slender nerve to the mylohyoid grooves the ramus of the mandible as it descends to run parallel to the inferior border with the submental branch of the facial artery. The mylohyoid nerve is motor to two suprahyoid muscles, the mylohyoid and anterior belly of the digastric. These muscles can function as accessory muscles of mastication, depressing the mandible if the hyoid bone is fixed in position from below by the infrahyoid muscles.
The lingual nerve emerges from deep to the lateral pterygoid muscle with the inferior alveolar nerve (Gr 7.47A; N45, 55, 71). It descends on the medial pterygoid muscle anterior and medial to the inferior alveolar nerve en route to the anterior 2/3 of the tongue. As will be seen later, it is joined by the chorda tympani branch of VII high in the infratemporal fossa (Gr 7.47B, 7.49A; N45, 71, 130). The chorda tympani carries preganglionic parasympathetic nerve fibers from the facial nerve destined for the submandibular ganglion in the floor of the oral cavity (Gr Table 9.15 [p. 822]; N122, 132). Postganglionic parasympathetic fibers from the submandibular ganglion supply the submandibular and sublingual salivary glands. The chorda tympani also carries the sensation of taste (SVA fibers) from the anterior 2/3 of the tongue, while the lingual nerve carries general sensation from the anterior 2/3 of the tongue via GSA fibers (N62).
The auriculotemporal nerve is a sensory nerve that passes posteriorly from the mandibular nerve. It splits around the middle meningeal artery, which is a useful landmark in the region and passes behind the neck of the mandible (Fig. 4; Gr 7.47B; N45, 71). The auriculotemporal nerve ascends across the zygomatic arch with the superficial temporal vessels. In the first part of its course it carries postganglionic parasympathetic nerve fibers from the otic ganglion to the parotid gland (Gr Tables 9.11 [p. 817], 9.15 [p. 822]; N124, 133). Preganglionic parasympathetic fibers are carried to the otic ganglion by the lesser petrosal branch of the glossopharyngeal nerve (CN IX).
The sensory buccal branch of the trigeminal nerve passes between the two heads of the lateral pterygoid muscle (Gr 7.47A, 7.49A; N45, 71). It was seen previously emerging onto the buccinator muscle from deep to the ramus of the mandible. The buccal nerve pierces the buccinator muscle and is sensory to buccal mucosa. It does not innervate the buccinator muscle, which is a muscle of facial expression innervated by the facial nerve (CN VII).
5. Locate where the maxillary artery branches from the external carotid artery. Follow the maxillary artery medially and try to find branches from the part lateral to the lateral pterygoid muscle (first part of maxillary artery). The only branches that may be visible at this point are the inferior alveolar artery and a small artery that accompanies the lingual nerve. Clean the inferior alveolar artery and vein as they descend toward the mandibular foramen lateral to the sphenomandibular ligament (N18). Look for this thin, flattened ligament, which may easily be rolled into a structure that looks like a nerve.
6. Trace the inferior alveolar vein superiorly to the maxillary vein. Be aware that the maxillary vein is formed by the coalescence of the pterygoid venous plexus, which has clinically important connections, but remove the venous plexus to expose other structures.
7. Clean the inferior alveolar nerve emerging from deep to the lateral pterygoid muscle to enter the mandibular foramen with the inferior alveolar artery and vein (Gr 7.47). Look for the nerve to the mylohyoid branching from the inferior alveolar nerve. If it branches immediately above the mandibular foramen, the nerve may be difficult to see at this time. Clean the lingual nerve emerging from deep to the lateral pterygoid muscle anterior and medial to the inferior alveolar nerve.
8. Look for the buccal nerve and buccal artery emerging from between the two heads of the lateral pterygoid muscle (Gr 7.47A). Follow them forward onto the buccinator muscle. XXX
The lateral pterygoid muscle is transversely oriented within the infratemporal fossa (Gr 7.47A, 7.48, 7.49,Table 7.9 [p. 662]; N45, 55). It has two heads with the superior head passing from the infratemporal surface of the greater wing of the sphenoid to the articular capsule and articular disc of the temporomandibular joint (TMJ) (Gr 7.51A; N55). Electromyographic (EMG) studies have shown that the superior head of the lateral pterygoid contracts eccentrically during jaw closure by the masseter, temporalis, and medial pterygoid muscles to protect the teeth from overly forceful closure. The inferior head of the lateral pterygoid passes from the lateral surface of the lateral pterygoid plate to insert into the capsule of the TMJ and pterygoid fovea on the neck of the mandible. It is active in protrusion and depression of the mandible, and these are the usual actions ascribed to the lateral pterygoid muscle. Unilateral contractions also contribute to side-to-side movements of the mandible during chewing.
The medial pterygoid muscle takes origin from the medial surface of the lateral pterygoid plate (deep head) and the maxillary tuberosity (superficial head). It descends slightly posteriorly and laterally to attach on the medial surface of the angle and lower part of the ramus of the mandible (Fig. 4; Gr 7.47A-B, Table 7.9 [p. 662]; N45, 55). Note that this attachment on the medial surface of the mandible corresponds to the attachment of the masseter on the lateral surface, and that these two muscles form a mandibular sling (Gr 7.90B). The medial pterygoid is a mandibular elevator. Unilateral contractions assist the lateral pterygoid muscles in side-to-side movements of the mandible.9. Carefully pick away the lateral pterygoid muscle piecemeal. Trying to cut out large portions of it usually results in damage to the neurovascular structures that we want to preserve.
10. Clean the second part of the maxillary artery. Look for anterior and posterior deep temporal branches passing superiorly deep to the temporalis muscle. The other muscular branches will already have been torn. Even if the maxillary artery runs superficial to the lateral pterygoid muscle, the middle meningeal branch of the first part is usually easier to dissect after the muscle is removed. Clean the middle meningeal artery. Finding where it passes through the split in the auriculotemporal nerve to enter the foramen spinosum is a useful landmark in this region. Look for the smaller accessory meningeal artery. It may branch directly from the maxillary artery or from the middle meningeal artery. Trace the accessory meningeal artery toward the foramen ovale, where the mandibular nerve is exiting the cranial cavity.
11. Follow the maxillary artery medially toward the pterygomaxillary fissure. Look for two branches that are described as branches of the third part of the maxillary artery, but arise near the pterygomaxillary fissure, sometimes within the infratemporal fossa. The posterior superior alveolar artery enters a foramen on the infratemporal surface of the maxilla. Look for the posterior superior alveolar nerve, a branch of the maxillary nerve (V2), exiting the pterygopalatine fossa through the pterygomaxillary fissure to enter the maxilla near the artery. The point at which the infraorbital branch of the maxillary artery arises is somewhat variable, and the infraorbital artery may be visible traversing the inferior orbital fissure to enter the orbit.
12. Find the lingual nerve as it descends from the trunk of the mandibular nerve. It may be easier to pick the lingual nerve up where it was seen earlier, anterior to the inferior alveolar nerve and follow it superiorly. Identify the slender, but important, chorda tympani nerve joining the posterior aspect of the lingual nerve. Be aware of its functional significance.
13. Keep the medial pterygoid muscle intact, but clean the exposed portion of its lateral surface. Notice how the medial pterygoid joins the masseter muscle in forming a sling for the mandible. XXX
Although we aren’t going to take time to dissect the temporomandibular joint (TMJ), injuries and diseases that affect it are capable of causing a distressing variety of symptoms (see http://emedicine.medscape.com/article/1143410-overview ), and an understanding of the joint’s basic structure and function is useful at this point. The TMJ is a synovial joint formed between the head (condyle) of the mandible and the articular tubercle (articular eminence) of the squamous portion of the temporal bone (Gr 7.44A, 7.45, 7.47, 7.50; N18, 54, 55). Note the close relationship of the roof of the mandibular fossa to the floor of the middle cranial fossa housing the temporal lobe of the brain (Gr 7.50A).
The TMJ differs from most synovial joints in that its articular surfaces are covered by dense fibrous connective tissue rather than hyaline cartilage. The fibrous articular capsule of the TMJ is strengthened laterally by the lateral temporomandibular ligament descending from the articular tubercle to the neck of the mandible (N18). Sensory innervation is mainly by the masseteric and auriculotemporal branches of V3, and the TMJ is a frequent site of referred pain.
The joint cavity of the TMJ is subdivided into upper and lower joint cavities by a fibrous and fibrocartilaginous articular disc (Gr 7.50, 7.51A; N18, 55). The central portion of the disc is avascular and aneural, as would be expected to prevent neurovascular compression. Gliding movements occur in the superior joint cavity with the head of the mandible and articular disc together gliding forward or backward on the articular tubercle. Hinge (rotary) movements occur in the inferior joint cavity of the TMJ with the head of the mandible rotating around a transverse axis. Opening the jaws too widely (as in yawning during one of Dr. Roy’s lectures) may result in dislocation of the head of the mandible anterior to the articular tubercle (Gr 7.51 CT and MRIs). For anyone who may have a special interest in the TMJ, see Hylander, W. L., 2006 Functional Anatomy and Biomechanics of the Masticatory Apparatus. In: Temporomandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment, D. M. Laskin et al. (Eds.), Quintessence Publishing Co., Inc., Chicago, pp. 3-34.
14. When your hands are clean place a finger into, or just in front of, your external acoustic meatus and feel the movement of the condyle of the mandible as you open and close your jaws. With your finger still in place, move your chin from side-to-side. (Hint: if you have a spouse, another significant other, or roommate, you may want to wait until that person has left the room before performing this exercise.) XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.