Orbit, Disarticulation of the Skull
ORBIT, DISARTICULATION OF THE SKULL
During this period we will dissect the orbit using a superior approach by removing part of the floor of the anterior cranial fossa. After studying the orbit we will disarticulate the skull from the atlas to facilitate later dissections.
The head is organized around a series of functional spaces, and this organization is reflected in the structure of the skull. The orbits are bony cavities on either side of the root of the nose. They are involved in vision and contain the eyeballs and optic nerves, extraocular muscles that move the eyes, and associated nerves and blood vessels.
Each orbit is formed by 7 bones and forms a 4-sided pyramid with a posterior apex and an anterior base (Fig. 2; Gr 7.1B, 7.36A; N4, 84). The orbit has medial and lateral walls, a roof, and a floor.
The medial wall is formed mainly by the orbital plate of the ethmoid bone (lamina papyracea) along with contributions from the frontal process of the maxilla and the lacrimal and sphenoid bones. Small anterior and posterior ethmoidal foramina are present near the junction of the roof and medial wall (frontoethmoid suture). Anteriorly the medial wall has a depression for the lacrimal sac (fossa for the lacrimal sac) (Gr 7.36A, 7.37A; N4, 82). The bone of the orbital plate of the ethmoid separating the cavity of the orbit from the spaces of the ethmoidal air cells (ethmoidal paranasal sinus) is paper thin (Gr 7.38A-B; N5, 48), and life-threatening orbital infections (orbital cellulitis) may result from ethmoidal sinusitis. The medial walls of the two orbits are separated by the upper portion of the nasal cavities in addition to the ethmoidal air cells (Fig. 3).
The lateral wall of the orbit is formed by the frontal process of the zygomatic bone and the greater wing of the sphenoid bone. The lateral wall doesn’t extend as far anteriorly as the medial wall of the orbit, and so provides a surgical approach to the eye (Gr 7.2). The lateral wall is the thickest, strongest wall, which is important because it is most exposed to direct trauma.
Although the medial walls of the orbits are nearly parallel, the lateral walls diverge from each other at approximately a 90° angle (Fig. 2). Consequently, the axes of the orbits form a 45° angle with each other. Since the optical axes (axes of the eyeballs) are parallel, they differ from the orbital axes. Since most of the extraocular muscles attach near the apex of the orbit, this divergence of the optical and orbital axes has significant implications for how the muscles move the eyeballs.
The roof of the orbit is formed mainly by the orbital part of the frontal bone with a contribution near the apex from the lesser wing of the sphenoid. Anterolaterally in the roof is a depression for the orbital part of the lacrimal gland (fossa for the lacrimal gland, lacrimal fossa) (Gr 7.37A). The roof separates the orbit from the floor of the anterior cranial fossa (Fig. 3; Gr 7.74, 7.76; N5). The frontal sinus extends posteriorly into the orbital plate of the frontal bone for a variable distance (Gr 7.68, 7.69, 7.71A-B; N5, 8, 48), and frontal sinusitis has been reported to result in infections of the orbit and abscesses of the frontal lobe of the brain (e.g., see http://emedicine.medscape.com/article/212946-overview ). The relatively thin bone of the roof of the orbit also means that a sharp object, such as a knife or a pencil, that penetrates the orbit in a superior direction may penetrate the frontal lobe.
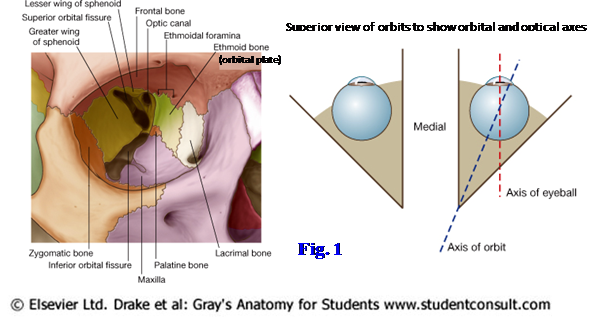
The floor of the orbit is formed mainly by the orbital surface of the maxilla with smaller contributions from the zygomatic bone laterally and the orbital process of the palatine bone posteromedially (Fig. 2). The floor features the infraorbital groove leading into the infraorbital canal for the infraorbital nerve and vessels. The floor separates the orbit from the maxillary sinus (Fig. 3; Gr 7.74). A blow to the eyeball (e.g., from a handball) may violently displace the orbital contents inferiorly, fracturing the floor of the orbit (blowout fracture). Usually the infraorbital nerve and vessels (Gr 7.39A, 7.72B, 7.74A, 7.89C; N48, 83) prevent the eyeball itself from entering the maxillary sinus, but the inferior rectus muscle may become wedged in a fracture, limiting eye movements ( http://www.emedicine.com/oph/topic229.htm ). Hemorrhage may occur from a damaged infraorbital artery. An inferior blowout fracture is unlikely in children because the small size of the maxillary sinus means that the floor of the orbit is relatively stronger than in adults.
The base of the orbit is located anteriorly (Gr 7.36, 7.38, 7.92D & E, 7.93A; N4, 84). It is formed by the orbital opening bounded by the thick bone of the orbital margin, which provides some protection to the orbital contents. The supraorbital margin is the boundary of the squamous and orbital parts of the frontal bone. It has a supraorbital notch (in some cases a foramen) for the supraorbital nerve and vessels. Just superior to each supraorbital margin is a ridge, the superciliary arch, deep to the eyebrows. The ridge is generally more prominent in adult males.
The infraorbital margin is formed by the maxilla and zygomatic bone. The infraorbital foramen, which is the opening for the infraorbital canal, is located inferior to its midpoint.
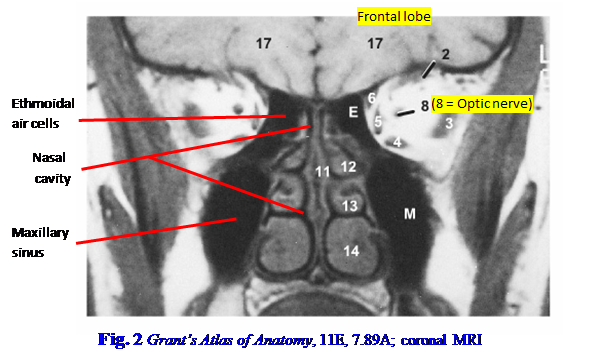
The apex of the orbit is the optic canal, which is located between the body and the roots of the lesser wing of the sphenoid bone (Fig. 2; Gr 7.36A, 7.38B; N4). The optic nerve leaves the orbit via the optic canal, and the ophthalmic artery enters the orbit from the middle cranial fossa through it. The optic canal is closely related to the sphenoid sinus and posterior ethmoidal air cells (Gr 7.38, 7.68A, 7.69A; N48, 83), and the optic nerve may be infected from these paranasal sinuses or injured during surgery on them.
The optic canal is just medial to the superior orbital fissure, which lies between the greater and lesser wings of the sphenoid bone (Fig. 2; Gr 7.36; N4, 86). The superior orbital fissure connects the orbit with the middle cranial fossa. It provides passage for most of the nerves and vessels entering or leaving the orbit, including cranial nerves III, IV, VI, and V1 and the ophthalmic veins.
The inferior orbital fissure separates the floor of the orbit from its lateral wall (Fig. 2; Gr 7.36, 7.44A; N4). It connects the orbit with the pterygopalatine fossa posteriorly and with the infratemporal fossa more laterally. The infraorbital nerve and artery (Gr 7.47, 7.48A; N44, 69) and the zygomatic branch of the maxillary nerve (Gr 7.70, 7.72B; N44) enter the orbit from the pterygopalatine fossa via the inferior orbital fissure. A vein connecting the pterygoid venous plexus of the infratemporal fossa and the inferior ophthalmic vein traverses the fissure, providing an indirect route for the spread of infection into the cranial cavity (Gr 7.16A, 7.40C; N70, 85).
Anterior and posterior ethmoidal foramina for vessels and nerves of the same name are present in or near the frontoethmoidal suture on the medial wall of the orbit (Fig. 2; Gr 7.36A, 7.38, Table 7.6 [p. 647]; N4, 85, 86). The anterior and posterior ethmoidal arteries are branches of the ophthalmic artery, and the corresponding nerves are branches of the nasociliary nerve from V1. The fossa for the lacrimal sac opens into the bony nasolacrimal canal, which contains the membranous nasolacrimal duct that drains the collected lacrimal fluid into the inferior meatus of the nasal cavity (Gr 7.37, 7.67; N82). That’s why someone’s nose runs when s/he cries, as from joy at the prospect of attending gross anatomy class.
The periosteum lining the orbit is given the special name “periorbita.” Extensions of the periorbita into the upper and lower eyelids from the supraorbital and infraorbital margins, respectively, form the orbital septum (Gr 7.39B; N81). The orbital septum is clinically important because it helps separate the preseptal (periorbital) space from the postseptal (orbital) space. A less serious periorbital infection (preseptal cellulitis) rarely spreads into the orbit. An orbital infection (orbital cellulitis) is more serious and usually requires hospitalization and intravenous antibiotics (e.g., see http://www.emedicine.com/oph/topic205.htm ).
CONTENTS OF THE ORBIT
The eyeball occupies most of the anterior portion of the orbit. The eyeball is essentially a sphere with an anterior bulging segment, the cornea (Fig. 4; Gr 7.36B-C, 7,38C, 7.39; N83, 87, 88). The eyeball consists of three layers: an outer fibrous layer, a middle vascular layer, and an inner nervous layer (Fig. 4; Gr 7.41, 7.42; N87). The cornea is the transparent anterior 1/6 of the fibrous layer and admits light into the eye. It is avascular (N90, 91) but richly innervated with sensory fibers by the nasociliary nerve (V1). The sclera is the tough, opaque posterior 5/6 of the fibrous layer. It is the “white of the eye.” The sclera is the fibrous skeleton of the eyeball and gives attachment to the extraocular muscles that move the eye.
The middle vascular layer of the eyeball, or uvea, is formed by the choroid, ciliary body, and iris (Gr 7.41, 7.42; N90, 91). The choroid is the large posterior part of the uvea and lines most of the sclera. It has a rich vascular supply which, importantly, supplies the layer of photoreceptor cells in the outer part of the nervous retina.
The ciliary body connects the choroid and the circumference of the iris (Fig. 4; Gr 7.41; N87, 88, 90). The ciliary body forms a complete ring around the the transparent, elastic, biconvex lens, which it suspends from ciliary processes by the suspensory ligament of the lens (ciliary zonule). Contraction of the circularly arranged smooth muscle fibers of the ciliary muscle under preganglionic parasympathetic control by the oculomotor nerve (III) draws the ciliary processes closer to the lens. This reduces tension on the suspensory ligament and allows the natural elasticity of the lens to make it more rounded for near vision (accommodation). The lens loses elasticity as we age and may remain too flattened to allow a good focus of the image on the retina for near objects. The inability to see near objects clearly with age is presbyopia.
The ciliary processes also form aqueous humor, which circulates from the posterior chamber through the pupil into the anterior chamber of the eye (Gr 7.42B; N87, 88). The aqueous humor nourishes the inner part of the cornea and, along with the gelatinous vitreous humor (vitreous body) behind the lens (Gr 7.41; N87), helps maintain intraocular pressure. The aqueous humor is absorbed into the scleral venous sinus (of Schlemm) at the iridocorneal junction in the anterior chamber (N87, 88, 91).
Increased intraocular pressure due to decreased absorption of aqueous humor (glaucoma) compresses the retina and retinal arteries and may result in blindness. Unfortunately, most patients don’t notice the gradual visual loss, which initially is at the periphery of the visual field, until significant damage has occurred. A less common form of glaucoma (closed-angle glaucoma) is painful and causes sudden visual loss, but in most patients glaucoma is symptomless early in its course. For a patient’s guide, see http://www.merckmanuals.com/home/sec20/ch233/ch233a.html
The iris is a thin, circular, adjustable diaphragm with a central opening, the pupil (Fig. 4). The iris separates the anterior chamber of the eye located in front of it from the posterior chamber located behind it. The iris is responsible for eye color due to its distribution of the pigment melanin. It contains two smooth muscles that control the size of the pupil and, therefore, the amount of light entering the eye. The sphincter pupillae (constrictor pupillae) muscle constricts the pupil under preganglionic parasympathetic control by the oculomotor nerve. The postganglionic parasympathetic fibers are from cell bodies in the ciliary ganglion. The dilator pupillae muscle dilates the pupil under control of postganglionic sympathetic fibers from cell bodies in the superior cervical sympathetic ganglion.
When the oculomotor nerve is compressed (e.g., due to a transtentorial herniation), the parasympathetic fibers, which are located peripherally in the nerve, are affected first and the pupil dilates (mydriasis) due to paralysis of the sphincter pupillae muscle. When the sympathetic innervation is interrupted, as in Horner’s syndrome, the pupil constricts (miosis).
The inner layer of the eyeball is the retina (Figs. 4, 5; Gr 7.41A; N87, 119). It consists of a posterior optic part and an anterior non-visual part, which meet at the ora serrata, the scalloped posterior border of the ciliary body. The optic retina is formed by an inner light-receptive neural layer and an outer pigment layer. The neural layer comprises multiple cell layers with the layer of photoreceptor cells—rods and cones—located most peripherally (i.e., farthest from the vitreous humor) so that light has to traverse the other layers to reach it (Fig. 5). The innermost layer of the optic retina is formed by ganglion cells, and their axons converge at the optic disc (optic papilla) to form the optic nerve (Fig. 5). The optic disc lacks rods and cones and, therefore, is the blind spot of the eye—light rays that land on the optic disc are not seen.
Just lateral to the optic disc is a small, yellowish oval area, the macula lutea. It contains a central depression, the fovea centralis (Fig. 4), which has the more superficial layers of the retina (i.e., those closest to the vitreous humor) pulled aside to expose its packed cone cells to light. The fovea centralis is the point of greatest visual acuity in the eye.
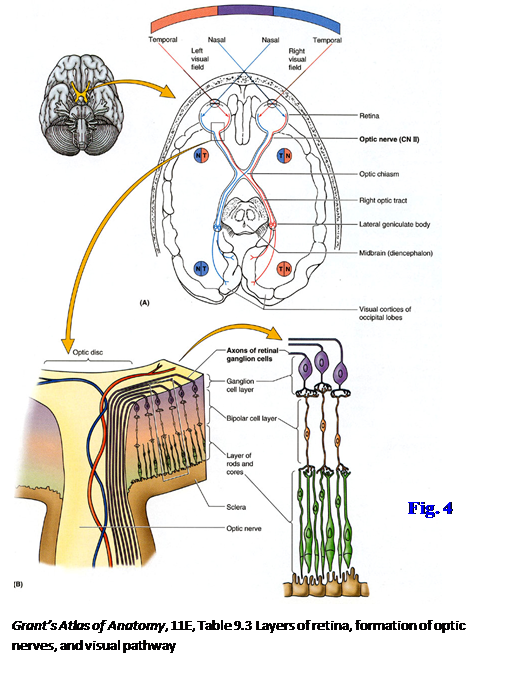
The outer pigment layer of the optic retina borders the choroid layer. The pigment layer is a single layer of cells that reduces the scattering of light inside the eye. It originally formed the outer layer of the embryonic optic cup, and the neural retina formed the inner layer (Fig. 6). In a detached retina, the neural and pigment layers of the optic retina separate, re-creating the intraretinal space of the optic cup (e.g., see http://emedicine.medscape.com/article/798501-overview ). Although the inner cells of the neural layer, those closest to the vitreous humor, receive their nourishment from branches of the central artery of the retina, which enters the eye at the optic disc, the layer of rods and cones is nourished by diffusion through the pigment layer from vessels of the choroid. Consequently a detached retina (e.g., following a blow to the eye) results in loss of the photoreceptor cells of the affected area with loss of vision.
The extraocular muscles include one muscle that elevates the upper eyelid and six muscles that move the eye to direct the pupil toward the object to be viewed. The muscle of the upper eyelid is the levator palpebrae superioris (Gr 7.38A, 7.39, 7.40A-B; N81, 83, 84, 86). It takes origin from the lesser wing of the sphenoid bone above the optic canal and passes anteriorly to insert into a dense fibrous plate in the upper eyelid, the superior tarsal plate. The levator palpebrae superioris elevates the upper eyelid under voluntary (GSE) control of the oculomotor nerve. The levator has a small inferior offshoot composed of smooth muscle, the superior tarsal muscle (of Müller) (Gr 7.39B; N81). The superior tarsal muscle is under sympathetic (GVE) control. Therefore, a lesion of the oculomotor nerve results in complete ptosis and inability to voluntarily raise the upper eyelid, but Horner’s syndrome results in partial ptosis while retaining the ability to voluntarily raise the upper eyelid.
The four recti (straight) muscles share an origin from a fibrous ring that surrounds the optic canal and part of the superior orbital fissure. This common tendinous ring (anulus tendineus), therefore, forms a muscular cone into which initially pass most of the structures entering the orbit (Gr 7.38A [left side], 7.39A, 7.40B, 9.5; N83, 84, 86). The exceptions are the frontal, lacrimal, and trochlear nerves and the ophthalmic veins, which enter the orbit outside of the muscular cone.
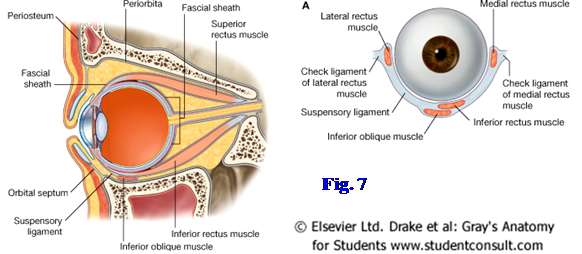
The superior, inferior, medial, and lateral rectus muscles all pass from the common tendinous ring to attach into the sclera of the anterior half of the eyeball (Fig. 7; Gr 7.40A-B, Table 7.7 [p. 648]; N84). The medial and lateral recti occupy the same horizontal plane and produce the simple adduction and abduction movements of the pupil, respectively, that one would expect. The superior and inferior recti muscles lie in the same vertical plane, but this is in the orbital axis rather than the optical axis. Consequently, the individual action of the superior rectus is the move the pupil superiorly and medially from the anatomical position, while the inferior rectus moves the pupil inferiorly and medially (Gr Table 7.8 [p. 649]). All of the recti except the lateral rectus are innervated by the oculomotor nerve (III). The lateral rectus muscle, the abductor of the pupil, is innervated by the abducent nerve (VI).
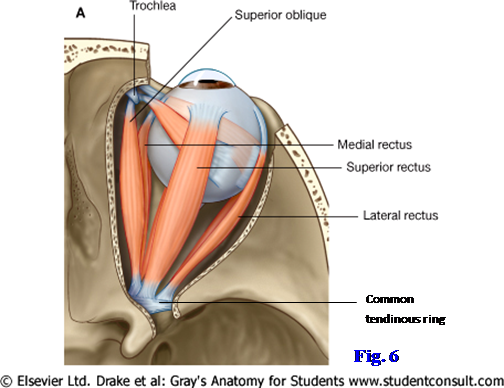
The superior oblique muscle takes origin from the body of the sphenoid medial to the superior part of the common tendinous ring. The muscle passes forward along the superomedial corner of the orbit to the trochlea (Fig. 7; Gr 7.37A; N83, 84). The trochlea is a small piece of cartilage suspended from the orbital margin at the trochlear fovea (or trochlear spine) by a sling of fibrous connective tissue. The tendon of the superior oblique hooks around the trochlea to turn posterolaterally and pass between the superior rectus muscle and the eyeball. It inserts into the sclera of the superior lateral quadrant of the posterior half of the eyeball. The superior oblique muscle has an individual action of moving the pupil inferiorly and laterally from the anatomical position (Gr Table 7.8 [p. 649]). It is innervated by the trochlear nerve (IV), which receives its name from the trochlea.
The inferior oblique muscle takes origin from the anteromedial portion of the floor of the orbit (Gr 7.37A, 7.39, 7.40A; N84, 120). It passes posterolaterally under the inferior rectus muscle to insert into the inferior lateral quadrant of the posterior half of the eyeball. The inferior oblique, acting individually, moves the pupil of the eye superiorly and laterally. It is innervated by the oculomotor nerve.
Although the individual action of each extraocular muscle starting from the anatomical position is described above, multiple muscles are involved in every eye movement, and this fact is used in testing the muscles clinically (see Moore Figs. 7.34E & 7.35). Thus, the superior oblique muscle depresses the pupil of the already adducted eye, and the inferior oblique elevates it. The superior rectus elevates the abducted eye, and the inferior rectus depresses it. Part of the physical examination also is testing the coordinated movements of the two eyes that are necessary for binocular vision. For example, having the patient look directly to the left requires coordinated contractions of the left lateral rectus and right medial rectus muscles. You will study how the central nervous system controls these movements in Neuroscience.
Before leaving a consideration of eye movements, it is important to mention one other important structure that is difficult to demonstrate in dissection. The eyeball from the optic nerve anteriorly to near the corneoscleral junction is enclosed by a connective tissue layer, the fascial sheath of the eyeball (bulbar sheath, Tenon’s capsule), which is pierced by the tendons of extraocular muscles (Fig. 8; Gr 7.39B; N83). The fascial sheath forms a socket within which the eye moves by the contraction of the extraocular muscles. The sheath is reinforced inferiorly between the anterior portions of the medial and lateral rectus muscles as the suspensory ligament of the eyeball. If the eye has to be surgically removed, an attempt is made to spare the fascial sheath and suspensory ligament to form a socket for the artificial eye.
The optic nerve is formed by the axons of ganglion cells. It is enclosed by extensions of the cranial meninges and subarachnoid space as it passes to the apex of the orbit and traverses the optic canal (Gr 7.39B-C, Table 7.6 Transverse Section [p. 647]; N87). The central artery of the retina, which is a branch of the ophthalmic artery, pierces the inferior surface of the optic nerve and enters the eye at the optic disc (Gr 7.41A, 7.42, Table 7.6 [p. 647]; N87, 90, 91). The central vein of the retina accompanies the distal part of the artery but leaves it en route to the cavernous sinus. Due to the extension of the subarachnoid space around the optic nerve, an increase in intracranial pressure reduces venous return from the retina and inhibits axoplasmic transport to produce swelling of the optic disc (papilledema). There are other causes of a swollen optic disc (e.g., optic neuritis), but it is often the first sign of increased intracranial pressure. Papilledema of unknown origin is a contraindication to lumbar puncture, which could cause a fatal brain herniation in the presence of a mass lesion (see http://www.merckmanuals.com/professional/sec09/ch107/ch107e.html ).
The ophthalmic division of the trigeminal nerve (V1) is the sensory nerve of the orbital region. It leaves the trigeminal ganglion and is embedded in the lateral wall of the cavernous sinus as it passes toward the superior orbital fissure (Gr 7.18, 7.22, 7.23A, Table 9.6 [p. 807]; N44, 86, 121). The frontal nerve is the largest of the three terminal branches of the ophthalmic nerve (Gr 7.38A, 7.39A; N44, 86). It enters the orbit above the common tendinous ring and divides into supraorbital and supratrochlear nerves at a variable distance into the orbit (Gr 7.10, 7.37A, 7.38A; N44, 86). The supraorbital nerve divides into medial and lateral branches. It was seen previously ascending into the forehead from the supraorbital notch or foramen. The supratrochlear nerve passes just above the trochlea to enter the forehead medial to the supraorbital nerve.
The lacrimal nerve is the smallest of the three branches of V1 (Gr 7.38, 7.39A, 7.70, 7.72B, Table 9.6 [p. 807]; N44, 86). It enters the orbit above the common tendinous ring and passes along the superolateral corner of the orbit, above the lateral rectus muscle. The lacrimal nerve supplies the lacrimal gland and the skin of the lateral portion of the upper eyelid. It receives postganglionic parasympathetic nerve fibers from cell bodies in the pterygopalatine ganglion that reach it via the zygomatic branch of the maxillary nerve (V2) (N44, 132). These parasympathetic fibers are secretomotor fibers. The postganglionic sympathetic innervation from cell bodies in the superior cervical sympathetic ganglion also reaches the lacrimal gland via the zygomatic nerve. These sympathetic fibers traverse the pterygopalatine ganglion from the deep petrosal nerve without synapsing and are vasoconstrictive.
The nasociliary nerve is the third terminal branch of the ophthalmic nerve (Gr 7.38, 7.39A; N44, 86). It enters the orbit through the part of the superior orbital fissure enclosed by the common tendinous ring and crosses medially above the optic nerve. The nasociliary nerve sends a branch to the ciliary ganglion, the sensory root, just after entering the orbit (N130, 131). These are sensory (GSA) nerve fibers from the eyeball and traverse the ciliary ganglion without synapsing to reach the eye via the short ciliary nerves. The sensory root of the ciliary ganglion also usually carries postganglionic sympathetic fibers that join the ophthalmic nerve from the internal carotid plexus in the cavernous sinus. These sympathetic fibers traverse the ganglion without synapsing to supply the dilator pupillae muscle of the iris and the smooth muscle of blood vessels. Alternatively, the sympathetic fibers may reach the ciliary ganglion in a separate sympathetic root arising in the cavernous sinus (N130).
The nasociliary nerve gives off 3-4 long ciliary nerves as it crosses the optic nerve. These carry sensory fibers from the eye and also may carry postganglionic sympathetic nerve fibers (N131). The sensory fibers supplied to the eye by the nasociliary nerve are tested in the corneal reflex. The examiner touches the cornea with a wisp of cotton, resulting in reflex closure of the eyelids. The afferent limb of the reflex arc, therefore, is by cranial nerve V1 and the efferent limb is by the facial nerve (VII), which supplies the orbicularis oculi muscle.
The posterior ethmoidal branch of the nasociliary nerve passes medially between the superior oblique and medial rectus muscles to enter the posterior ethmoidal foramen (Gr 7.38B; N86). It supplies the mucoperiosteum of the posterior ethmoidal air cells and sphenoid sinus. It may continue across the cribriform plate in the anterior cranial fossa and enter the upper portion of the nasal cavity to help supply general sensation to the nasal mucosa. The posterior ethmoidal nerve sometimes is absent.
The terminal branches of the nasociliary nerve are the anterior ethmoidal and infratrochlear nerves (Gr 7.38; N44, 86). The anterior ethmoidal nerve traverses the anterior ethmoidal foramen to supply the anterior ethmoidal air cells and frontal sinus. It continues across the cribriform plate and descends into the anterosuperior part of the nasal cavity, where it supplies the nasal mucosa. It leaves the nasal cavity between the nasal bone and lateral nasal cartilage as the external nasal nerve (N42, 44). The infratrochlear nerve exits the orbit between the trochlea and medial rectus muscles (Gr 7.10A; N44, 86). It is sensory to the lacrimal sac, medial portions of both eyelids, and skin over the root of the nose.
The oculomotor (III), trochlear (IV), and abducent (VI) nerves are the motor nerves of the orbit (N120). The oculomotor nerve passes forward embedded in the lateral wall of the cavernous sinus to reach the superior orbital fissure. It divides into superior and inferior branches/divisions as it enters the orbit within the common tendinous ring (Gr 7.38A, 7.39A, 9.5B, Table 9.4 [p. 804]; N86, 120). The superior branch innervates the levator palpebrae superioris and superior rectus muscles. The inferior branch of the oculomotor nerve sends a branch medially under the optic nerve to the medial rectus muscle and branches that descend to reach the inferior rectus and inferior oblique muscles. The inferior branch also gives of the motor (parasympathetic) root of the ciliary ganglion (N120, 131). The motor root carries preganglionic parasympathetic nerve fibers of the oculomotor nerve to the ciliary ganglion, where they synapse on the cell bodies of postganglionic neurons. The postganglionic parasympathetic fibers pass through the short ciliary nerves to the eye, where they innervate the ciliary and sphincter pupillae muscles.
The slender trochlear nerve courses forward in the lateral wall of the cavernous sinus to the superior orbital fissure (Gr 7.22, 7.23, 7.38; N86, 103, 120). Just before reaching the orbit, it crosses above the oculomotor nerve and enters the orbit above the common tendinous ring. The trochlear nerve pierces the superior surface of the superior oblique muscle.
The abducent nerve pierces the dura of the posterior cranial fossa over the clivus and traverses the cavernous sinus inferolateral to the internal carotid artery (Gr 7.28, 7.22, 7.23; N86, 103). It enters the orbit within the common tendinous ring and passes onto the medial surface of the lateral rectus muscle, which it supplies (Gr 7.38, 7.39A).
The motor innervation of the orbit is easily remembered by the formula LR6SO4AO3. In other words, the lateral rectus muscle is innervated by cranial nerve VI, the superior oblique by cranial nerve IV, and all of the other extraocular muscles are innervated by cranial nerve III.
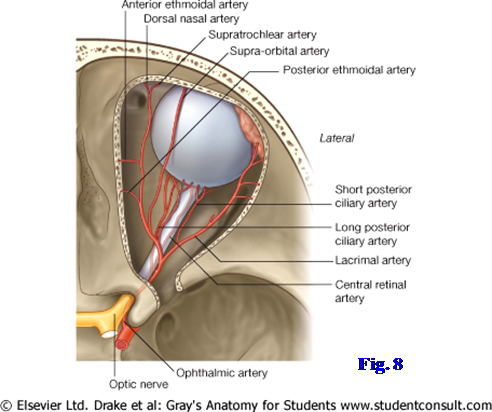
The ophthalmic artery is the blood supply to structures in the orbit (Fig. 9; Gr Table 7.6 [p. 647]; N85). It branches from the internal carotid artery medial to the anterior clinoid process and enters the orbit via the optic canal below the optic nerve. The ophthalmic artery ascends lateral to the optic nerve and passes medially above it to a point near the medial wall of the orbit, where it courses anteriorly. Its branches include the central artery of the retina, lacrimal artery, long and short posterior ciliary arteries, supraorbital artery, posterior and anterior ethmoidal arteries, and its terminal branches, the supratrochlear and dorsal nasal arteries.
The central artery of the retina is the most important branch of the ophthalmic artery (Fig. 9; Gr 7.41, 7.42; N90, 91). It branches from the ophthalmic artery below the optic nerve and pierces it. From the center of the optic nerve it enters the eye through the optic disc and sends branches across the inner surface of the retina. The central artery of the retina supplies blood to all layers of the nervous retina except the layer of rods and cones, which are nourished by diffusion from vessels of the choroid layer. Occlusion of the central artery of the retina by a thrombus from the carotid artery or heart results in instant and usually permanent blindness in the affected eye. Temporary occlusion of the central artery of the retina is one cause of temporary blindness lasting from seconds to hours and known as amaurosis fugax (e.g., http://ijahsp.nova.edu/articles/vol4num2/Bacigalupi.pdf).
The lacrimal artery ascends anteriorly on the lateral side of the orbit to the reach the lacrimal gland and neighboring structures (Fig. 9; Gr 7.38A, Table 7.6 [p. 647]; N85). The long and short posterior ciliary arteries pierce the sclera of the posterior part of the eye and are distributed through the choroid layer (N90, 91). The supraorbital artery usually arises from the ophthalmic artery just after it crosses above the optic nerve. It was seen earlier leaving the orbit with the supraorbital nerve.
The posterior and anterior ethmoidal arteries join nerves to enter foramina of the same name in the medial wall of the orbit (N85). Both supply ethmoidal air cells and cross the cribriform plate in the anterior cranial fossa to enter the nasal cavity. The anterior ethmoidal artery usually gives off an anterior meningeal artery before leaving the cranial cavity. The posterior and anterior ethmoidal arteries supply the upper mucosa of the nasal cavity (N40).
The supratrochlear artery is one terminal branch of the ophthalmic artery (N69, 85). It leaves the orbit above the trochlea with the supratrochlear nerve to supply the forehead. The dorsal nasal artery is the other terminal branch of the ophthalmic artery. It exits the orbit to supply the dorsum of the nose. The dorsal nasal artery often anastomoses with the angular artery, providing collateral circulation between the internal and external carotid arteries that may compensate if slow occlusion of the internal carotid artery occurs.
The venous drainage of the orbit, except the nervous retina, is mainly via the superior and inferior ophthalmic veins (Gr 7.16, 7.40C; N85, 91). The superior ophthalmic vein is formed by the union of the supraorbital and angular veins. As it passes posteriorly in the upper medial part of the orbit, the superior ophthalmic vein receives tributaries mostly corresponding to branches of the ophthalmic artery. In addition it receives vorticose veins (Gr 7.42B; N91) from the upper two posterior quadrants of the eyeball and often the inferior ophthalmic vein as tributaries. The superior ophthalmic vein drains into the cavernous sinus, providing a route for the spread of infection from the middle third of the face (danger area) to the cavernous sinus.
The inferior ophthalmic vein begins by the confluence of small veins in the floor of the orbit with usually a contribution from the angular vein (Gr 7.16A, 7.40C; N85). It receives the vorticose veins from the lower two posterior quadrants of the eyeball (N91). The inferior ophthalmic vein communicates through the inferior orbital fissure with the pterygoid plexus of veins (N70, 85), providing an alternative route for the spread of infection to the cavernous sinus. The inferior ophthalmic vein often drains into the superior ophthalmic vein before that larger vein leaves the orbit; however, sometimes the inferior ophthalmic vein drains directly into the cavernous sinus.
The central vein of the retina drains blood from the neural layer of the optic retina (Gr 7.41, 7.42, Table 7.6 Transverse Section [p. 647]; N90). It leaves the eyeball at the optic disc to enter the optic nerve with the central artery of the retina. The vein leaves the optic nerve and usually drains directly into the cavernous sinus. Occlusion of the central vein of the retina often results in slow, painless visual loss. See http://emedicine.medscape.com/article/1223746-overview
SUPERIOR APPROACH TO THE ORBIT
This dissection is performed on BOTH SIDES of the cadaver.
1. Strip the dura mater off the floor of the anterior cranial fossa. With a mallet and chisel, CAREFULLY chip away the orbital plate of the frontal bone. If you have a chisel with a wide blade, it may be easier to control if you use one corner of the blade. We also have rongeurs for removing thin plates of bone, but please use them carefully as they are relatively fragile and expensive.
2. Continue removing bone anteriorly to near where the orbital plate meets the vertical squamous portion of the frontal bone. DO NOT REMOVE THE ORBITAL MARGIN! Since the frontal sinus extends a variable distance backward into the orbital plate, you will probably break into the sinus. Notice the membranous mucoperiosteum that lines the sinus. If you go too far medially you will break into the ethmoidal air cells (ethmoidal sinus). Try to leave them intact as we will later be looking for structures that traverse the ethmoidal air cells. Insert a probe through the superior orbital fissure to protect the structures traversing it and remove the roof, which is formed by the lesser wing of the sphenoid bone.
3. The structures of the orbit will be enclosed within a sleeve of periorbita. Incise the periorbita longitudinally along the orbital axis. When your incision approaches the squamous part of the frontal bone, make medial and lateral transverse incisions from the front of the longitudinal incision. Reflect and remove the flaps of periorbita. You will have to carefully pick away orbital fat in a piecemeal manner to expose some of the structures described below.
4. Clean the frontal nerve passing forward in the middle of the orbit superior to the levator palpebrae superioris muscle. Follow it until it branches into a lateral supraorbital nerve and a medial supratrochlear nerve. Look for the supraorbital nerve dividing into medial and lateral branches. Laterally find the slender lacrimal nerve passing forward in the superior part of the orbit, above the lateral rectus muscle, toward the lacrimal gland. Look for the lacrimal gland in the upper anterolateral part of the orbit.
5. Clean the supraorbital and lacrimal arteries coursing anteriorly near the nerves of the same name. The supratrochlear artery is one of the terminal branches of the ophthalmic artery and may be difficult to find in the upper anteromedial corner of the orbit. Look for the usually tortuous superior ophthalmic vein passing posteriorly toward the superior orbital fissure.
6. Clean the superior oblique muscle located superiorly on the medial side of the orbit. Near its proximal attachment, identify the trochlear nerve entering the muscle’s upper surface. Realize that the superior oblique muscle passes forward to the region of the trochlear fovea (or trochlear spine) in the upper medial angle of the orbit, where its tendon recurs around a small piece of cartilage, the trochlea, suspended from the orbital margin by a sling of fibrous connective tissue.
7. Cut the frontal nerve near the apex of the orbit and reflect it forward. Clean the levator palpebrae superioris muscle as it passes forward from the apex of the orbit above the superior rectus muscle. The levator passes above the eyeball to insert into a fibrous plate in the upper eyelid, the superior tarsus. Clean the superior rectus muscle.
8. Cut the levator palpebrae superioris and superior rectus muscles near the middle of the orbit and reflect their anterior and posterior halves in those respective directions. Look for the superior branch of the oculomotor nerve piercing the posterior half of the superior rectus muscle or winding around its border to enter the levator palpebrae superioris.
9. Laterally in the orbit remove the fat inferior to the lacrimal nerve and artery to expose the lateral rectus muscle. Clean the abducent nerve coursing along the medial surface of the muscle before piercing it.
10. Carefully begin removing fat piecemeal from the middle of the orbit between the exposed lateral rectus and superior oblique muscles. Find the slender nasociliary nerve and ophthalmic artery crossing medially above the optic nerve. Attempt to clean the threadlike branches of the nasociliary nerve and the accompanying arteries. Three or four long ciliary nerves branch from the nasociliary nerve as it crosses the optic nerve. Attempt to preserve these and trace them to the posterior part of the eyeball. There are short and long posterior ciliary arteries. Attempt to find ciliary arteries, but don’t try to distinguish short from long.
11. Medial to the optic nerve find the posterior and anterior ethmoidal nerves and arteries passing between the superior oblique and medial rectus muscles to enter the posterior and anterior ethmoidal foramina, respectively. Be aware that both posterior and anterior ethmoidal nerves and arteries have a short course in the anterior cranial fossa and enter the upper part of the nasal cavity.
12. Find the infratrochlear nerve continuing forward from the anterior ethmoidal nerve. The infratrochlear and anterior ethmoidal nerves are the terminal branches of the nasociliary nerve. Note that the branching pattern of the terminal part of the ophthalmic artery differs from that of the nasociliary nerve. The artery ends in supratrochlearand dorsal nasal branches.
13. Lateral to the optic nerve, near the apex of the orbit, find where the nasociliary nerve gives off the small sensory root of the ciliary ganglion (N86). Clean the ciliary ganglion, which may be no larger than a pinhead, in the posterior interval between the optic nerve and lateral rectus muscle. If you have difficulty finding the ganglion, look for the inferior branch of the oculomotor nerve near the floor of the orbit and follow the motor (parasympathetic) root to the ganglion. The inferior branch of oculomotor has a relatively short course in the orbit before dividing into branches to the medial rectus, inferior rectus, and inferior oblique muscles. Don’t look for those branches.
14. Clean the slender short ciliary nerves passing forward from the ciliary ganglion lateral to the optic nerve to reach the posterior part of the sclera. If you are still having trouble finding the ciliary ganglion, attempt to trace the short ciliary nerves posteriorly from the eyeball to the ganglion.
15. Study the optic nerve. Be aware, but don’t attempt to demonstrate, that the cranial meninges and subarachnoid space continue from the middle cranial fossa to the back of the eyeball. The central artery of the retinapierces the underside of the optic nerve near the back of the eye and enters the eye through the optic disc.
16. At the apex of the orbit clean the common tendinous ring (anulus tendineus), from which the four rectus muscles take origin (N84). It surrounds the optic canal and part of the superior orbital fissure. For a point of reference, remember that the frontal, lacrimal, and trochlear nerves enter the orbit through the superior orbital fissure above the common tendinous ring (N86). The oculomotor, nasociliary, and abducent nerves enter the orbit through the part of the superior orbital fissure enclosed by the common tendinous ring.
ANTERIOR APPROACH TO THE ORBIT
17. ON ONE SIDE OF THE CADAVER an additional procedure will be performed on the orbit. From the front bluntly dissect through the palpebral portion of orbicularis oculi and the orbital septum to find the attachment of the levator palpebrae superioris into the superior tarsal plate of the upper eyelid (N81). At the superolateral part of the orbit, find the palpebral portion of the lacrimal gland descending into the upper eyelid (N82). Find the connection between the palpebral and orbital parts of the lacrimal gland. Remove the remainder of the upper and lower eyelids to expose the anterior portion of the eyeball and associated structures. Time doesn’t permit detailed study of the eyelids, but be aware that their structure has implications for pathology in the region.
18. Find the inferior oblique muscle taking origin from the anteromedial portion of the floor of the orbit. Follow it as it passes laterally and posteriorly inferior to the inferior rectus muscle. At the superomedial angle of the orbit, find the tendon of the superior oblique muscle as it hooks around the trochlea and descends posterolaterally to insert into the sclera.
19. Expose the lacrimal sac in the fossa for the lacrimal sac (N82). Open the lacrimal sac and insert a probe through it into the nasolacrimal duct, which drains into the inferior meatus of the nasal cavity.
DISARTICULATION OF THE SKULL
20. In order to study the pharynx and larynx and to bisect the head for exposure of the nasal and oral cavities, it is necessary to disarticulate the head from the cervical vertebral column and to pull the head and the attached cervical viscera forward. To do this we need to disarticulate the atlanto-occipital joints and cut the ligaments and muscles that attach the skull to the cervical spine.
21. BEGIN BY PLACING THE BODY IN A SUPINE POSITION. If the cervical sympathetic trunkshave not been dissected previously, clean them now (Gr 8.21, 8.24, Table 8.6 [p. 760]; N129). Place your hands behind the cervical viscera from opposite sides of the neck. Yours hand will meet behind the contents of the carotid sheaths (carotid artery, internal jugular vein, and vagus nerve), cervical sympathetic trunks, and the pharynx or esophagus. Your right and left hands should be in the retropharyngeal space located between the buccopharyngeal and prevertebral fasciae (Gr 8.18, 8.41A; N34, 63). Move your hands upward in the retropharyngeal space toward the base of the skull. Place a probe in the retropharyngeal space as close to the base of the skull as possible and leave it in place. This will pull the structures that traverse the jugular foramen forward and, hopefully, protect them during the disarticulation of the skull.
22. NOW PLACE THE CADAVER IN A SEATED POSITION so that you have exposure to the posterior aspect of the cervical vertebral column and the region of the posterior cranial fossa that was exposed by removal of the occipital wedge of bone. As close to the skull as possible cut any remaining muscles that attach the posterior parts of the head to the vertebral column (e.g., trapezius, longissimus capitis). The remaining sternocleidomastoid muscle attachments can remain intact.
23. You will hear more later about the following important structures to be cut, but a brief overview will be helpful now (Gr 4.38, 4.39; N22, 23). The cruciform (cruciate) ligament is formed by the transverse ligament of the atlas and superior and inferior bands of fibers extending from it to the occipital bone and body of the axis, respectively. Be aware that the transverse ligament of the atlas may undergo degenerative changes in rheumatoid arthritis and often is lax or missing in Down syndrome patients, posing a danger for fatal atlantoaxial subluxation if care isn’t taken examining this region in an affected patient. The apical ligament of the dens is a slender band of connective tissue attaching the apex of the dens to the anterior margin of the foramen magnum (N23). The alar ligaments are a strong, rounded cord on each side that attach the upper part of the dens to the medial side of the corresponding occipital condyle. They prevent excessive rotation at the atlantoaxial joints. The tectorial membrane is the superior continuation of the posterior longitudinal ligament and covers the cruciform ligament posteriorly (Gr 4.38D, 4.39; N23).
24. The anterior atlanto-occipital membrane connects the anterior arch of the atlas and the anterior margin of the foramen magnum.
25. The posterior arch of the atlas should still be intact (Gr 4.39A, 7.20; N19). Using it as a guide, insert a fresh, sharp scalpel horizontally into the interval between the anterior margin of foramen magnum and the anterior arch of the atlas. Cut the tissue in the anterior interval between the atlas and occipital bone from one atlanto-occipital joint to the other. This usually isn’t as easy as it sounds, and you may want to ask for an instructor’s help if you have difficulty making the cut. In making this cut, you will be going through the tectorial membrane, superior band of the cruciform ligament, apical ligament of the dens, right and left alar ligaments, anterior atlanto-occipital membrane, longus capitis, and rectus capitis anterior and rectus capitis lateralis muscles (N29).
26. Place the blade of a wide chisel against the posterior surface of an atlanto-occipital joint and tap it forcefully with a mallet. You will probably have to do this more than once. When the joint is entered or you have fractured the occipital condyle, pry the bones apart. Repeat this procedure on the other side.
27. Separate the head from the cervical spine and pull it and the cervical viscera forward. If you have difficulty doing this, turn the cadaver back to a supine position and replace the probe in the upper part of the retropharyngeal space with a scalpel. Use the scalpel to cut posteriorly between the atlas and the occipital bone. The longus capitis muscles may still be partly intact. In addition, two small muscles that join the bones on each side—rectus capitis anterior and rectus capitis lateralis—may not have been cut or torn. If you are having problems, ask for an instructor’s assistance. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.