Oral Cavity thru Laryngopharynx
During this period, the muscles entering the soft palate from above will be dissected. Then the oral cavity and oropharynx will be studied. Finally, the laryngopharynx and larynx will be dissected.
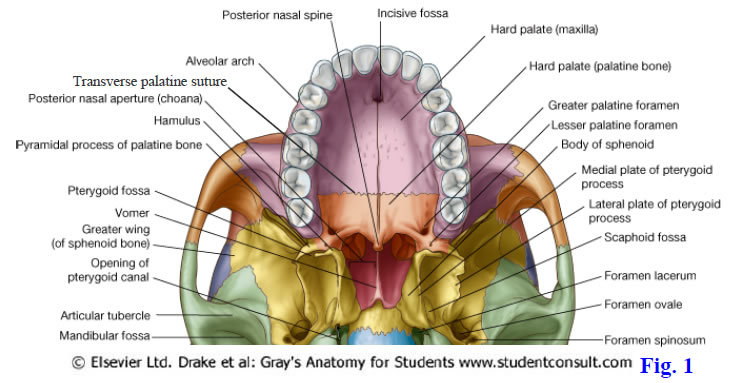
The palate separates the nasal cavity and nasopharynx above from the oral cavity and oropharynx below. It consists of the bony hard palate in its anterior 2/3 and the musculofibrous soft palate in its posterior 1/3 (Gr 7.57, 7.76; N36, 48, 63). The hard palate is formed by the palatine processes of the maxillae and the horizontal plates of the palatine bones, which meet at the transverse palatine suture (palatomaxillary suture) (Fig. 1; N10, 37, 56). Features of the hard palate include an anterior midline incisive fossa and posterolateral greater and lesser palatine foramina. The incisive fossa is a depression containing the openings of paired incisive canals connecting the nasal and oral cavities. Each greater palatine foramen is medial to a maxillary 3rd molar tooth, if the tooth is present. The smaller lesser palatine foramina pierce the pyramidal processes of the palatine bones.
The greater palatine nerve and vessels emerge onto the oral surface of the palate at the greater palatine foramen and run anteriorly to supply the mucoperiosteum of the hard palate (Gr 7.57D, 7,64; N39-42, 52). The greater palatine artery continues superiorly through an incisive canal to reach the anterior nasal septum (Gr 7.65; N39, 40 [in these two figures ignore the label “Anastomosis in incisive canal” since the artery in the incisive canal is the greater palatine ascending into the nasal cavity]). Passing downward through an incisive canal is the nasopalatine nerve, which supplies the palate between the incisive fossa and maxillary incisor teeth (N42). The lesser palatine nerve and vessels pass posteriorly from the lesser palatine foramina to supply the soft palate.
The soft palate is suspended from the posterior border of the hard palate (Gr 7.57C-D, 8.41A, Table 7.12 [p. 674]; N38, 52, 63, 66). It has a posterior free margin with a conical midline process, the uvula. The soft palate consists of a thin, fibrous palatine aponeurosis covered by attached muscles and mucous membrane. The palatine aponeurosis gives the soft palate flexible support so that it can be depressed to help close the opening between the oral cavity and oropharynx (oropharyngeal isthmus) or elevated and tensed against the posterior pharyngeal wall during swallowing to prevent food or drink from passing superiorly into the nasopharynx.
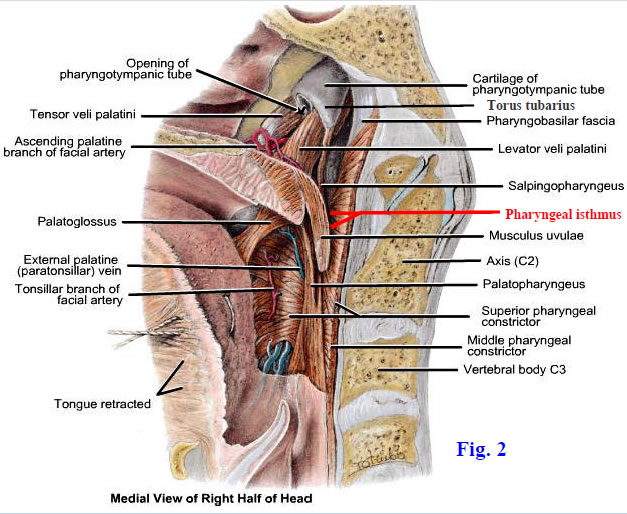
There are five pairs of muscles in the soft palate (Gr 8.32C-D, Table 7.12 [p. 674]; N52, 64-67). Two pairs of muscles descend from the cranial base into the palate and can raise it, two pairs ascend into the soft palate from the tongue or pharynx and can depress it, and one pair passes posteriorly into the uvula from the hard palate to control the uvula’s shape and movements. The levator veli palatini and tensor veli palatini descend into the soft palate (Fig. 2). The levator arises from the petrous portion of the temporal bone and cartilage of the pharyngotympanic (auditory) tube. It raises a ridge of mucous membrane (torus levatorius) as it passes medially into the soft palate and spreads across the superior surface of the palatine aponeurosis (Gr 8.32A-B; N66, 67). Fibers of the levator veli palatini interdigitate with those of the opposite side, which helps the pair of muscles elevate the soft palate into contact with the posterior pharyngeal wall during swallowing.
The tensor veli palatini is located anterior and lateral to the levator veli palatini (Gr 8.32C-D & F; N52 [Posterior view], 64, 65, 68). The tensor descends lateral to the medial pterygoid plate from attachments at the scaphoid fossa, spine of the sphenoid bone, and pharyngotympanic tube cartilage. The tensor veli palatini’s tendon makes a 90° turn around the pterygoid hamulus to pass medially into the soft palate, reinforcing (some authors say forming) the palatine aponeurosis and meeting the tendon of the other side (N52). The tensor veli palatini muscles tense the soft palate during swallowing to prevent the bolus of food from pushing it upward into the nasopharynx.
The tensor veli palatini, through its attachment to the pharyngotympanic tube cartilage, can open the pharyngotympanic tube, which is closed in the resting state. This allows an equalization of pressure between the tympanic cavity and the outside (e.g., swallowing during an airplane’s ascent to cruising altitude). The levator veli palatini also may function in opening the auditory tube. The tensor veli palatini is innervated by the mandibular division of the trigeminal nerve (V3), making it the only muscle of the soft palate that isn’t innervated by the vagus nerve (X) via the pharyngeal plexus.
Two pairs of muscles that ascend into the soft palate are the palatoglossus and palatopharyngeus muscles (Gr 8.30, 8.31C, 8.32C-D, Table 7.12 [p. 674]; N52, 59, 64). The slender palatoglossus muscle passes from the side of the tongue up into the palate. It raises a fold of mucous membrane, the palatoglossal arch, which is the boundary between the oral cavity and oropharynx (N64). The palatoglossal arch is also the anterior boundary of the bed of the palatine tonsil (tonsillar fossa).
The larger palatopharyngeus muscle passes between the soft palate and the posterior pharyngeal wall (N65, 67). Its inferior fibers spread from the posterior border of the thyroid cartilage as far posteriorly as the midline pharyngeal raphe. The palatopharyngeus is the core of the palatopharyngeal fold, which forms the posterior boundary of the tonsillar fossa (N64).
The musculus uvulae is a small paired muscle extending from the posterior nasal spine into the uvula (Fig. 2; Gr Table 7.12 [p. 674]; N52, 67). It shortens and elevates the uvula, helping to close the pharyngeal isthmus, which is the gap between the posterior free border of the soft palate and the pharyngeal wall, during swallowing.
The muscles of the soft palate, except the tensor veli palatini, are innervated by the vagus nerve (CN X) through the pharyngeal plexus. The tensor veli palatini develops from the first pharyngeal arch and is innervated by the mandibular nerve (V3). Elevation of the soft palate into contact with the posterior pharyngeal wall, closing the pharyngeal isthmus, is essential both for swallowing and for normal speech. One of the more significant difficulties following cleft palate repair (palatoplasty) is establishing satisfactory speech ( http://www.emedicine.com/plastic/topic519.htm).
Sensory innervation of the hard palate is by the greater palatine nerves posterior to the incisive fossa (Fig. 3; Gr 7.57C-D, 7.64, 7.70B, 8.30A, 8.31; N41, 42, 52, 62). Anterior to the incisive fossa the palate is innervated by the nasopalatine nerves, which descend through incisive canals from the nasal cavities. The soft palate receives its sensory innervation from the lesser palatine nerves.
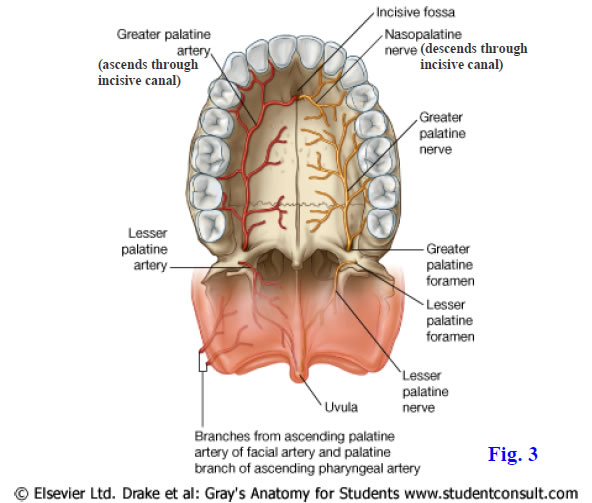
The blood supply of the hard palate is mainly from the greater palatine arteries (Fig. 3; Gr 7.57C-D, 8.30A; N39, 40, 52). These arteries pass forward from the greater palatine foramina and ascend through the incisive canals to reach the anterior inferior portion of the nasal septum. The soft palate is supplied by the lesser palatine arteries, ascending palatine branches of the facial arteries, and palatine branches of the ascending pharyngeal arteries (N64, 69).
1. Identify the torus tubarius and the opening of the auditory tube in the nasopharynx (Fig. 2). Find the salpingopharyngeal fold descending posteriorly from the torus tubarius. Carefully remove the fold’s mucous membrane to expose the delicate salpingopharyngeus muscle. Note the mucosal ridge extending into the soft palate from just below the opening of the auditory tube. This ridge is the torus levatorius overlying the levator veli palatini muscle. Remove the mucous membrane overlying the levator veli palatini.
2. Anterior and lateral to the levator veli palatini, remove the mucous membrane and a variable amount of loose connective tissue to find the tensor veli palatini. If you have difficulty finding the tensor, remember that you should be looking just posterior to the medial pterygoid plate, which in turn is just posterior to the pterygopalatine fossa that was opened in a previous dissection. Verify that the tendon of the tensor veli palatini hooks around the hamulus of the medial pterygoid plate, changing direction 90° to enter the soft palate almost horizontally. Look for the small ascending palatine branch of the facial artery between the upper parts of the levator and tensor veli palatini muscles (Fig. 2). XXX
The oropharynx lies posterior to the oral cavity, bounded by the soft palate above and the tip of the epiglottis below (Gr 8.29, 8.30, 8.32A-C, 8.41; N63, 66). It is normally digestive in function but may also function in breathing if the nasal cavity or nasopharynx is obstructed. The oropharynx communicates anteriorly with the oral cavity at the oropharyngeal isthmus formed by the two palatoglossal arches. Each palatoglossal arch is a fold formed by mucous membrane covering the slender palatoglossus muscle of its side (Figs. 2, 4; N64). The palatoglossus muscle has been classified by different authors both as a muscle of the soft palate and a muscle of the tongue, but its innervation from the vagus nerve through the pharyngeal plexus supports its inclusion as a palatal muscle.
Another set of mucosal folds raised over muscles in the lateral wall of the oropharynx are the palatopharyngeal arches (Gr 8.30, 8.31, 8.32A-C; N58, 60 [Horizontal section], 64, 66, 67). The palatopharyngeal arch is separated from the more anterior palatoglossal arch by the shallow bed of the palatine tonsil (tonsillar fossa). The palatoglossal and palatopharyngeal arches together are the pillars of the fauces (fauces = throat). The palatopharyngeal muscles have already been discussed with the longitudinal muscles of the pharynx.
The tonsillar fossa is the location of the palatine tonsil in children and young adults (Gr 8.30, 8.31, 8.32A-D; N60, 63, 64). The palatine tonsils are usually atrophied and unrecognizable in the elderly. Each palatine tonsil is a mass of lymphoid tissue with a surface epithelium covered with pits, the tonsillar crypts. The palatine tonsils frequently must be surgically removed (tonsillectomy) in children due to recurrent tonsillitis. The condition is so common that the jugulodigastric lymph node, which receives lymph from the palatine tonsil, is the most frequently enlarged lymph node in the body and is called the “tonsillar node” (Gr 7.88B; N72, 73).
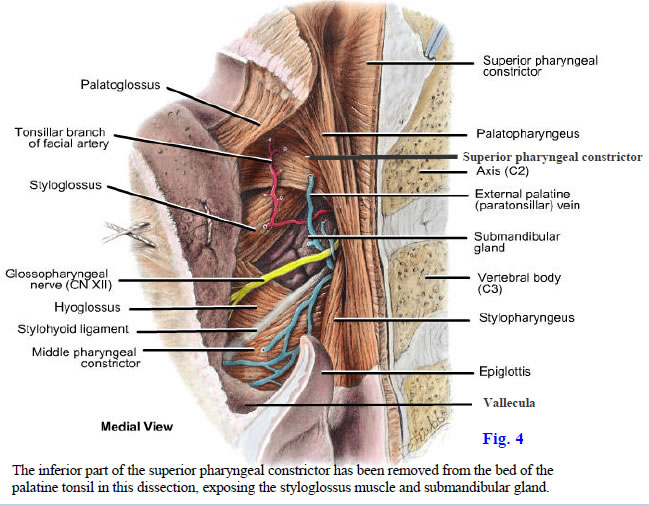
The lateral relationships of the palatine tonsil are clinically important (Fig. 4; Gr 8.32B-E; N64). The deep surface of the tonsil has a capsule formed by pharyngobasilar fascia. The capsule is normally separated from the superior pharyngeal constrictor muscle (Figs. 2, 4; Gr 8.32C; N64, 65) by loose connective tissue of the peritonsillar space. This loose connective tissue is commonly a site of abscess formation (peritonsillar abscess or quinsy), which may result in airway obstruction or aspiration pneumonia, among other complications ( http://www.emedicine.com/emerg/topic417.htm ). The loose connective tissue also forms a cleavage plane that facilitates surgical removal of the tonsil. Following chronic tonsillitis, however, the capsule may adhere to the superior constrictor muscle, making removal of the tonsil more difficult.
The blood vessels in the bed of the palatine tonsil can be a troublesome source of bleeding during tonsillectomy ( http://www.emedicine.com/ent/topic315.htm ). The largest artery and usual source of arterial bleeding is the tonsillar branch of the facial artery (Fig. 4; Gr 8.32B-E; N64, 69), but branches from other small arteries are also present. The paratonsillar (external palatine) vein also may hemorrhage (Gr. 8.32C; N70). Importantly, the internal carotid artery is sometimes tortuous with a loop located just lateral to the superior pharyngeal constrictor muscle, where the artery can be injured with fatal results if the muscle is penetrated during surgery.
The glossopharyngeal nerve is also in jeopardy during palatine tonsillectomy (Fig. 4; Gr 8.28A, 8.32E; N64). The nerve traverses the gap between the superior and middle pharyngeal constrictor muscles with the stylopharyngeus muscle. It crosses the lower pole of the tonsil en route to the mucosa of the posterior third of the tongue. The glossopharyngeal nerve may become temporarily nonfunctional due to edema following surgery, resulting in diminished taste, or it may be permanently damaged by a surgical instrument.
The oropharyngeal portion (posterior 1/3) of the tongue has an irregular surface due to the presence of multiple lymphoid follicles of the lingual tonsil (Gr 7.52A, 7.54A, 8.29, 8.32A; N 58, 64, 66). Along with the palatine and pharyngeal tonsils, the lingual tonsil forms the tonsillar ring (of Waldeyer) around the superior portion of the pharynx. The tonsillar ring of lymphatic tissue may provide limited protection against the entrance of infection into the respiratory and digestive systems.
Behind the tongue, between it and the epiglottis, is a midline mucosal fold, the median glossoepiglottic fold. On either side of the median glossoepiglottic fold is a shallow depression, the vallecula, where foreign objects may lodge (Gr 7.54B, 8.40B; N58).3. Identify the palatoglossal and palatopharyngeal arches descending from the inferior surface of the soft palate. Note that the palatoglossal arch reaches the tongue near the sulcus terminalis, while the palatopharyngeal arch descends posterior to the tongue and blends into the posterior pharyngeal wall. Carefully incise and remove the mucous membrane of these arches to expose the underlying palatoglossus and palatopharyngeus muscles.
4. Study the bed of the palatine tonsil (tonsillar fossa). Usually the palatine tonsil is atrophied and unidentifiable in the elderly. If a remnant of the tonsil is present, examine its exposed surface for the presence of tonsillar crypts. Remove the mucosa of the tonsillar bed and attempt to find the tonsillar branch of the facial artery (Figs. 2, 4). Clean the glossopharyngeal nerve as it crosses the lower part of the tonsillar fossa to reach the posterior 1/3 of the tongue. You can confirm the identity of the glossopharyngeal nerve by returning to a posterior view of the stylopharyngeus muscle entering the pharyngeal wall and gently tugging on the nerve as it descends in a curve posterior, then lateral, to the muscle. Don’t confuse the glossopharyngeal nerve with the stylohyoid ligament, which traverses the lower part of the tonsillar bed en route to the lesser horn of the hyoid bone and has middle pharyngeal constrictor muscle fibers attached to it (Fig. 4; N64, 65). If in doubt, palpate the lesser horn of the hyoid bone and follow the ligament to it. Confirm that the muscular bed of the palatine tonsil is formed mainly by the superior pharyngeal constrictor muscle (Fig. 2). XXX
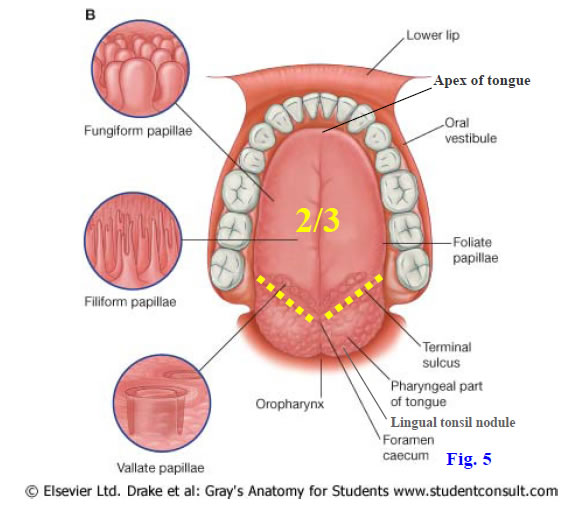
The oral cavity consists of the vestibule and the oral cavity proper (Gr 7.53). The vestibule is the narrow space separating the lips and cheeks externally from the teeth and gums internally (Fig. 5). The oral cavity proper is located internal to the maxillary and mandibular alveolar arches and teeth. The roof of the oral cavity proper is formed by the palate, and its floor is formed by the tongue and a U-shaped sublingual sulcus below the tip and lateral edges of the tongue. The palate has already been described. The tongue is a muscular organ involved in mastication and taste, swallowing, and speech. It is divided into an anterior 2/3 and a posterior 1/3 by a V-shaped groove on its dorsal surface, the terminal sulcus (sulcus terminalis) (Fig. 5; Gr 7.52A, 8.29A; N58). A small pit may be present at the angle of the V, the foramen cecum (N63), indicating the embryonic site of origin of the thyroid gland.
The anterior 2/3 of the tongue is located in the oral cavity and is the body of the tongue. It has an anterior tip, or apex (Fig. 5, 6; N58, 63). The body and apex of the tongue are highly mobile and can be protruded (sticking out the tongue) or rolled posteriorly against the palate to push a bolus of food into the oropharynx during swallowing ( http://www.emedicine.com/pmr/topic152.htm ). The inferior surface of the tip of the tongue is connected to the floor of the oral cavity by a midline fold of mucous membrane, the lingual frenulum (Gr 7.55A; N51). An abnormally short lingual frenulum limits movement of the tongue (ankyloglossia) and may have to be surgically released. The posterior 1/3 of the tongue lies in the oropharynx and is the root of the tongue.
The anterior 2/3 of the tongue is covered by mucous membrane derived from oral ectoderm. Because it develops from ectoderm of the first pharyngeal arch, the general innervation of this mucosa is by general sensory afferent (GSA) nerve fibers of the lingual nerve (V3) (Gr 7.52B; N62). The mucous membrane has a rough texture because it is covered by numerous small lingual papillae (Fig. 5; Gr 7.52A-B; N58). Of the four types of lingual papillae—filiform, fungiform, foliate, and vallate—all but the first contain taste buds. The most numerous are the microscopic filiform papillae, but the most important in humans are the fungiform and vallate papillae. As the name suggests, the fungiform papillae are mushroom-shaped. They appear as scattered small pink or red spots on the dorsum of the tongue. The vallate (circumvallate) papillae are arranged in a row of 8-12 papillae just anterior to the terminal sulcus. They are the largest of the lingual papillae—sometimes nearly the size of a pencil eraser—and contain abundant taste buds. The foliate papillae along the sides of the tongue are poorly developed in humans.
The posterior 1/3 of the tongue is covered by mucous membrane derived from pharyngeal endoderm, mainly from the third pharyngeal arch. Therefore, its general sensation is from general visceral afferent (GVA) nerve fibers of the glossopharyngeal nerve (IX). The mucosal surface is irregular due to the presence of follicles of submucosal lymphoid tissue, the lingual tonsil. The lingual tonsil joins the palatine tonsils and pharyngeal tonsil in forming a tonsillar ring of lymphatic tissue at the beginning of the respiratory and digestive systems.
Taste is carried from sensory receptor cells in taste buds, most of which are associated with lingual papillae (Gr 7.52A-B; N58). In addition, small numbers of taste buds are present on the epiglottis and soft palate. The taste (special visceral afferent, SVA) fibers to the anterior 2/3 of the tongue are carried by the chorda tympani, a branch of the facial nerve (VII) that joins the lingual nerve (V3) in the infratemporal fossa (Gr 7.47B, 7.49A, Table 9.9 [p. 813]; N45, 62, 121, 122). The lingual nerve carries general (GSA) sensation from the anterior 2/3 of the tongue. The cell bodies of SVA neurons in the chorda tympani are in the geniculate ganglion and those of the GSA neurons in the lingual nerve are in the trigeminal ganglion.
Both taste (SVA) and general (GVA) sensation from the posterior 1/3 of the tongue are carried by the glossopharyngeal nerve (IX) (Gr 7.52B, 8.32E, Table 9.11 [p. 817]; N62, 124). This includes taste from the vallate papillae, even though they lie slightly anterior to the sulcus terminalis. The limited taste sensation from the epiglottis is carried by the internal laryngeal nerve (X) and that from the soft palate near the palatine tonsil by a few SVA fibers of VII traveling with the lesser palatine nerves (V2). The SVA fibers in the lesser palatine nerves reach them via the greater petrosal nerves and traverse the pterygopalatine ganglion (of course without synapsing). We will ignore the few taste fibers from the soft palate.
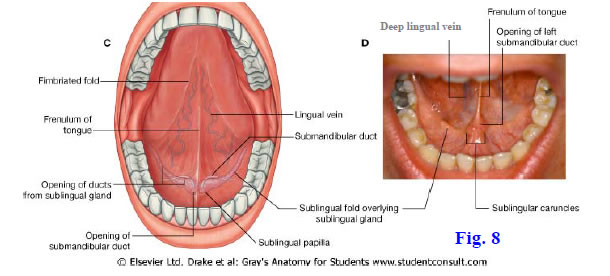
The inferior surface of the tongue has a thin, translucent mucous membrane, through which submucosal veins can be seen in a living person (Fig. 8; Gr 7.55A; N51). A deep lingual vein is visible through the mucous membrane on each side of the frenulum. The thin mucosal barrier allows the rapid sublingual absorption of drugs (e.g., nitroglycerin) into the bloodstream via the deep lingual veins.
5. Study the surface features of the dorsum of the tongue. Identify the V-shaped sulcus terminalis. Look for the foramen cecum, which may be absent, at the apex of the V. Find the scattered fungiform papillae on the oral surface of the tongue. Locate the large vallate papillae just anterior and parallel to the sulcus terminalis (Fig. 5). XXX
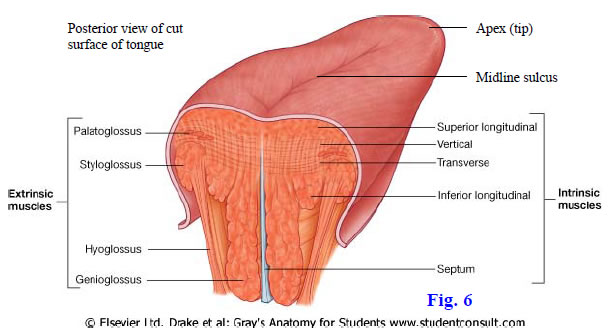
The tongue consists mainly of skeletal muscle and consists of two halves separated by a median fibrous septum (Fig. 6). It has both intrinsic muscles contained entirely within the tongue and extrinsic muscles that originate outside the tongue and pass into it (Figs. 6, 7; Gr Table 7.11 [p. 667]; N59, 60). In general, the intrinsic muscles change the shape of the tongue, and the extrinsic muscles move the tongue. The intrinsic muscles consist of longitudinal, transverse, and vertical fibers. It’s important to be aware of the presence of the intrinsic muscles, but they won’t be dissected. The muscles of the tongue are innervated by GSE fibers of the hypoglossal nerve (XII).
The extrinsic muscles of the tongue are the genioglossus, hyoglossus, and styloglossus (Figs. 6, 7; Gr 7.54A, 8.41, Table 7.11 [p. 667]; N59). The palatoglossus is better considered a muscle of the soft palate, with which it shares innervation. The genioglossus muscle is a fan-shaped muscle that takes origin from the superior mental spine (genial tubercle). The must anterior fibers curve upward into the tip of the tongue, and a few of the most posterior fibers pass posteriorly and slightly inferiorly to attach into the hyoid bone above the geniohyoid muscle. The intermediate fibers of the genioglossus fan out between the anterior vertical and posterior horizontal fibers. The genioglossus muscles protrude the tongue.
Lateral to the genioglossus muscles are the hyoglossus and styloglossus muscles (Figs. 6, 7; Gr 8.13A, 8.14B, Tables 7.11 [p. 667], 8.7 [p. 766]; N59, 60, 127). The thin, quadrilateral hyoglossus passes superiorly into the tongue from the body and greater horn of the hyoid bone. The hyoglossus muscle is a useful landmark during dissection since the lingual and hypoglossal nerves pass lateral to it and the lingual artery passes medial to it. The two hyoglossus muscles depress the tongue.
Each styloglossus muscle descends anteriorly into the tongue from the styloid process of the temporal bone (Fig. 7; Gr 8.13A-B; N59, 68). Its fibers interdigitate with the posterior superior fibers of the hyoglossus muscle. Contraction of the styloglossus muscles pulls the tongue posteriorly and superiorly.
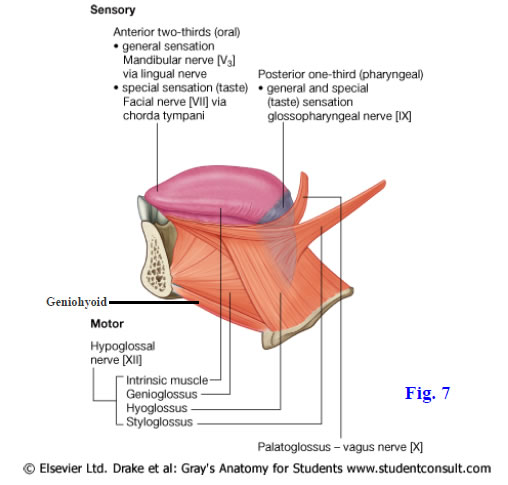
The intrinsic and extrinsic muscles of the tongue, except palatoglossus (X) if it is included as a tongue muscle, are innervated by the hypoglossal nerve (XII) (Fig. 7; Gr 8.12, 8.13A, Table 9.14 [p. 821]; N59, 71, 127). The hypoglossal nerve exits the posterior cranial fossa through the hypoglossal canal and descends in close relation to the upper part of the vagus nerve. It loops forward below the angle of the mandible and ascends deep to the posterior belly of the digastric muscle to enter the submandibular triangle. The hypoglossal disappears into the floor of the oral cavity between the mylohyoid and hyoglossus muscles. The hypoglossal nerve’s position lateral (superficial)to the hyoglossus muscle makes it easier to find during dissection of the floor of the oral cavity.
A unilateral lesion of the hypoglossal nerve results in deviation of the protruded tongue toward the paralyzed side. In an unconscious supine person, relaxation of the genioglossus muscles allows the tongue to fall posteriorly, obstructing the airway. Thus the jaw thrust maneuver is performed to pull the mandible, and with it the tongue, anteriorly; however, special care must be taken if a cervical spine injury is suspected.
The major blood supply to the tongue is from the lingual artery, which branches from the external carotid artery in the carotid triangle (Gr 7.54B, 7.56B, 8.13A-B, 8.14B; N33, 59). The lingual artery may branch from a common faciolingual stem with the facial artery. The lingual artery ascends anteriorly above the hyoid bone and passes medial (deep) to the hyoglossus muscle. The artery is divided into three parts in relation to the hyoglossus—posterior to it, deep to it, and anterior to it (Gr 8.14B; N59). The second part, which is deep to the muscle, gives off a couple of dorsal lingual arteries to the oropharyngeal portion of the tongue. As the third part of the lingual artery emerges anterior to the hyoglossus, it divides into deep lingual and sublingual arteries. The deep lingual artery runs forward on the inferior surface of the tongue to the apex. The sublingual artery continues forward below the mucosa of the sublingual sulcus to supply the sublingual gland and other structures in the floor of the oral cavity.
The venous drainage of the tongue diverges slightly from the arterial supply. The deep lingual vein (Fig. 8; Gr 7.55A, 8.14A) joins the sublingual vein to accompany the hypoglossal nerve lateral (superficial)to the hyoglossus muscle. As mentioned above, the deep lingual veins provide a convenient route for the rapid absorption of drugs placed under the tongue. Dorsal lingual veins travel with the dorsal lingual arteries deep to the hyoglossus and drain into the lingual vein posterior to the muscle. The lingual vein is a tributary of the internal jugular vein.
The floor of the oral cavity below the sides and tip of the tongue forms the U-shaped sublingual sulcus (Fig. 8; Gr 8.14A; N51, 61). A small ridge of mucous membrane in the sublingual sulcus on each side of the frenulum is the sublingual fold overlying the sublingual gland, which is the smallest of the three major salivary glands. A series of minor sublingual ducts usually opens through the mucosa of the sublingual fold (Gr 8.12; N51, 61). Each sublingual fold terminates anteriorly at the base of the lingual frenulum in a slight elevation, the sublingual caruncle (sublingual papilla). The duct of the submandibular gland opens on the sublingual papilla.
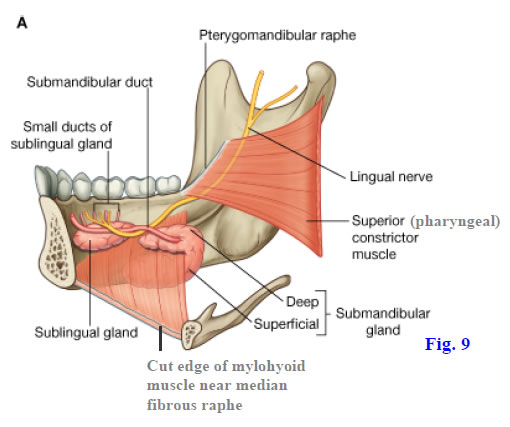
The sublingual gland is located deep to the mucous membrane of the sublingual fold (Gr 7.55, 7.76, 8.12; N61). The gland is flattened mediolaterally between the mandible and the muscles of the tongue. The submandibular duct leaves the small deep part of the submandibular gland and ascends across the medial surface of the sublingual gland (Fig. 9; Gr 7.55B; N53, 61) to reach and open on the sublingual caruncle. The larger superficial part of the submandibular gland was seen in the submandibular triangle (Gr 7.45, 8.8; N26, 30). There are superficial and deep parts of the submandibular gland because the C-shaped gland curves around the posterior border of the mylohyoid muscle (N61).
The lingual nerve (V3) was seen previously in the infratemporal fossa dissection, where it was joined by the chorda tympani branch of the facial nerve (VII) (Gr 7.47B, 7.49A; N45, 71). After crossing the lateral surface of the medial pterygoid muscle, the lingual nerve enters the floor of the oral cavity inferomedial to the mandibular third molar tooth (Gr 7.55B, 8.12, 8.13; N45, 53). The nerve loops anteromedially through the floor of the oral cavity under the submandibular duct, which is a useful landmark (Fig. 9). Near the lingual nerve’s entrance into the oral cavity, the submandibular ganglion is suspended from it by two or more ganglionic branches. The ganglion is discussed below. The lingual nerve carries general sensation from the anterior 2/3 of the tongue (Gr 7.52B; N62). The chorda tympani carries taste sensation from the anterior 2/3 of the tongue.
The submandibular ganglia are one of the four pairs of parasympathetic ganglia in the head (Gr 8.12, 8.13, Table 9.13 [p. 822]; N130, 132). Preganglionic parasympathetic nerve fibers reach the submandibular ganglion via the chorda tympani and lingual nerves to synapse on the cell bodies of postganglionic parasympathetic neurons within the ganglion. Postganglionic parasympathetic nerve fibers leave the ganglion in one of two ways. Some axons enter branches of the ganglion that pass directly to the deep portion of the submandibular gland. Other fibers re-enter the lingual nerve and travel in it to the sublingual gland and some minor salivary glands.
Two additional pairs of muscles in the floor of the oral cavity—the mylohyoid and geniohyoid—help to support the tongue (Gr 8.11, 8.12, 8.13A, 8.15, 8.41, Table 8.5 [p. 740]; N53, 59, 63). The mylohyoid muscles were seen from below when the suprahyoid region was dissected. The muscles of the two sides arise from the mylohyoid lines of the mandible and descend medially (Fig. 9). Their posterior fibers attach to the hyoid bone but the middle and anterior fibers meet in a median fibrous raphe to form the muscular floor of the oral cavity. The submandibular gland wraps around the posterior free border of the mylohyoid muscle, an arrangement that divides the gland into superficial and deep parts (Fig. 9). The mylohyoid muscle is innervated by the nerve to the mylohyoid, which is a branch of the inferior alveolar nerve (V3) (Gr 7.47, 8.9, 8.11; N45, 71).
The geniohyoid muscle passes from the inferior mental spine (genial tubercle) to the hyoid bone (Fig. 7; Gr 8.13, 8.15B, 8.41; N53, 59, 63). The geniohyoid is separated by fascial planes from the genioglossus muscle above and the mylohyoid muscle below. It is innervated by the nerve to the geniohyoid (anterior ramus of C1), which travels with the hypoglossal nerve (N128).
BISECTING THE TONGUE AND MANDIBLE, FLOOR OF THE ORAL CAVITY
6. The tongue and floor of the oral cavity are more easily studied following bisection of the tongue and mandible. Use a sharp scalpel to bisect the lower lip in the midline. Saw through the mandible between the two medial incisor teeth, or as close to the midline as possible if the cadaver is edentulous. Use the scalpel to bisect the tongue and floor of the oral cavity in the midline as far posteriorly as the epiglottis and as far inferiorly as the hyoid bone. DO NOT CUT THE EPIGLOTTIS!
7. On the medial, cut surface of the tongue and floor of the oral cavity, identify the genioglossus muscle fanning out into the tongue from the superior mental spine. Note that its lowest fibers insert into the hyoid bone. In some cadavers there may not be distinct superior and inferior mental spines, but rather a single bony projection for muscle attachments. Clean the geniohyoid muscle passing from the inferior mental spine to the hyoid bone. Below the geniohyoid find the thin cut edge of the mylohoid muscle. If the tissue isn’t too desiccated, there are usually clear fascial intervals separating the geniohyoid from the muscles above and below it. Note the anterior belly of the digastric muscle, which was seen earlier inferior to the mylohyoid muscle. The digastric is classified as a suprahyoid muscle and an accessory muscle of mastication.
8. Displace the half-tongue medially to expose the sublingual sulcus below its lateral edge. Identify the sublingual fold as a slight longitudinal ridge in the sublingual sulcus. The fold ends anteriorly at the base of the lingual frenulum in a slight elevation, the sublingual caruncle. Examine the caruncle for the opening of the submandibular duct. This may be seen more easily on a live classmate or in one’s own oral cavity by shining a flashlight while looking in a mirror.
9. Carefully incise and remove the mucous membrane of the sublingual sulcus. Clean the sublingual gland located anteriorly between the tongue and mandible. Medial to the sublingual gland find the terminal portion of the submandibular duct (Fig. 9). Trace the submandibular duct posteriorly and inferiorly to the deep part of the submandibular gland.
10. Locate the lingual nerve as it loops under the submandibular duct from lateral to medial (Fig. 9). Alternatively, probe for the termination of the nerve between the tongue and sublingual gland and follow the nerve posteriorly under the submandibular duct to a point below the last mandibular molar tooth. Find the submandibular ganglion suspended from the lingual nerve near the third molar. Instead of two or more branches suspending a rounded, clearly defined ganglion (Gr 8.12), the ganglion may appear as a single mass of tissue hanging from the lingual nerve. If that’s the case, the ganglion can usually be identified by slender branches leaving it to enter the deep part of the submandibular gland.11. Further inferiorly in the same fascial plane as the lingual nerve look for the hypoglossal nerve. If you have difficulty finding the hypoglossal nerve in the floor of the oral cavity, re-position the head and neck for a lateral view and again identify the hypoglossal nerve in the carotid triangle. Trace it deep to the posterior belly of the digastric muscle into the submandibular triangle and clamp the nerve as it disappears between the mylohyoid and hyoglossus muscles. Now identify the nerve from a superior view, through the floor of the oral cavity.
12. Clean the fascia from the hyoglossus muscle, which lies medial to the lingual and hypoglossal nerves. Note the vertical orientation of the muscle fascicles. Find fascicles of the styloglossus muscle descending anteriorly from the styloid process of the temporal bone to interdigitate with the posterior superior portion of the hyoglossus (Fig 7).
13. The lingual artery runs medial, or deep, to the hyoglossus muscle. Look for the third part of the lingual artery emerging from deep to the hyoglossus muscle at its anterior border. Attempt to find the terminal branching of the lingual artery into the deep lingual artery, which ascends into the apex of the tongue, and the sublingual artery to the floor of the oral cavity. If an instructor directs that you also look for the dorsal lingual arteries on one side of the tongue, the hyoglossus muscle will have to be carefully transected. It is probably easiest to do this using small, sharp-pointed scissors to cut posteriorly superficial to the path of the lingual artery starting at the anterior border of the hyoglossus muscle. Note that the deep and sublingual veins join to accompany the hypoglossal nerve lateral to the hyoglossus muscle, but don’t attempt to preserve these veins. Dorsal lingual veins descend deep to the hyoglossus muscles. XXX
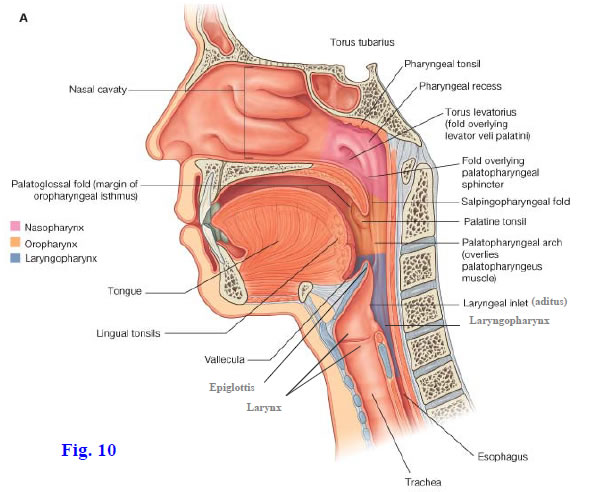
The laryngeal part of the pharynx, or laryngopharynx (formerly called the “hypopharynx”), extends from the superior border of the epiglottis to the inferior border of the cricoid cartilage (Fig. 10; Gr 8.29, 8.40B, 8.41; N63, 66 [Note: neither one of these Netter images actually marks the boundaries of the laryngopharynx correctly). The laryngopharynx is continuous with the esophagus below and lies behind the aditus (inlet) and posterior wall of the larynx. Thus the laryngeal part of the pharynx is both respiratory and digestive in function. The aditus of the larynx is formed by the superior border of the epiglottis, aryepiglottic folds, arytenoid cartilages, and interarytenoid fold and will be studied in more detail with the larynx.
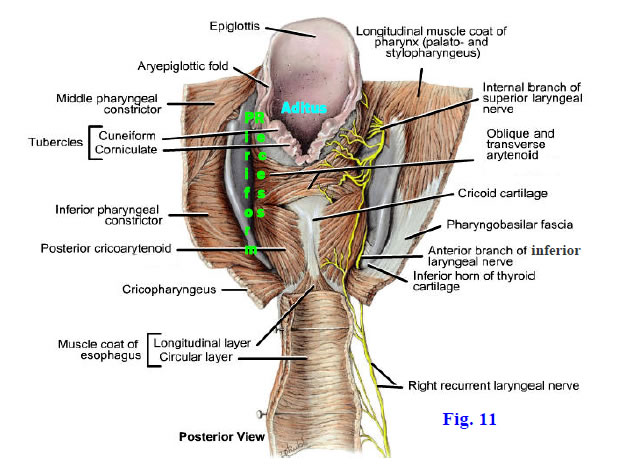
A longitudinal depression lateral to the inlet and lateral wall of the larynx on each side, between it and the lamina of the thyroid cartilage, is the piriform recess (piriform fossa) (Fig. 11; Gr 8.29A; N66). During swallowing, the bolus of food or stream of liquid is directed to the sides of the epiglottis and into the piriform recesses. Nerves and small arteries traverse the piriform recess subjacent to its mucous membrane. The internal laryngeal nerve was seen previously piercing the thyrohyoid membrane in company with the superior laryngeal artery to enter the recess (Fig. 11; Gr 8.16E, 8.38A, Table 8.8 [pp. 784-785]; N69, 71, 74). The internal laryngeal nerve arises from the superior laryngeal branch of the vagus nerve (X). The inferior laryngeal nerve ascends just posterior to the cricothyroid joint to enter the piriform recess with the inferior laryngeal artery (N80). “Inferior laryngeal nerve” is the correct term for the continuation of the recurrent laryngeal nerve (X) once it ascends deep to the inferior border of the inferior pharyngeal constrictor muscle, but this part of the nerve often is still referred to as the “recurrent laryngeal nerve.”
The superior laryngeal artery is a small branch of the superior thyroid artery and enters the piriform fossa with the internal laryngeal nerve (Gr 8.16E; N69, 74). The inferior laryngeal artery branches from the inferior thyroid artery. It ascends through the lower part of the piriform recess with the inferior laryngeal nerve.
The relationships of the piriform recess are clinically important because swallowed objects (e.g., a chicken bone) may become lodged there and damage the internal laryngeal or inferior laryngeal nerve. These nerves lie just deep to the mucous membrane of the upper and lower parts of the piriform recess, respectively. Attempts to remove a foreign object also may damage the nerves.
14. With the head and cervical viscera reflected forward from the vertebral column, study the laryngopharynx from behind through the previously opened pharyngeal wall. It may be necessary to extend the midline incision in the posterior pharyngeal wall 4-5 cm inferiorly into the upper esophagus. Identify the epiglottis and aryepiglottic folds bounding the laryngeal aditus (Fig. 11).
15. Carefully incise and remove the mucous membrane of the piriform recess. Clean the internal laryngeal nerve entering the recess after piercing the thyrohyoid membrane (Fig. 11). If you have difficulty locating the nerve, re-position the head and neck for a lateral view and clamp the internal laryngeal nerve where it was previously dissected disappearing into the thyrohyoid membrane. Then turn back to a posterior view and find the clamped portion of the nerve as it enters the piriform recess. Be aware of the superior laryngeal artery accompanying the nerve but don’t attempt to dissect it.
16. Find the inferior laryngeal nerve ascending through the inferior part of the piriform recess. Is the small inferior laryngeal artery apparent running with the nerve? XXX
The larynx is the part of the respiratory system between the laryngopharynx above and the trachea below (Fig. 10; Gr 8.40B, 8.41; N63). It is located below the hyoid bone and anterior to the bodies of vertebrae C3-C6. The larynx is involved in voice production as well as in the passage of air to and from the lungs. It has a rigid cartilaginous skeleton to protect the patency of the airway; however, the larynx also has muscles that act as sphincters to appose mucosal folds, controlling air flow and preventing the entrance of foreign bodies.
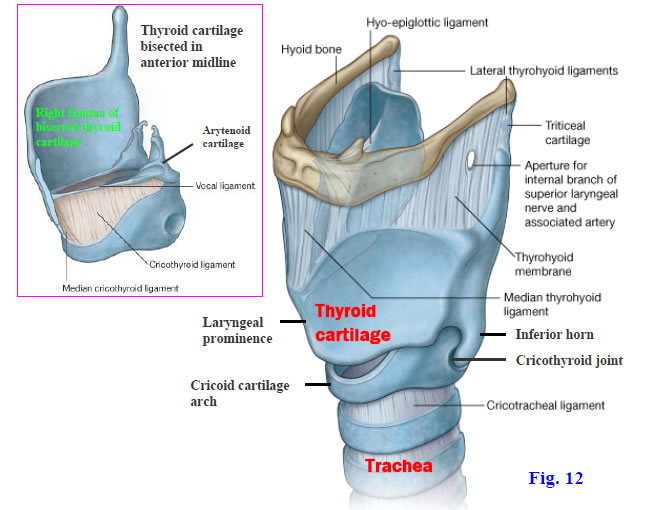
The laryngeal skeleton is formed by three large unpaired cartilages and by three pairs of smaller cartilages. The largest of the laryngeal cartilages is the thyroid cartilage, which is formed by two plate-like laminae fused in the anterior midline (Figs. 12, 13; Gr 8.33, 8.34, 8.37A & D; N77). The anterior fused portion of the thyroid cartilage forms a marked laryngeal prominence (“Adam’s apple”) in men due to the narrow (approx. 90°) angle between the laminae. The prominence is less in women due to the more obtuse (approx. 120°) angle at which the laminae meet. The other major implication of this difference in angulation is that the vocal folds (vocal cords) are longer in males, resulting in the deeper pitch of the male voice.
Short horns (cornua) extend superiorly and inferiorly from the posterior free edge of each thyroid lamina. The upper border and superior horn of each lamina are attached to the hyoid bone above by the thyrohyoid membrane (Fig. 12; Gr 8.16E, 8.33, 8.34, 8.37A; N68, 74, 77). This membrane was seen earlier as it was pierced by the internal laryngeal nerve and superior laryngeal artery. The inferior horns of the thyroid cartilage articulate with the sides of the cricoid cartilage below at synovial cricothyroid joints. The thyroid cartilage tilts forward and backward on the cricoid cartilage at the cricothyroid joints, changing the length of the vocal folds (N79).
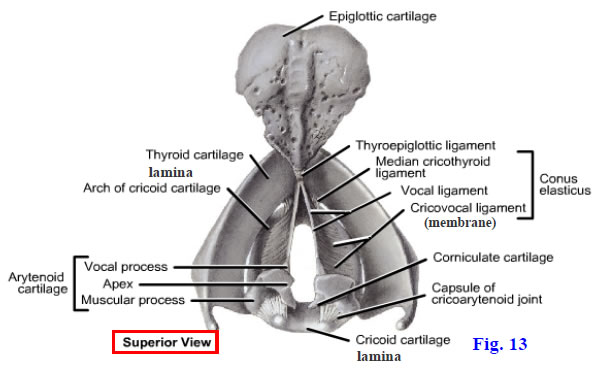
The cricoid cartilage is shaped like a signet ring with a broad posterior lamina and a narrow anterior arch (Figs. 12, 13; Gr 8.33, 8.34, 8.38C; N77, 78). It is attached inferiorly to the first tracheal ring by the cricotracheal ligament. The superior border of the cricoid arch gives attachment to the cricothyroid ligament (conus elasticus, cricovocal membrane) (Figs. 12 [inset], 13; Gr 8.16E, 8.36, 8.37D, 8.38C; N77, 78). The cricothyroid ligament (conus elasticus) ascends somewhat medially from the cricoid arch on its side of the body to end in a superior free border, the vocal ligament (Fig. 13) and will be discussed below.
The arytenoid cartilages are paired cartilages that are positioned laterally on the superior surface of the cricoid lamina (Figs. 12 [inset], 13; Gr 8.33A, 8.34A, 8.37A & D, 8.38C; N77, 78). Each is a three-side pyramid with an apex and a base. The base of each arytenoid cartilage forms a synovial joint with the cricoid cartilage (cricoarytenoid joint). Muscular and vocal processes project laterally and anteriorly, respectively, from the base of the arytenoid cartilage. The muscular process provides muscle attachments and the vocal process is the posterior attachment of the vocal ligament. The arytenoid, cricoid, and thyroid cartilages frequently ossify with age and become visible on x-rays.
The leaf-shaped epiglottic cartilage forms the elastic core of the epiglottis (Figs. 10, 11, 14B; Gr 8.36, 8.37, 8.38C, 8.40B, 8.41; N63, 66, 77). The epiglottis is located posterior to the root of the tongue and forms the upper part of the anterior wall of the laryngeal aditus. The epiglottic cartilage is anchored above to the hyoid bone by the hyoepiglottic ligament (Figs. 10, 12; Gr 8.37C, 8.38C; N63, 77) and below to the junction of the thyroid laminae by the short thyroepiglottic ligament (Fig. 13; Gr 8.37D; N77).
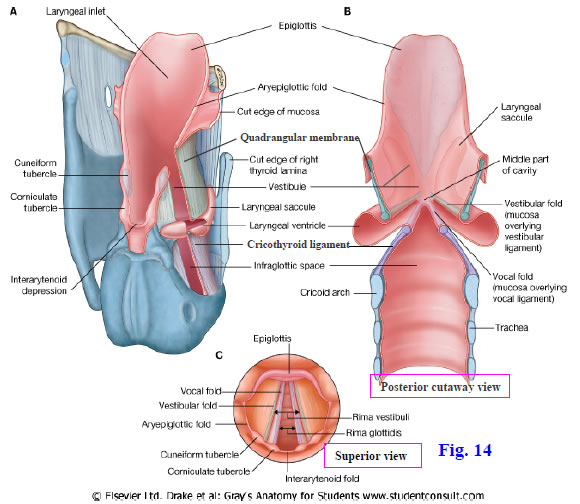
Two thin, submucosal fibroelastic membranes unite the laryngeal cartilages. They are the quadrangular membrane and the cricothyroid ligament. The quadrangular membrane connects the lateral aspects of the epiglottic and arytenoid cartilages (Fig. 14; Gr 8.36, 8.37A; N80 [Coronal section, unlabeled]). The upper free border of the quadrangular membrane is covered by mucous membrane to form the aryepiglottic fold, which helps bound the laryngeal inlet. The lower free border of the quadrangular membrane (vestibular ligament) and its covering mucosa form the vestibular fold (false vocal cord). The midline space in the laryngeal cavity between the two vestibular folds is the rima vestibuli (Fig. 14C).
The cricothyroid ligament, which is also called the “conus elasticus” and “cricovocal membrane,” extends superomedially from the cricoid arch (Figs. 12 [inset], 13, 14A-B; Gr 8.33B, 8.36, 8.37D, 8.38C; N77, 78, 80). It is thickened anteriorly in the midline where the two sides meet to form the median cricothyroid ligament, which is one site where an emergency airway is often made (cricothyrotomy, cricothyroidotomy) (e.g., http://www.surgeryencyclopedia.com/Ce-Fi/Cricothyroidotomy.html ). The free upper border of the cricothyroid ligament is also thickened between its posterior attachment to the vocal process of the arytenoid cartilage and its anterior attachment to the thyroid cartilage near the junction of the thyroid laminae. This upper free border is the vocal ligament, which is covered by mucosa to form the vocal fold (true vocal cord) (Fig. 14B-C; Gr 8.36; N80). The space in the laryngeal cavity between the two vocal folds is the rima glottidis. The vocal folds and rima glottidis together form the glottis.
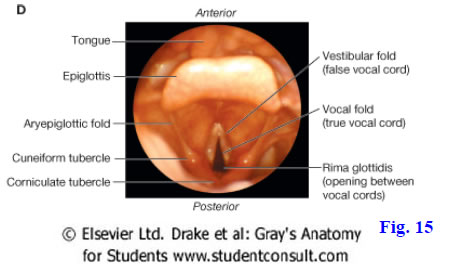
The small corniculate and cuneiform cartilages form small nodules in the posterior part of the aryepiglottic folds (N66, 78). The corniculate cartilage sits atop the apex of the arytenoid cartilage (N77), with which it articulates, and is a landmark in a superior view of the larynx during laryngoscopy (Figs. 14A & C, 15). The cuneiform cartilage is located anterior to the corniculate cartilage within the aryepiglottic fold. It does not articulate with other laryngeal cartilages.
17. Re-position the head and cervical viscera to their original positions against the vertebral column to examine the larynx from an anterior view. Again locate and palpate the hyoid bone. Identify its body and greater horns. Review the thyrohyoid membrane connecting the hyoid bone and thyroid cartilage. The thyrohyoid membrane may be partially hidden by the thyrohyoid muscles. The internal laryngeal nerve and superior laryngeal artery were previously seen piercing the membrane on each side.
18. Palpate the thyroid cartilage and verify that its two laminae fuse anteriorly in the midline. Compare the laryngeal prominence in a male cadaver with the wider angled union in a female cadaver. Palpate the arch of the cricoid cartilage and the midline fibroelastic tissue between the thyroid and cricoid cartilages. Realize that this median cricothyroid ligament is one place where an emergency airway can be created (cricothyrotomy). One member of the dissection team may want to attempt this procedure on the cadaver. Note the superior and inferior horns of the thyroid cartilage more laterally. Study the cricothyroid joints formed between the cricoid cartilage and the inferior horns of the thyroid cartilage. Identify the cricotracheal ligament, which attaches the arch of the cricoid cartilage to the first tracheal cartilage.
19. Pull the head and cervical viscera forward to examine the larynx from a posterior view. At the anterior margin of the laryngeal aditus find the epiglottis. Be aware of, but don’t attempt to clean, the hyoepiglottic ligament. Trace the aryepiglottic folds at the lateral margins of the laryngeal aditus as they pass from the epiglottic cartilage to the arytenoid cartilages. The arytenoid cartilages are hidden by mucous membrane and muscles at this time but can be palpated as a large pyramidal mass atop the cricoid lamina on each side. In the posterior margin of the aryepiglottic folds palpate the small nodules of the corniculate and cuneiform cartilages. These raise the overlying mucous membrane as corniculate and cuneiform tubercles visible during laryngoscopy (Fig. 15). XXX
The laryngeal muscles include both extrinsic and intrinsic groups. The extrinsic laryngeal muscles have an attachment outside the larynx and include the infrahyoid and suprahyoid muscles. The infrahyoid muscles are the sternohyoid, omohyoid, sternothyroid, and thyrohyoid (Gr 8.9, 8.10A, 8.16A-C; N26-28). In general, the infrahyoid muscles depress the hyoid bone and larynx or stabilize the hyoid bone in position from below. The thyrohyoid muscle is an exception among infrahyoid muscles in that it raises the larynx toward the hyoid bone.
The suprahyoid muscles elevate the hyoid bone and larynx. They are the digastric, stylohyoid, mylohyoid, and geniohyoid muscles (Gr 8.9, 8.10A, 8.11, 8.13A, 8.15, 8.16A; N26-28, 53). The longitudinal pharyngeal muscles (e.g., stylopharyngeus) perform the same action as they elevate the pharynx during swallowing.
The intrinsic laryngeal muscles change the length and tension of the vocal folds, control the degree of separation between the vocal and vestibular folds of the two sides, or otherwise act as sphincters to prevent the entrance of foreign objects into the larynx. The main muscles that increase tension on the vocal folds are the cricothyroid muscles, which run posteriorly and superiorly from the arch of the cricoid cartilage to attach to the inferior surface of the lamina and the inferior horn of the thyroid cartilage (Gr 8.16C & E, 8.21, 8.38A, Table 8.8 [p. 784]; N68, 78-80). The cricothyroid muscles tilt the thyroid cartilage forward on the cricoid cartilage at the cricothyroid joints (N79). They are innervated by the external laryngeal nerves, being the only intrinsic laryngeal muscles not innervated by the recurrent laryngeal nerves (X).
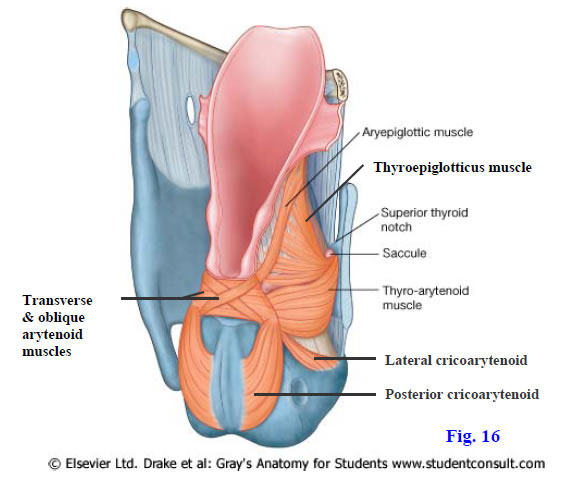
The only abductors of the vocal folds are the posterior cricoarytenoid muscles (Fig. 16; Gr 8.29B, Table 8.8 [pp. 784-785]; N78, 79). Each posterior cricoarytenoid ascends anteriorly from the posterior surface of the cricoid lamina to the muscular process of the arytenoid cartilage of the same side, so that the muscle’s contraction rotates the arytenoid cartilage laterally around a vertical axis. This abducts the vocal fold to widen the rima glottidis.
Adductors of the vocal folds include the lateral cricoarytenoid, transverse arytenoid, and oblique arytenoid muscles (Fig. 16; Gr Table 8.8 [pp. 784-785]; N78, 79). Each lateral cricoarytenoid muscle ascends posteriorly from the superior surface of the cricoid arch to the muscular process of the arytenoid cartilage on its side. It rotates the arytenoid cartilage medially around a vertical axis so that the vocal fold moves toward the midline (N79). The transverse and oblique arytenoid muscles pull the two arytenoid cartilages toward each other, narrowing the rima glottidis. In adducting the vocal folds, these muscles also serve as sphincters to protect the airway.
Other muscles contribute to sphincteric actions of more superior portions of the larynx. The thyroarytenoid muscle passes from the deep surface of the thyroid lamina to the lateral border of the arytenoid cartilage. It draws the arytenoid cartilage toward the thyroid cartilage (Fig. 16; Gr Table 8.8 [pp. 784-785]; N78, 79). It also pushes the quadrangular membrane and overlying mucosa medially to form a sphincter for the vestibule of the laryngeal cavity. The upper fibers of the thyroarytenoid muscle ascend to the epiglottic cartilage as the thyroepiglotticus muscle. The aryepiglottic muscles are continuous with the oblique arytenoid muscles. The aryepiglottic muscles pull the arytenoid cartilages toward the epiglottic cartilage to narrow the laryngeal aditus in an anteroposterior direction and also draw the aryepiglottic folds toward each other to narrow the width of the inlet.
The vocalis muscle lies between the thyroarytenoid muscle and the vocal ligament, to which it attaches (Gr 8.38C; N78). Some authors consider the vocalis to be the medial part of the thyroarytenoid. The vocalis muscle makes minute adjustments in the tension of the vocal ligaments during speech.20. Turning to an anterior view of the cervical viscera, review the extrinsic muscles of the larynx. Identify the sternohyoid, omohyoid, sternothyroid, and thyrohyoid muscles, or their attachments if the muscles have been cut.
21. Clean the cricothyroid muscle of one side and find the external laryngeal nerve innervating it. To study the other intrinsic muscles of the larynx, pull the head and cervical viscera forward to expose the posterior wall of the larynx. If the mucous membrane over the lamina of the cricoid cartilage and the arytenoid cartilages is still intact, carefully remove it at this time. Clean the transverse and oblique arytenoid muscles passing between the two arytenoid cartilages. Follow the slender oblique arytenoid muscle into the aryepiglottic fold of one side, where it becomes the aryepiglotticus muscle.
22. Clean the posterior cricoarytenoid muscles and follow the muscle of the right side superolaterally to its attachment on the muscular process of the right arytenoid cartilage. Realize that the posterior cricoarytenoids are the only muscles that can ABduct the vocal folds.
23. Disarticulate the right cricothyroid joint. Use a scalpel to make a vertical cut through the right lamina of the thyroid cartilage near the anterior midline and remove the lamina. To do this you will have to remove part of the right half of the thyrohyoid membrane and the right cricothyroid muscle. If the thyroid cartilage is ossified, as frequently occurs in middle age, you may have to use bone shears to cut it. Clean the lateral cricoarytenoid muscle ascending posteriorly from the arch of the cricoid cartilage to the muscular process of the arytenoid cartilage. Superior to the lateral cricoarytenoid, and sometimes indistinctly separated from it, find the thyroarytenoid muscle. Realize that its most medial fibers attach to the vocal ligament as the vocalis muscle, but don’t attempt to demonstrate this. Look for the upper fibers of the thyroarytenoid ascending to the epiglottic cartilage as the thyroepiglotticus muscle. XXX
The cricothyroid muscles are innervated by the external laryngeal nerves (X), which are branches of the superior laryngeal nerves. All of the other intrinsic muscles of the larynx are innervated by the recurrent laryngeal nerves (X) (Gr 8.16E, 8.21, 8.35, 8.38A, Table 8.8 [pp. 784-785]; N71, 76, 80). Injury to the external laryngeal nerve, which may occur during thyroidectomy due to its close relationship to the superior thyroid artery, results in a monotonous voice that tires easily. A lesion of one recurrent laryngeal nerve results in unilateral vocal cord paralysis so that the vocal folds are unable to meet in the midline, producing a hoarse, breathy, easily fatigable voice. Since the left recurrent laryngeal nerve has an intrathoracic course as well as a cervical one, it is more commonly involved in lesions than the right recurrent laryngeal nerve. Frequent causes of lesions are surgical iatrogenic injury and malignant invasion. Re-innervation surgery may be performed (e.g., see http://archotol.ama-assn.org/cgi/content/full/127/10/1211 ). Alternatively, the vocal fold may be injected with a material to cause its medialization, or the arytenoid cartilage may be repositioned. The vocal folds may not fully appose in geriatric patients due to degenerative changes in the folds and muscular atrophy.
Bilateral vocal fold paralysis results in a variable loss of voice. More importantly it results in airway compromise, ranging in severity from immediately life-threatening to largely unnoticeable. A tracheostomy may be performed or the rima glottidis may be surgically widened ( http://www.emedicine.com/Ent/topic348.htm ).
Sensory innervation of the laryngeal mucosa is from the internal laryngeal and recurrent laryngeal nerves. The internal laryngeal nerve branches from the superior laryngeal nerve and pierces the thyrohyoid membrane to enter the piriform recess, which it supplies. It also supplies the mucous membrane of the larynx superior to the vocal folds and is the afferent limb of the cough reflex to expel foreign objects that enter the vestibule. The density of sensory innervation is greatest at the laryngeal inlet. The recurrent laryngeal nerve (actually its inferior laryngeal continuation) innervates the laryngeal mucosa inferior to the vocal folds.
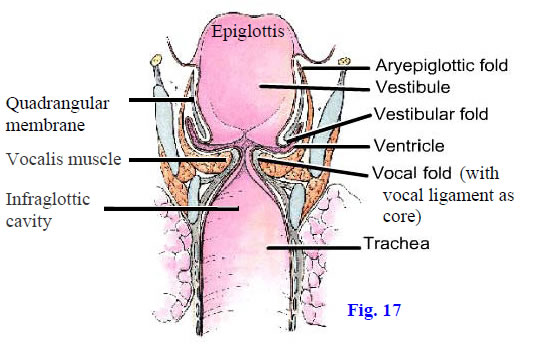
The laryngeal cavity extends from the laryngeal inlet (aditus) to the inferior border of the cricoid cartilage. It communicates above with the laryngopharynx at the aditus and is continuous below with the trachea (Figs. 10, 14B, 17; Gr 8.40B, 8.41; N63, 66). The laryngeal cavity is subdivided into three regions by the vestibular and vocal folds: the vestibule, ventricle, and infraglottic cavity. The vestibule is the part of the cavity between the laryngeal inlet and the vestibular folds. It is lined by mucous membrane richly innervated by the internal laryngeal nerves so that contact with an aspirated foreign object results in the reflex spasm of laryngeal muscles to close the rima vestibuli and rima glottidis, preventing the object from entering the trachea. There is also vigorous reflex coughing to expel the object. Some drowning victims succumb to laryngospasm rather than to the actual entry of water into the lungs ( http://www.emedicine.com/emerg/topic744.htm ).
The ventricle extends laterally between the vestibular and vocal folds from the middle part of the laryngeal cavity (Fig. 14A-B; Gr 8.36, 8.38C, 8.40; N80 [unlabeled]). The ventricle is a lateral recess with a blind pocket anterosuperiorly, the laryngeal saccule (Figs. 14A, 16). The ventricle and saccule’s mucous glands lubricate the vocal folds. The saccule occasionally projects above the superior edge of the thyroid cartilage lamina to protrude the thyrohyoid membrane (laryngocele) (Gr 8.38A-B).
The infraglottic cavity is the portion of the laryngeal cavity below the vocal folds (Figs. 14A-B, 17). It is continuous with the lumen of the trachea at the inferior border of the cricoid cartilage. An incision through the median cricothyroid ligament (or a needle inserted there) to create an emergency airway (cricothyrotomy, cricothyroidotomy) enters the infraglottic cavity below an obstruction at the level of the vocal folds (e.g., due to laryngospasm or edema from an allergic reaction).
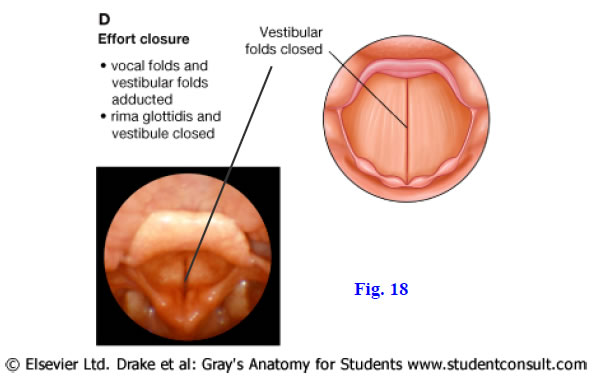
The vestibular fold (false vocal cord) is formed by mucous membrane covering the vestibular ligament, which is the thickened inferior free edge of the quadrangular membrane (Figs. 14B-C, 17; Gr 8.36; N80). The midline space between the two vestibular folds is the rima vestibuli. The vestibular folds are protective in function and play little or no role in speech. They can be tightly adducted, closing the rima vestibuli, to prevent further incursion by a foreign object that has entered the vestibule (Fig. 18).
The vocal fold (true vocal cord) is formed by mucous membrane covering the vocal ligament, which is the thickened superior free edge of the cricothyroid ligament (Figs. 14B-C, 17; Gr 8.36, 8.37D, 8.38C; N63, 80). The midline space between the vocal folds is the rima glottidis (Figs. 14B-C, 15), which is narrower than the rima vestibuli. It varies in shape according to the position of the vocal ligaments. The vocal folds and rima glottidis together form the glottis.
The vocal folds protect the airway and function in phonation. Variations in the length, tension, and proximity of the vocal folds change the sounds produced during vocal fold vibrations by expired air. The fundamental tone produced at the larynx is modified by resonating chambers in the upper respiratory and digestive tracts.
The vestibular folds and vocal folds act together to close the airway during a forced expiratory effort in the Valsalva maneuver, which is used during coughing, straining during bowel movements, weight lifting, etc. The strong contractions of anterolateral abdominal muscles result in increased intraabdominal pressure, which is passively transmitted into increased intrathoracic pressure through the relaxed diaphragm. Because the increased intrathoracic pressure resulting from the Valsalva maneuver impedes venous return and puts a strain on the heart, elderly and cardiac patients are usually counseled to avoid it whenever possible. The maneuver is sometimes used as an intervention to resolve supraventricular tachycardias.
The life-saving Heimlich maneuver is sudden vigorous external compression of the abdomen to eject a foreign object from an obstructed airway. The sudden increase in intraabdominal pressure throws the diaphragm upward, increasing intrathoracic pressure and expelling air from the trachea through the larynx. This often dislodges the obstructing foreign object.24. Look into the laryngeal cavity through the laryngeal aditus and identify the vestibular and vocal folds. Using large scissors open the larynx in the posterior midline, cutting downward from the aditus between the arytenoid cartilages and through the lamina of the cricoid cartilage into the upper trachea. If the cricoid cartilage is calcified, use bone shears to cut the lamina. Spread the cut edges apart as you would open a book. Identify the vestibular and vocal folds from this view and use a probe to explore the intervening ventricle.
25. Carefully remove the mucous membrane between the aryepiglottic and vestibular folds on one side to expose the thin quadrangular membrane (Figs. 14B, 17; Gr 8.36). Clean the inferior free edge of the quadrangular membrane, which forms the vestibular ligament, the core of the vestibular fold. Carefully remove the mucosa inferior to the vocal fold on the same side of the body to expose the cricothyroid ligament. Clean the upper free edge of the cricothyroid ligament, the vocal ligament, which forms the core of the vocal fold. Verify that the vocal ligament attaches near the junction of the thyroid cartilage laminae anteriorly and to the vocal process of the arytenoid cartilage posteriorly. XXX
The illustrations in this dissection guide are used with permission from Gray’s Anatomy for Students. 2005, by Richard Drake, Wayne Vogel, and Adam Mitchell, Elsevier Inc., Philadelphia; and from Grant’s Atlas of Anatomy, 11E, 2005, Anne Agur and Arthur Dalley II, Lippincott Williams & Wilkins, Philadelphia.